Volume 4, Issue 12
December 2024
Prevalence and Factors Related to Urinary Incontinence in the Elderly: A Systematic Review
Mohammed Hashim Alaish, Ali Naji AlNihab, Ali Hussain Al-Shehab, Ashraf Hassan Al Awani, Abdul-moneem Mohammed Al-aman, Mansoor Mohammed Alrebeh
DOI: http://dx.doi.org/10.52533/JOHS.2024.41218
Keywords: urinary incontinence, elderly, prevalence, risk factor, UI
Urinary incontinence (UI) is a prevalent condition among the elderly, affecting approximately 30%-50% of individuals over 65 years old. Understanding the prevalence of UI and its associated risk factors is crucial for improving management and treatment strategies. This systematic review aims to synthesize existing literature on the prevalence of UI and identify significant risk factors influencing its occurrence in diverse populations. A comprehensive literature search was conducted across multiple databases, including PubMed, Scopus, the Cochrane Library, and Web of Science, for studies published after 2014. Studies were included if they reported the prevalence of UI and associated risk factors in elderly populations. Data extraction focused on overall prevalence rates, demographic information, and specific risk factors along with their respective odds ratios or risk ratios, or prevalence ratios, confidence intervals, and p-values. The methodological quality of the included studies was assessed using the Newcastle-Ottawa Scale tool. A total of 12 studies met the inclusion criteria, revealing a wide prevalence range of UI from 14.2% to 82.9%. Gender-specific prevalence shows that among men, rates can be as low as 20% (monthly UI) and as high as 35.96%, while women exhibit prevalence rates from 15% to 66.1%. Significant risk factors identified include female sex, increased body mass index, history of cancer, diabetes, cognitive impairment, and mobility limitations. The odds ratios for these factors varied, indicating a robust association with the occurrence of UI across different populations. The findings of this systematic review underscore the high prevalence of UI incontinence and its multifactorial nature, emphasizing the need for targeted screening and intervention strategies. Increased awareness among healthcare professionals about the significant risk factors associated with UI can facilitate early identification and improve patient outcomes, ultimately enhancing the quality of life for those affected.
Introduction
Urinary incontinence (UI) is a prevalent geriatric syndrome that has far-reaching impacts on the elderly, affecting them both physically and socially. Characterized by the involuntary leakage of urine, UI is a condition that significantly burdens individuals over the age of 65. Current estimates suggest that approximately 30-50% of older adults experience some form of UI, highlighting its widespread nature and the considerable physical, psychological, and economic challenges it poses. The implications of UI extend beyond the immediate discomfort of leakage, encompassing a range of issues including high treatment costs, caregiver strain, and the exacerbation of skin and hygiene problems. Socially, UI can lead to profound isolation, diminished self-esteem, and depression, further compounding the difficulties faced by affected individuals (1).
UI often coexists with other health issues, making its management even more complex. It is frequently associated with conditions such as dementia, urinary tract infections, and both physical and cognitive impairments (2, 3). The prevalence of UI varies across different studies and populations, reflecting a diversity of experiences and challenges. For instance, a study conducted in São Paulo, Brazil, identified a 38.4% prevalence of UI among individuals aged 65 and older, with women being disproportionately affected compared to men (50% vs. 18.3%) (4). Among women over the age of 50, the prevalence of UI ranges from 26.2% to 52.3%, illustrating the significant variation and highlighting the gender disparities in the incidence of this condition (5, 6).
The risk factors contributing to UI are multifaceted and include a combination of physiological, behavioral, and medical conditions. Advanced age is a major factor, but other elements such as a history of cardiovascular disease, low physical activity levels, obesity, smoking, and limitations in functional health also play critical roles. Psycho-social factors, diabetes, chronic cough, bowel issues, and prior urinary tract surgeries further complicate the risk profile. For women, additional risk factors include urogenital infections, vaginal deliveries, higher parity, incontinence following childbirth, urogynecological surgery, menopause, and hormone replacement therapy (7-9). These factors collectively contribute to the development and severity of UI, but research comparing these risk factors between men and women is still limited. Much of the existing research has focused on clinical populations, leaving gaps in understanding the general population's experiences with UI.
Given the substantial impact of UI on the elderly population, a thorough understanding of the condition and its management is essential. This systematic review aims to provide an overview of the prevalence of urinary incontinence among older adults, exploring the various factors that contribute to its development.
