Volume 4, Issue 12
December 2024
A Rare Case of Gastrointestinal Basidiobolomycosis Mimicking Appendicitis in a Young Adult
Zahrah Barnawi, Abdulrahman Alharthi, Abdulrahman Alhassani, Wied Qamrah, Arif Almasoudi, Bassam Bin Laswad, Alaa Alasiri
DOI: http://dx.doi.org/10.52533/JOHS.2024.41214
Keywords: Gastrointestinal basidiobolomycosis, Appendectomy, Fungal infection, Case report
Background: Gastrointestinal basidiobolomycosis (GIB) is a rare fungal infection caused by Basidiobolus ranarum, primarily affecting immunocompetent individuals in tropical and subtropical regions. It mimics common abdominal conditions, such as appendicitis and malignancies, leading to diagnostic challenges. Diagnosis relies on histopathology, and treatment involves a combination of surgical resection and antifungal therapy.
Case presentation: A 17-year-old male presented with right lower quadrant pain and a pelvic mass initially suspected to be an appendicular abscess. Initial diagnosis suggested a perforated appendix. After unsuccessful conservative management, open appendectomy revealed GIB on histopathology. The patient received itraconazole for 9 months, resulting in significant clinical improvement and reduction in mass size, as confirmed by follow-up imaging.
Conclusion: This case highlights the diagnostic challenges of GIB, particularly in regions where it is endemic, and the importance of considering it in the differential diagnosis of atypical abdominal presentations. Histopathology remains critical for accurate diagnosis, and a combined approach of surgical intervention and prolonged antifungal therapy proved effective, with close follow-up essential to monitor treatment response and prevent recurrence. The case underscores the need for increased awareness among clinicians to facilitate timely diagnosis and management of this rare condition.
Introduction
Gastrointestinal basidiobolomycosis (GIB) is a rare yet emerging fungal infection caused by Basidiobolus ranarum, a saprophytic fungus commonly found in soil, decaying organic matter, and the gastrointestinal tracts of amphibians, reptiles, and insectivorous bats. Traditionally associated with chronic cutaneous infections, B. ranarum has increasingly been recognized as a significant gastrointestinal pathogen affecting both children and adults (1-3). GIB poses diagnostic and therapeutic challenges due to its rarity, nonspecific clinical presentation, and geographic distribution, particularly in tropical and subtropical regions. Saudi Arabia accounts for nearly 70% of all pediatric GIB cases and ranks second in reported cases globally, indicating the localized burden of this condition in endemic areas (4, 5).
The disease predominantly affects immunocompetent individuals, though immunosuppressed patients remain at higher risk. Environmental exposure to soil, decaying vegetation, and contaminated water sources are critical risk factors for infection, as the fungus can enter the body through ingestion of contaminated food or water. However, cases in otherwise healthy individuals suggest a broader susceptibility that is not fully understood (1, 3). Once ingested, the fungus may localize to the gastrointestinal tract, causing granulomatous inflammation that mimics malignancies or other chronic inflammatory conditions, further complicating diagnosis.
Clinical presentation is highly variable, with common symptoms including abdominal pain, fever, diarrhea, weight loss, and palpable abdominal masses. In advanced cases, patients may develop complications such as bowel obstruction, perforation, or fistula formation. The nonspecific nature of these symptoms often leads to misdiagnoses, with GIB frequently mistaken for inflammatory bowel disease, tuberculosis, or neoplasms (6).
Histopathological examination is the gold standard for diagnosis, typically revealing characteristic fungal hyphae surrounded by eosinophilic material, known as the Splendore-Hoeppli phenomenon. Imaging studies such as CT and MRI are often used but are nonspecific and primarily aid in identifying complications or guiding biopsies. Culture of B. ranarum from tissue samples may confirm the diagnosis but is technically challenging and time-consuming, often leading to delays. Management involves a combination of surgical intervention to resect infected tissue and antifungal therapy. Itraconazole is the most commonly used antifungal agent, given its efficacy and safety profile. Amphotericin B may be used in severe or refractory cases (7). Despite these therapeutic options, treatment can be protracted, lasting several months to ensure eradication of the infection. Delay in diagnosis and treatment can significantly increase morbidity and mortality, with a reported case-fatality rate of 18.6% in 2019 (8).
The case presented in this report highlights a unique instance of GIB that clinically mimicked appendicitis in a young patient. It highlights the importance of considering this rare infection in the differential diagnosis of atypical gastrointestinal presentations, particularly in endemic regions, to avoid delays in diagnosis and improve patient outcomes.
Case presentation
On 21 November 2023, a 17-year-old male patient with a history of asthma presented to the emergency department complaining of right lower quadrant pain for one month. The pain started gradually in the umbilical area before shifting to the right lower quadrant and flank. It was colicky in nature, intermittent, and relieved by analgesia. The associated symptoms included undocumented fever and polyuria. There were no changes in bowel habits, other urinary symptoms, or recent upper respiratory tract infections. The patient is currently using Salbutamol on an as-needed basis to manage his asthma symptoms. The patient was surgically free, denied smoking and had neither recent contact with sick persons nor previous similar complaints.
On examination, the patient was fully conscious, oriented and alert. His vital signs were as follows:
Temperature: 36.8°C (Reference range: 36.5-37.5°C)
Blood pressure: 103/71 mmHg (Reference range: 90-120/60-80 mmHg)
Pulse: 61 bpm (Reference range: 60-100 bpm)
Respiratory rate: 17 breaths/min (Reference range: 12-20 breaths/min)
Oxygen saturation: 97% (Reference range: 95-100%)
Abdominal examination revealed tenderness in the right lower quadrant with positive rebound tenderness. Below is Table 1 showing the patient’s initial laboratory results.
|
Table 1: Initial Laboratory Results |
||||
|
Procedures |
Normality |
Results |
Unit |
Reference Range |
|
CBC Differential |
||||
|
WBC |
Normal |