Methodology
The systematic review adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Definition of Outcomes and Inclusion Criteria
The primary outcome of this systematic review was the prevalence of urinary incontinence (UI) in elderly populations, defined as the involuntary loss of urine. UI was further categorized into three types: stress urinary incontinence (SUI), urge urinary incontinence (UUI), and mixed urinary incontinence (MUI), as described in the included studies. Secondary outcomes focused on factors associated with UI, including demographic variables, clinical variables, and functional factors.
Studies that reported the prevalence of UI and associated factors in individuals aged 65 years and older were considered for inclusion. Eligible studies were original research articles published in peer-reviewed journals, written in English, and focused on elderly populations. The study designs included cross-sectional, cohort, and case-control studies that identified risk factors for UI. Additionally, only studies that provided relevant outcomes such as prevalence rates and associated risk factors, including the reporting of odds ratios (OR), relative risks (RR), or prevalence ratios (PR) with 95% confidence intervals (CI), were included.
Search Strategy
A comprehensive literature search was conducted using multiple databases, including PubMed, Scopus, Cochrane Library and Web of Science, covering publications from 2014 to September 2024. The search utilized a combination of medical subject headings (MeSH) and keywords related to "urinary incontinence," "elderly," "prevalence," and "risk factors," with Boolean operators such as AND, OR, and NOT to refine the results. Specific terms included “Urinary incontinence,” “Elderly” or “Older adults” or “Aging population,” “Prevalence” or “Epidemiology,” and “Risk factors” or “Determinants” or “Predictors.” Additionally, the references of included articles and relevant reviews were manually checked to identify further studies not captured by the database search. To maintain a focus on peer-reviewed data, grey literature and conference abstracts were excluded.
Quality Assessment
The methodological quality of the included studies was evaluated using the Newcastle-Ottawa Scale (NOS), which is designed for observational studies. This scale assesses studies based on three primary criteria: selection of study groups, comparability of groups, and outcome assessment. Each study was assigned a score ranging from 0 to 9 stars, with a score of 6 or higher indicating high quality. The assessment focused on specific criteria, including the representativeness of the exposed cohort, selection of the non-exposed cohort, ascertainment of exposure, and confirmation that the outcome was absent at the study's outset. Comparability was evaluated by examining the control of confounders, such as age, gender, and comorbidities. For outcome assessment, the method used to determine urinary incontinence (UI), the duration of follow-up, and the adequacy of follow-up for cohort studies were considered. Any disagreements between reviewers regarding quality assessments were resolved by consensus or discussion with a third reviewer, ensuring a robust quality evaluation. Only studies meeting the predefined quality threshold were included in the final analysis.
Results
Search Results
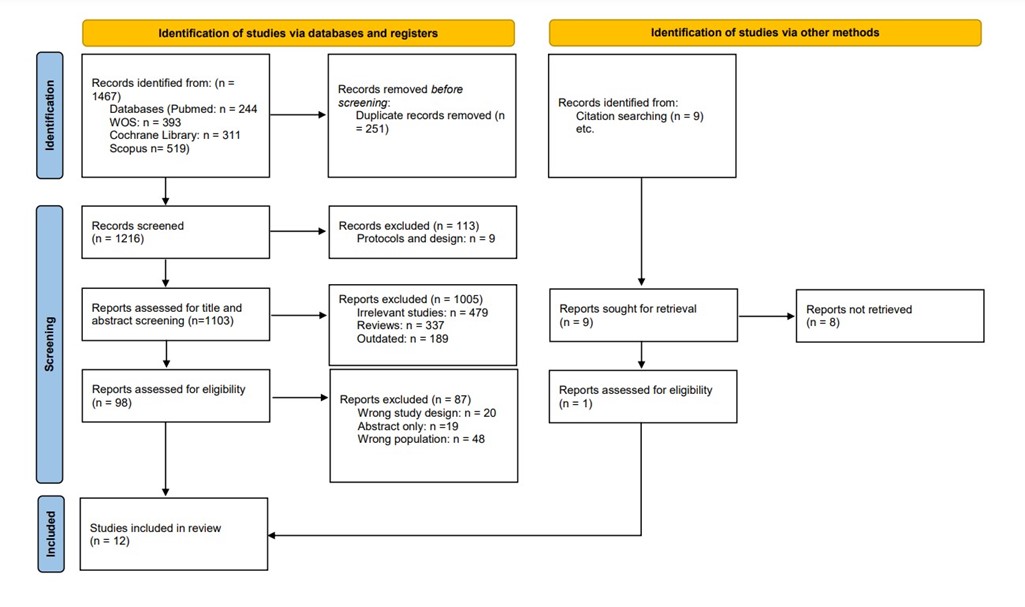
We executed the search methodologies outlined previously, resulting in the identification of a total of 1467 citations, subsequently reduced to 1216 following the removal of duplicates. Upon screening titles and abstracts, only 98 citations met the eligibility criteria for further consideration. Through full-text screening, this number was further refined to 12 articles (10-21) aligning with our inclusion and exclusion criteria. Figure 1 provides an in-depth depiction of the search strategy and screening process.