9.56 |
X10^3/uL |
(4 - 11) |
|
RBC |
Normal |
4.92 |
X10^12/L |
(4.5 - 5.5) |
|
HGB |
Low |
10.8 |
g/dL |
(13 - 17) |
|
HCT |
Low |
34.5 |
% |
(40 - 50) |
|
MCV |
Low |
70.1 |
fL |
(83 - 101) |
|
MCH |
Low |
22 |
Pg |
(27 - 32) |
|
MCHC |
Low |
31.3 |
G/DL |
(31.5 - 34.5) |
|
Platelet count |
Normal |
396 |
X10^9/L |
(150 - 400) |
|
MPV |
Normal |
9.3 |
fL |
(7.4 - 10.9) |
|
Automated Differential |
||||
|
Neutrophil % |
Low |
32.4 |
% |
(40 - 80) |
|
Lymphocyte % |
Normal |
35 |
% |
(20 - 40) |
|
Monocyte % |
High |
10.1 |
% |
(2 - 10) |
|
Eosinophils % |
High |
21.9 |
% |
(1 - 6) |
|
Basophils % |
Normal |
0.6 |
% |
(0 - 1) |
|
Neutrophil Count |
Normal |
3.09 |
10^3/UL |
(2 - 7.5) |
|
Lymphocyte Count |
Normal |
3.35 |
10^3/UL |
(1.5 - 3.5) |
|
Monocyte Count |
High |
0.97 |
10^3/UL |
(0.2 - 0.9) |
|
Eosinophils Count |
Hight |
2.09 |
10^3/UL |
(0.02 - 0.5) |
|
Basophils Count |
Normal |
0.06 |
10^3/UL |
(0.02 - 0.1) |
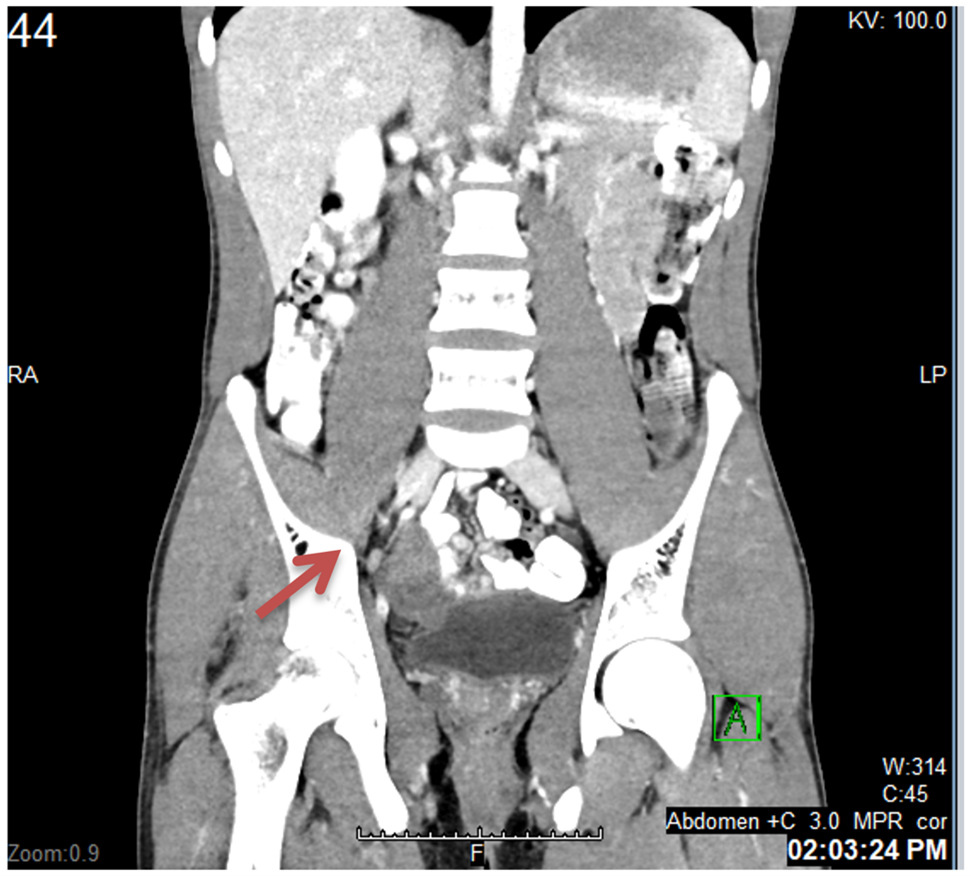
Despite an Alvarado score of 4 out of 10, which suggests a low likelihood of acute appendicitis, the patient's symptoms noticeably pointed towards the condition. Chest and abdominal X-rays were unremarkable. On November 22, 2023, the patient was admitted for a CT scan of the abdomen and pelvis with intravenous and oral contrast. The scan revealed a heterogeneous, slightly hypodense pelvic mass measuring approximately 4.9 x 4.0 cm with peripheral enhancement, suggestive of an abscess secondary to a perforated appendix (Figures 1, 2).
Figure 1: Coronal CT image from the abdomen and pelvis.
Figure 1 - Coronal CT image from the abdomen and pelvis: shows a heterogeneous, slightly hypodense pelvic mass (arrow) measuring approximately 4.9 x 4.0 cm with peripheral enhancement, suggestive of an abscess secondary to a perforated appendix.