Results of Quality Assessment
The quality of the included studies was assessed using the Newcastle-Ottawa Scale for both cohort and cross-sectional designs. For the cohort studies, most were rated as "Good" quality, with strong performance in areas such as cohort representativeness, exposure ascertainment, and outcome assessment. However, some limitations were noted, particularly in follow-up duration and controlling for loss to follow-up, which resulted in one study being rated as "Satisfactory" (Table 1).
For cross-sectional studies, the majority also demonstrated "Good" quality, with high scores in sample representativeness, sample size, and outcome assessment. Most studies adequately controlled for confounding factors and used appropriate statistical tests. A few studies had minor shortcomings, such as limited control of confounders or weaker outcome ascertainment, but overall, the quality of the evidence was strong, providing reliable findings for this review. These limitations should be kept in mind when interpreting the results (Table 2).

Figure 1: PRISMA flowchart
|
Table 1: Quality Assessment of Included Cohort Studies Using the Newcastle-Ottawa Scale |
||||||||||
|
Study |
Selection |
Comparability |
Outcome |
|||||||
|
Representativeness of exposed cohort |
Selection of non- exposed cohort |
Ascertainment of exposure |
Demonstration of that outcome of interest was not present at the start of the study |
Adjust for the most important risk factors |
Adjust for other risk factors |
Assessment of outcome |
Follow-up length |
Loss to follow-up rate |
Quality |
|
|
Tsui et al 2018 (12) |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
0 |
1 |
Good |
|
Tamanini et al 2018 (13) |
0 |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
Good |
|
Chen et al 2023 (21) |
1 |
1 |
1 |
0 |
1 |
1 |
1 |
0 |
0 |
Satisfactory |
Characteristics of the included studies
The baseline characteristics of the included studies in this systematic review reflect a diverse range of geographical regions and study designs, with most being cross-sectional. Sample sizes varied greatly, from as few as 68 participants to over 200,000 in some large cohort studies. The average age of participants ranged from 66 to 87 years, covering a wide spectrum of elderly populations. Gender distribution also showed variability, with some studies including both males and females, while others focused exclusively on one gender (Table 3).
Study outcome measures
The prevalence of UI varies widely, with reported rates ranging from 14.2% to 82.9% across different studies and populations. Gender-specific prevalence shows that among men, rates can be as low as 20% (monthly UI) and as high as 35.96%, while women exhibit prevalence rates from 15% to 66.1% (Table 4).
|
Table 2: Quality Assessment of Included Cross Sectional Studies Using the Newcastle-Ottawa Scale |
|||||||||
|
Study |
Selection |
Comparability |
Outcome |
||||||
|
Representativeness of the sample |
Sample size |
Non respondents |
Ascertainment of exposure |
Confounding Factors controlled |
Assessment of outcome |
Statistical test |
Quality score |
Quality |
|
|
Chiu et al 2015 (10) |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
7 |
Good |
|
Jerez-Roig et al 2016 (11) |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
7 |
Good |
|
Baeur et al 2019 (14) |
1 |
1 |
1 |
1 |
1 |
2 |
1 |
8 |
Good |
|
Erdogan et al 2019 (15) |
1 |
1 |
1 |
1 |
1 |
2 |
1 |
8 |
Good |
|
Bozdar et al 2021 (16) |
1 |
1 |
1 |
0 |
2 |
0 |
1 |
6 |
Good |
|
Northwood et al 2021 (17) |
1 |
1 |
1 |
1 |
2 |
1 |
1 |
8 |
Good |
|
Suzuki et al 2021 (18) |
1 |
1 |
1 |
1 |
2 |
1 |
1 |
8 |
Good |
|
Tai et al 2021 (19) |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
7 |
Good |
|
Godayol et al 2022 (20) |
1 |
1 |
1 |
1 |
1 |
1 |
1 |
7 |
Good |
The analysis of risk factors associated with UI across multiple studies highlights various demographic, clinical, and functional variables as significant contributors. Chiu et al. (10) identified that poor performance in mobility and flexibility tests, such as the 8-ft up-and-go test and chair sit-and-reach test, was significantly associated with UI, with risk factors demonstrating OR ranging from 1.01 to 1.16, and p-values below 0.05, indicating a strong link between impaired physical function and UI. Tsui et al. (12) emphasized the role of gender, with females having a higher likelihood of UI, reflected by an OR of 4.12 (95% CI 2.49–6.82, p ≤ 0.01). Other significant risk factors identified were co-existing stress urinary incontinence (SUI) and conditions such as stroke or transient ischemic attack (TIA), as well as increased body mass index (BMI), with ORs ranging from 1.19 to 1.99 and p-values below 0.05, illustrating how comorbidities and obesity exacerbate UI risk. In a study by Tamanini et al. (13), sex-specific factors emerged, where a history of cancer and diabetes in women were associated with increased UI risk (OR = 2.66 and 1.70, respectively), while men reporting impaired activities of daily living (ADL) and "fair" self-reported health showed heightened odds of UI (OR = 9.25 and 2.33, respectively). These findings underscore the sex-specific pathways that influence UI, particularly chronic disease history and physical function. Bauer et al. (14) demonstrated that BMI and fat mass were significant predictors of UI in men, with higher BMI linked to increased odds (OR = 1.36, p < 0.05), while better muscle function, including higher grip strength and quadriceps strength relative to BMI, was associated with reduced UI risk (OR = 0.82–0.77, p < 0.05). These findings emphasize the role of muscle mass and body composition in UI risk among males. Similarly, Erdogan et al. (15) found sarcopenia, defined by low muscle mass adjusted by weight or BMI, to be a significant risk factor, with ORs of 1.465 to 1.971 (p < 0.05), further highlighting the connection between muscle function and UI risk.
|
Table 3: Baseline Characteristics of Included Studies |
|||||||
|
Author |
Country |
Study type |
Year of publication |
Study period |
Total Sample size |
Age(yrs) Mean± SD (Years) |
Gender F/M % |
|
Chiu et al (10) |
Taiwan |
Cross sectional |
2015 |
2011 |
77 |
78.7±8.0 |
43.5/32.7 |
|
Jerez-Roig et al (11) |
Brazil |
Cross-sectional |
2016 |
October and December 2013 |
321 |
81.5± 9 |
75.4/24.6 |
|
Tsui et al (12) |
England, Scotland and Wales |
Longitudinal Cohort |
2018 |
March 1946 1 week and 2014-2015 |
1762 |
68 |
- |
|
Taminini et al (13) |
Brazil |
Cross-sectional |
2018 |
2000- cohort A 2006 cohort b 2010 and 2011 -follow up |
1413 |
74.5 ±9.3 |
61.8/38.2 |
|
Bauer et al (14) |
San Francisco, CA |
Prospective cohort study |
2019 |
- |
1298 men |
73.7± 3 |
NA/100 |
|
Erdogan et al (15) |
Turkey |
Retrospective Cross-sectional |
2019 |
November 2012 and November 2016 |
802 females |
74.4 ±7.3 |
100/NA |
|
Bozdar et al (16) |
Khairpur Mirs |
Prospective cross-sectional |
2021 |
1st December 2014 to 31st December 2016 |
310 |
71.49±7.01 |
59.7/40.3 |
|
Northwood et al (17) |
Canada |
Cross-sectional |
2021 |
2011-2016 |
118,519 |
80.7 ±7.81 |
57.6 /42.4 |
|
Suzuki et al (18) |
Japan |
Cross-sectional epidemiological |
2021 |
15 October 2015 to 16 November 2015 |
4881 |
87.0 ± 7.5 |
80.9/19.1 |
|
Tai et al (19) |
China |
Institution-based cross-sectional |
2021 |
June to December 2018 |
551 |
84.16 ±4.84 |
67/33 |
|
Godayol et al (20) |
Spain |
Observational cross-sectional |
2022 |
January 2020 - March 2020 |
68 |
83.6 ±7.6 |
80.9/19.1 |
|
Chen et al (21) |
US, UK, and Europe |
Prospective longitudinal cohorts |
2023 |
2004-2018 |
HRS 207,805 ELSA 98,158 SHARE 360,800 200,717 participants |
HRS 66 ELSA 67 SHARE 64 |
HRS 55.74/44.25 ELSA 54.32/45.67 SHARE 55.09/44.90 |
HRS: Health and Retirement Study; ELSA: English Longitudinal Study of Ageing; SHARE: Survey of Health, Ageing, and Retirement in Europe; NA: not applicable.