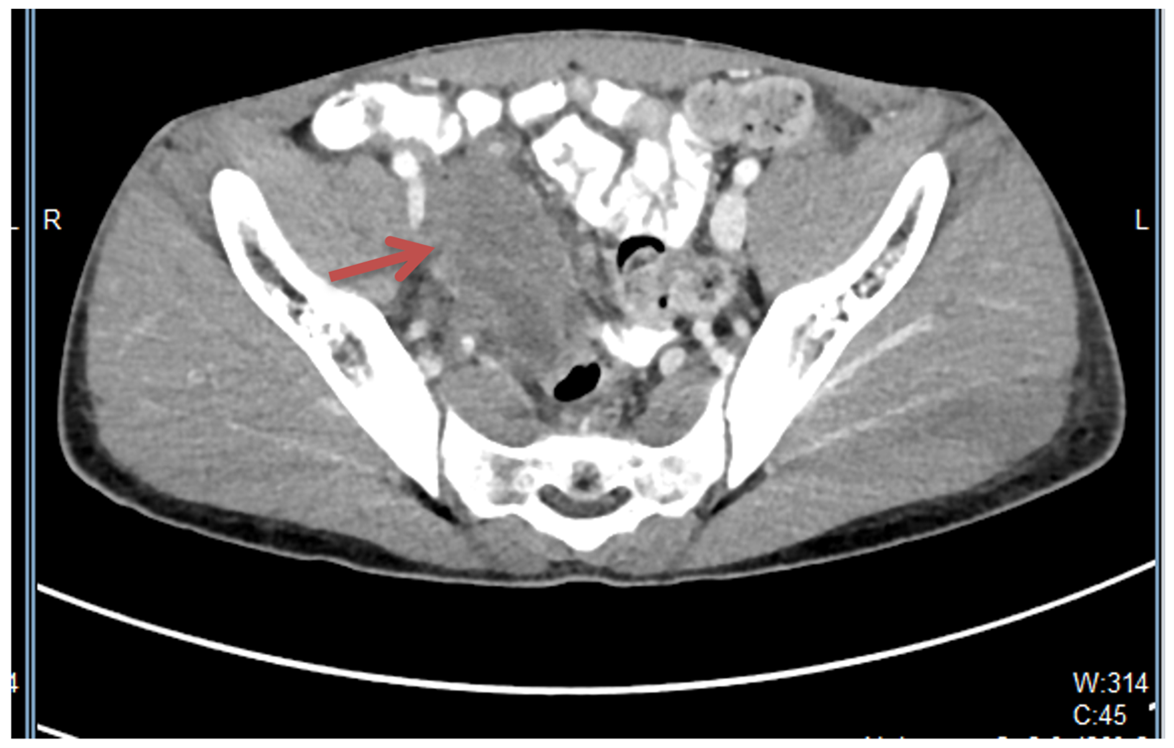
Figure 2: Axial CT image from the right iliac fossa and pelvis.
Figure 2 - Axial CT image from the right iliac fossa and pelvis: shows the suggested appendicular abscess (arrow) obscuring the view of right ureter.
The patient was admitted and conservative therapy was initiated from 22 - 27 November 2023, where the patient was on IV (intravenous) fluids only for the first day admission and tolerated regular diet from the second day. He was started on Cefuroxime 750 mg IV and Metronidazole 500 mg IV; both were given 3 times a day for 7 days. After 5 days of conservative therapy, an abdominal ultrasound was done and showed a right pelvic hypoechoic lesion measuring about 53 x 40 mm, with no detectable vascularity.
Due to inadequate clinical improvement and unchanged mass size, the patient underwent open appendectomy on 28 November 2024. Intraoperative findings revealed an appendicular mass at the tip of the appendix, adherent to the terminal ileum and posterior abdominal wall, with a normal proximal appendix and serous free fluid in the right iliac fossa.
An appendicular specimen was taken for histopathological examination. The report identified fibrous tissue with extensive inflammation and numerous invasive fungal organisms surrounded by dense eosinophilic material “Splendore-Hoeppli phenomenon” morphologically consistent with basidiobolomycosis (Figures 3, 4).