|
Table 4: Prevalence and Risk Factors Associated With the Occurrence of UI |
||
|
Study |
Overall Prevalence of UI (%) |
Significant Risk Factors and Associations |
|
Chiu et al (10) |
35.90% |
8-ft up-and-go test: 1.16 (1.03–1.31), p = 0.018; Chair sit-and-reach test (Right): 1.01 (0.85–0.99), p = 0.018; Chair sit-and-reach test (Left): 0.91 (0.85–0.99), p = 0.018 |
|
Jerez-Roig et al (11) |
58.88% |
White race: 1.39 (1.10–1.76), p = 0.005; Physical inactivity: 1.97 (1.20–3.22), p = 0.007; Stroke: 1.61 (1.17–2.21), p = 0.003; Mobility impairment: 1.36 (1.02–1.81), p = 0.034; Cognitive decline: 1.48 (1.11–1.98), p = 0.008 |
|
Tsui et al (12) |
Overall, 35.96%;15% (men); 54% (women) |
Female sex: 4.12 (2.49–6.82), p ≤ 0.01; Co-presentation of SUI: 1.80 (1.36–2.37), p ≤ 0.01; Stroke/TIA: 1.99 (1.14–3.49), p < 0.01; Increased BMI: 1.19 (1.05–1.34), p = 0.01 |
|
Tamanini et al (13) |
14.2% (men) |
Women: History of cancer: 2.66 (1.33–5.31), p = 0.006; Diabetes: 1.70 (1.03–2.80), p = 0.037 |
|
28.2% (women) |
Men: IADL category 5-8: 9.25 (1.50–57.18), p = 0.017; "Fair" self-reported health: 2.33 (1.14–4.78), p = 0.021 |
|
|
Bauer et al (14) |
Men: 20% (monthly UI), 11% (weekly UI) |
Higher BMI: 1.36 (1.16–1.63), p < 0.05; Fat mass: 1.16 (1.01–1.33), p < 0.05; Lower ALM/BMI: 0.81 (0.69–0.95), p < 0.05; Grip strength/BMI: 0.82 (0.70–0.95), p < 0.05; Quadriceps strength/BMI: 0.77 (0.66–0.90), p < 0.05 |
|
Erdogan et al (15) |
48.90% |
Sarcopenia (weight adjusted): 1.465 (1.029-2.085), p = 0.034; LMM (muscle mass adjusted by weight): 1.819 (1.315–2.515), p < 0.001; LMM (muscle mass adjusted by BMI): 1.971 (1.369–2.838), p < 0.001 |
|
Bozdar et al (16) |
23.90% |
Female: 2.06 (1.01-4.17), p = 0.046; Urban residents: 4.67 (2.41-9.304), p < 0.001; Retired: 0.18 (0.08-0.38), p < 0.001; Hypertension: 4.29 (1.89-9.71), p < 0.001; DM: 4.36 (2.06-9.26), p < 0.001 |
|
Northwood et al (17) |
33.70% |
Impaired ADL function: 5.31 (5.14, 5.50), p < 0.05; Cognitive impairment: 2.37 (2.28, 2.47), p < 0.05; Female sex: 1.87 (1.82, 1.93), p < 0.05; Multiple chronic conditions: 1.83 (1.74, 1.93), p < 0.05; Presence of a distressed caregiver: 1.31 (1.27, 1.35), p < 0.05; Economic trade-off: 1.23 (1.11, 1.34), p < 0.05; Falls: 1.22 (1.19, 1.26), p < 0.05 |
|
Suzuki et al (18) |
82.90% |
Age: 1.023 (1.011–1.036), p < 0.05; Care-Needs level: 1.149 (1.041–1.267), p < 0.05; Loss of voiding desire: 7.256 (5.286–9.987), p < 0.05; Fecal incontinence: 1.372 (0.927–2.031), p < 0.05 |
|
Tai, H et al (19) |
24.30% |
Constipation: 1.62 (1.03, 2.55); p= 0.0381; Immobility: 13.13(4.44, 38.80); p<0.001; Wheelchair use: 6.58 (2.70, 16.03); p= <0.001; Cardiovascular Disease (CVD): 2.15 (1.34, 3.43); p=0.001; Pelvic or spinal surgery: 2.02(1.31,3.12); p=0.001; |
|
Godayol et al (20) |
66.10% |
Frailty: PR = 1.84 (0.96–3.53), p = 0.003; Faecal Incontinence: PR = 1.65 (1.01–2.65), p = 0.006; Anxiety: PR = 1.64 (1.01–2.66), p = 0.014; Physical Performance: PR = 1.77 (1.00–3.11), p = 0.018; Cognitive State: PR = 1.95 (1.05–3.60), p = 0.032 |
|
Chen et al (21) |
19.14% |
Among female: BMI; WC |
UI: Urinary Incontinence; SUI: Stress Urinary Incontinence; BMI: Body Mass Index; TIA: Transient Ischemic Attack; ALM: Appendicular Lean Mass; IADL: Instrumental Activities of Daily Living; LMM: Low Muscle Mass; PR: Prevalence Ratio; OR: Odds Ratio; CI: Confidence Interval; ADL: Activities of Daily Living; NR: Not Reported; WC: Waist Circumference; CVD: Cardiovascular Disease.
This study reinforces the importance of assessing muscle mass in evaluating UI risk, particularly in populations with decreased mobility or muscle strength. Bozdar et al. (16) reported that female sex, living in urban areas, and chronic diseases such as hypertension and diabetes were significantly associated with increased UI risk, with ORs ranging from 2.06 to 4.67 (p < 0.05). These findings reflect the multifactorial nature of UI risk, where socioeconomic factors and comorbid conditions play critical roles. Northwood et al. (17) expanded on this by identifying impaired ADL function, cognitive impairment, multiple chronic conditions, and female sex as significant UI risk factors. Odds ratios for these variables were high, ranging from 1.22 to 5.31 (p < 0.05), indicating that a combination of functional decline and chronic disease burden contributes heavily to UI risk, particularly in aging populations. Farrés-Godayol et al. (20) identified frailty, fecal incontinence, anxiety, and poor physical performance as significant predictors of UI, with prevalence ratios (PR) between 1.64 and 1.95 (p < 0.05). These findings highlight the overlap between physical and mental health conditions and their cumulative impact on UI risk. Finally, Tai et al. (19) and Suzuki et al. (18) found that immobility, constipation, cardiovascular disease, and sedative use were linked to higher UI odds, with ORs ranging from 1.97 to 11.07 (p < 0.05). Similarly, Suzuki et al. (18) identified increasing age and higher care-needs level as significant UI predictors (OR = 1.023–7.256, p < 0.05), reflecting the profound effect of both physical and cognitive decline on UI risk in elderly populations (Table 4). Overall, across the studies, female sex, impaired physical function, chronic diseases, and cognitive impairment consistently emerged as significant risk factors for UI.
Discussion
This systematic review analyzed the predictive factors for UI in the elderly, and the analysis of UI risk factors reveals a complex interplay of demographic, clinical, and functional elements. The reported overall incidence of UI varied from 14.2% to 82.9%. Key contributors include gender, with women at significantly higher risk, and physical function, where poor mobility and flexibility are linked to increased odds of UI. Comorbidities such as obesity, diabetes, and other chronic diseases amplify this risk, particularly in older adults. Additionally, muscle strength and composition play a critical role, as lower muscle mass correlates with higher UI risk. Socioeconomic factors, cognitive impairments, and conditions like frailty and anxiety further complicate the landscape of UI. Overall, these findings underscore the multifactorial nature of UI, highlighting the need for targeted interventions to improve physical health and manage chronic conditions to reduce prevalence in vulnerable populations.