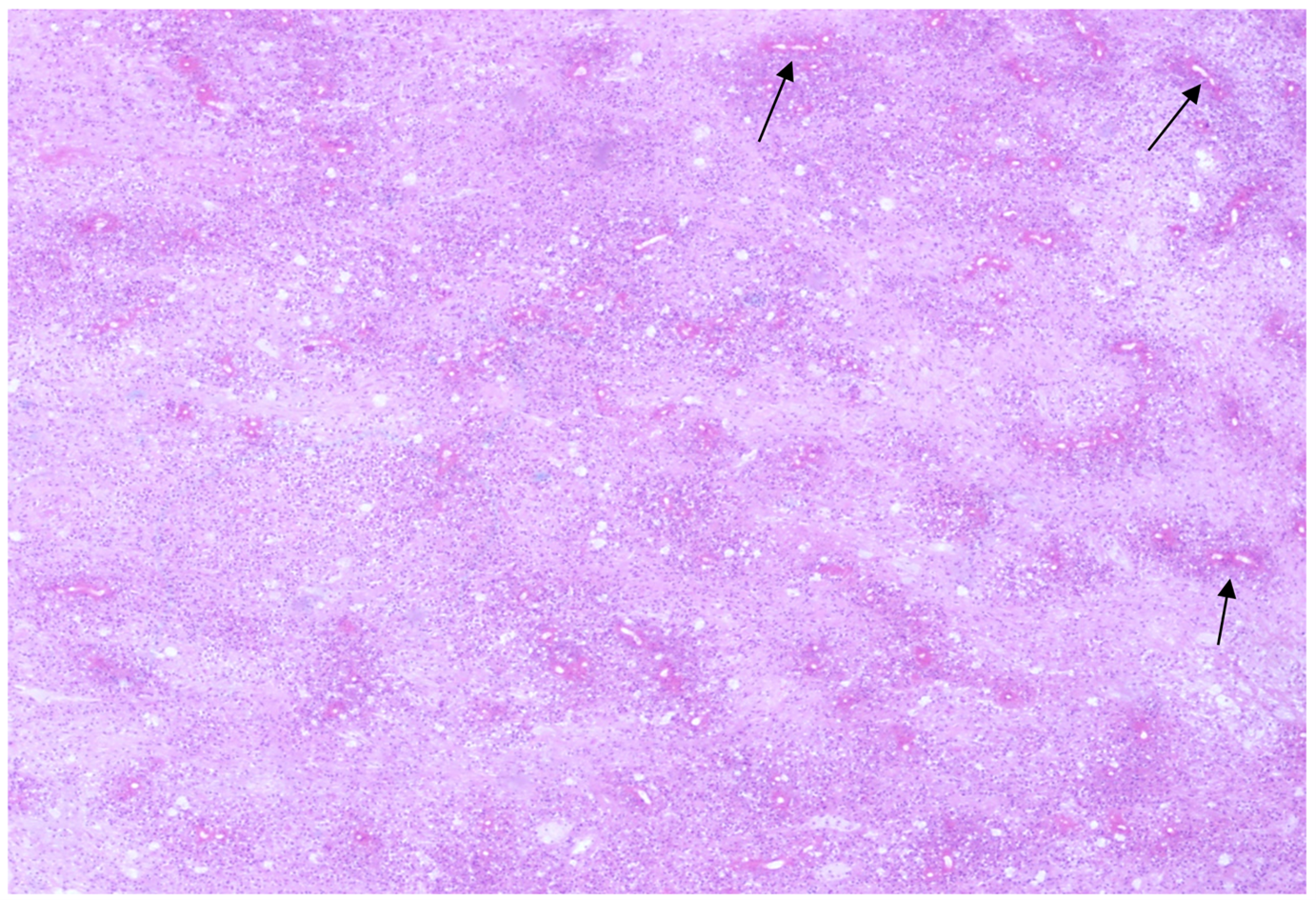
Figure 3: Hematoxylin and eosin (H&E) stain (x40).
Figure 3 - Hematoxylin and eosin (H&E) stain (x40): shows numerous basidiobolomycosis fungal organisms (arrows) surrounded by dense eosinophilic material and embedded in a dense eosinophil-rich mixed inflammatory cell infiltrate.