Similarly, findings of a meta-analysis of 29 studies involving 518,465 individuals aged 55 to 106 years found that the global prevalence of UI among older women is 37.1% (95% CI: 29.6–45.4%). The highest prevalence was observed in older women in Asia, at 45.1% (95% CI: 36.9–53.5%). Key factors affecting the incidence of UI in older women include age (p < 0.001), obesity (p < 0.001), diabetes (p < 0.001), level of education (p < 0.001), parity (p < 0.001), hypertension (p < 0.001), smoking (p < 0.001), and urinary tract infections (p < 0.001) (22). While a systematic review from the past demonstrated the prevalence of UI among nursing home residents varied between 43% and 77%, with a median of 58%. Comparisons across studies highlighted age and sex as significant factors influencing UI prevalence. A total of 45 risk factors were identified, with individual studies showing associations between UI and factors such as sex, age, cognitive function, dementia, being bedfast, and mobility (2). Another review based on the female population demonstrated that population studies across various countries have shown that the prevalence of UI varies widely, ranging from about 5% to 70%. Most studies indicate that the prevalence falls between 25% and 45%. The rates tend to increase with age, with over 40% of women aged 70 and older affected. The prevalence is even higher among the oldest elderly and nursing home residents. Additionally, research suggests that there may be a hereditary component to UI, with family studies revealing that first-degree relatives of women with stress UI have two to three times higher prevalence rates of stress UI compared to those with continent relatives (23). Additionally, a scoping review on risk factors for UI in older men identified several significant contributors. The most prominent risk factors included increasing age, benign prostatic hyperplasia, diabetes mellitus, detrusor overactivity, and limitations in physical function or activities of daily living. Other notable factors included higher body mass index or obesity, dementia, and Parkinson's disease (24). Furthermore, a review by Kaur et al. highlighted the prevalence of UI among older adults living in the community varied from 10% to 53%, with a median of 32%. There was a correlation between UI and physical functional decline, particularly in mobility, locomotion, and interruptions in activities of daily living. While the evidence is limited, there is also an observed association between reduced cognitive function and UI (25). Another review by Aly et al. reported that in the population examined, UI had an 80% prevalence, with mixed UI being the most frequently observed type. The condition was significantly linked to several factors, including older age, functional impairments, multiparity, osteoarthritis, stroke, vaginal prolapse, and the use of laxatives (26). The results of a review by Hewiz et al. indicated that the prevalence of urinary incontinence among elderly women in Japanese and Taiwanese communities ranged from 29.8% to 31.3%. Various factors, including age, body mass index, and smoking habits, were found to impact the occurrence of UI (27).
Moreover, while comparing our findings with other studies available in the literature a Sudi Arabian cross-sectional study indicated a moderate prevalence of UI among Saudi women in Al Medina Al Munawara. Factors such as age, marital status, number of children, and certain medical conditions are linked to this issue, highlighting the necessity for comprehensive management approaches (28). While findings of a Turkish multi-centre study demonstrated that in a study of 1,176 inpatients, the prevalence of UI was found to be 29.4%, with a higher rate of 41.6% in patients aged 65 and older. Factors associated with UI included advanced age (OR, 1.966; 95% CI, 1.330–2.905), being female (OR, 2.055; 95% CI, 1.393–3.030), care dependency score (CDS) (OR, 3.236; 95% CI, 2.080–5.035), the number of coexisting health conditions (OR, 1.312; 95% CI, 1.106–1.556), end-of-life care (OR, 3.156; 95% CI, 1.412–7.052), use of sedatives (OR, 1.981; 95% CI, 1.230–3.191), and fecal incontinence (FI) (OR, 12.533; 95% CI, 4.892–32.112) for all adults. Among geriatric patients, significant associations with UI were also found for CDS (OR, 2.589; 95% CI, 1.458–4.599), end-of-life care (OR, 2.851; 95% CI, 1.095–7.424), sedative use (OR, 2.529; 95% CI, 1.406–4.548), and FI (OR, 13.138; 95% CI, 4.352–39.661) (29). Additionally, results of a community-based study from India reported the prevalence of UI among older women was identified as 63.9%. The most frequently reported type was urge incontinence, affecting 38.3% of participants, followed by mixed incontinence at 32.3%, and stress incontinence at 29.3%. Several risk factors were associated with UI, including chronic cough (OR: 1.754), chronic constipation (OR: 1.563), obesity (OR: 1.591), diabetes (OR: 1.517), and the use of medications for diabetes and hypertension (OR: 1.476). Additionally, gynecological and obstetric factors linked to UI included multiparity (OR: 1.757), home delivery (OR: 1.761), and prior pelvic surgery (OR: 1.504) (30).
The evidence from existing literature closely aligns with our findings, reinforcing the conclusions of this review regarding the prevalence of UI and its associated risk factors. In addition to the commonly recognized factors such as age, gender, and coexisting medical conditions, the literature also highlights several additional risk factors. For instance, fecal incontinence has been identified as a significant concern that can coexist with UI, complicating the clinical picture and affecting management strategies. Furthermore, the use of sedative medications has been noted as another contributing factor, potentially impacting bladder function and increasing the risk of UI. Constipation is also frequently mentioned in literature as a relevant factor, as it can exacerbate urinary symptoms due to increased abdominal pressure and bladder dysfunction. These additional risk factors underscore the complexity of UI and the importance of a comprehensive assessment and management approach that considers not only the primary urinary symptoms but also related conditions that may influence the patient’s overall health and quality of life. Addressing these factors through targeted interventions, education, and supportive care can enhance treatment outcomes and improve the well-being of those affected by UI.
Furthermore, Mainu et al. described that UI is prevalent among older adults and is often linked to various co-morbidities. Chronic illnesses like hypertension, heart failure, and arthritis can contribute to UI, and diabetes can cause it through mechanisms such as detrusor overactivity or poor glycemic control. Mental health issues like depression and anxiety are also associated with UI, often going unrecognized in older adults, which can lead to reduced life satisfaction. Geriatric syndromes, including falls, are related to urinary urgency as well. UI presents differently in various types of dementia: it tends to emerge with severe cognitive decline in Alzheimer’s patients, while in Lewy body dementia, it can appear earlier. Research shows a correlation between UI prevalence and lower mini-mental state examination scores. For patients with new-onset UI accompanied by gait disturbances and cognitive impairment, normal-pressure hydrocephalus should be considered as a possible cause. Overall, older adults with UI face a higher burden of multiple health issues compared to those without (31).
Pathophysiology
Overactive bladder is common among the elderly, characterized by symptoms like urgent urinary needs, frequent urination, and urge incontinence if involuntary loss occurs. This condition is thought to arise from involuntary contractions of the detrusor muscle, which can be confirmed through urodynamic testing. Structural changes in the bladder, such as decreased elasticity due to collagen restructuring, also contribute to this issue as the detrusor muscle ages. While, stress incontinence, on the other hand, results from a weakened sphincter mechanism at the bladder outlet, leading to involuntary urine loss during physical activities that increase abdominal pressure, like coughing or sneezing (32). In clinical practice, urge and stress incontinence often occur together, resulting in mixed incontinence. Additionally, diabetes significantly increases the risk of urinary incontinence, with nearly 25% of individuals over 75 affected in industrialized countries. The risk of severe incontinence symptoms nearly doubles in those with type 2 diabetes, especially as the duration of the disease increases. Urodynamic tests reveal abnormal findings in many elderly patients with diabetes, including reduced sensory reflexes and bladder overactivity (32).
This study provides an in-depth analysis of the risk factors related to UI among the elderly in addition to estimating its burden in terms of prevalence. This review exhibits several strengths that enhance its value in understanding UI. It synthesizes a broad range of literature, providing a comprehensive overview of UI prevalence and associated risk factors across diverse populations. The focus on specific demographic groups, particularly older adults and both genders, allows for targeted interventions that can improve clinical outcomes. The systematic search methodology and rigorous literature search further strengthen the review, ensuring a thorough and reliable analysis of available evidence.
Limitations and future research directions
The study has several limitations that should be acknowledged. One key limitation is the disparity in gender representation; while this review includes both genders, the majority of studies in the literature primarily focus on female populations. This imbalance may limit the generalizability of findings to male populations, as UI can manifest differently between genders. Additionally, the variation in study methodologies and definitions of UI across different studies could introduce inconsistencies in prevalence rates and associated risk factors. Despite these limitations, the findings remain important to publish, as they contribute valuable knowledge to the field and can inform clinical practice and future research initiatives.
Future research on UI should focus on several key directions to enhance understanding and management of the condition. Longitudinal studies are needed to track the progression of UI over time, establishing causal relationships between risk factors and onset. Additionally, targeted intervention trials should evaluate the effectiveness of exercise programs, nutritional support, and lifestyle modifications aimed at improving physical function and managing comorbidities. Investigating the unique biological and psychosocial mechanisms that contribute to higher UI prevalence in women is crucial, as is examining the interplay between mental health and UI. Further exploration of the links between sarcopenia and muscle health across demographics can inform strategies to preserve muscle function. Research should also address socioeconomic factors and their impact on access to care, alongside the potential of technology for real-time monitoring of health. Multidisciplinary approaches that integrate insights from various fields, along with culturally sensitive studies, will provide a comprehensive view of UI and inform more effective prevention and treatment strategies. Furthermore, educational interventions for both patients and healthcare providers can raise awareness and promote early intervention, ultimately improving outcomes for those affected by UI.
Conclusion
This systematic review highlights the multifactorial nature of UI, identifying critical demographic, clinical, and functional risk factors that significantly contribute to its prevalence. Key findings underscore the importance of gender differences, physical function, comorbidities, and the interplay of mental and physical health in understanding UI. Future research should focus on longitudinal studies, intervention trials, and multidisciplinary approaches to further elucidate the complex dynamics of UI and to develop effective prevention and treatment strategies.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.