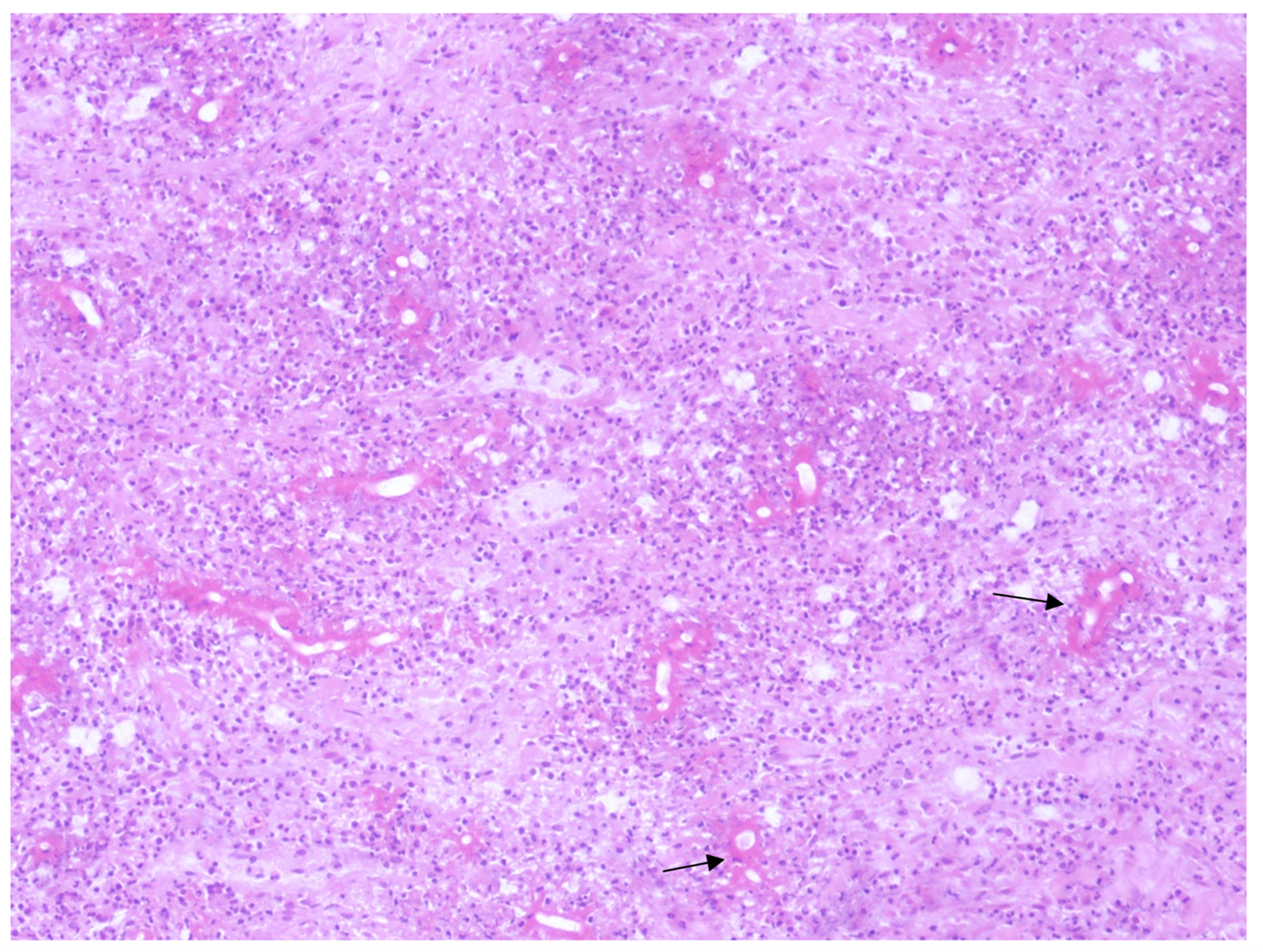
Figure 4: H&E stain (x100).
Figure 4 - H&E stain (x100): basidiobolomycosis fungal organisms comprised of fragmented hyphae with infrequent septations, surrounded by dense eosinophilic material known as Splendore-Hoeppli phenomenon (arrows).
The patient was discharged on 30 November 2023, and on 6 December 2023 he followed up in the outpatient clinic and started on itraconazole for 6 months. A few months later, on 25 February 2024, follow-up in the outpatient clinic showed improvement in urinary symptoms and pain. An abdominal and pelvic ultrasound was unremarkable.
A follow-up CT on May 1, 2024, demonstrated a decrease in the size of the right para-midline pelvic mass to 3.1 x 2.1 x 3 cm, compared to the previous 4.4 x 6 x 8 cm. Mild mass effect on the right lateral aspect of the urinary bladder and interval improvement of right-side hydroureteronephrosis were noted (Figure 5). The patient responded well to treatment and was discharged for another three months of itraconazole therapy.
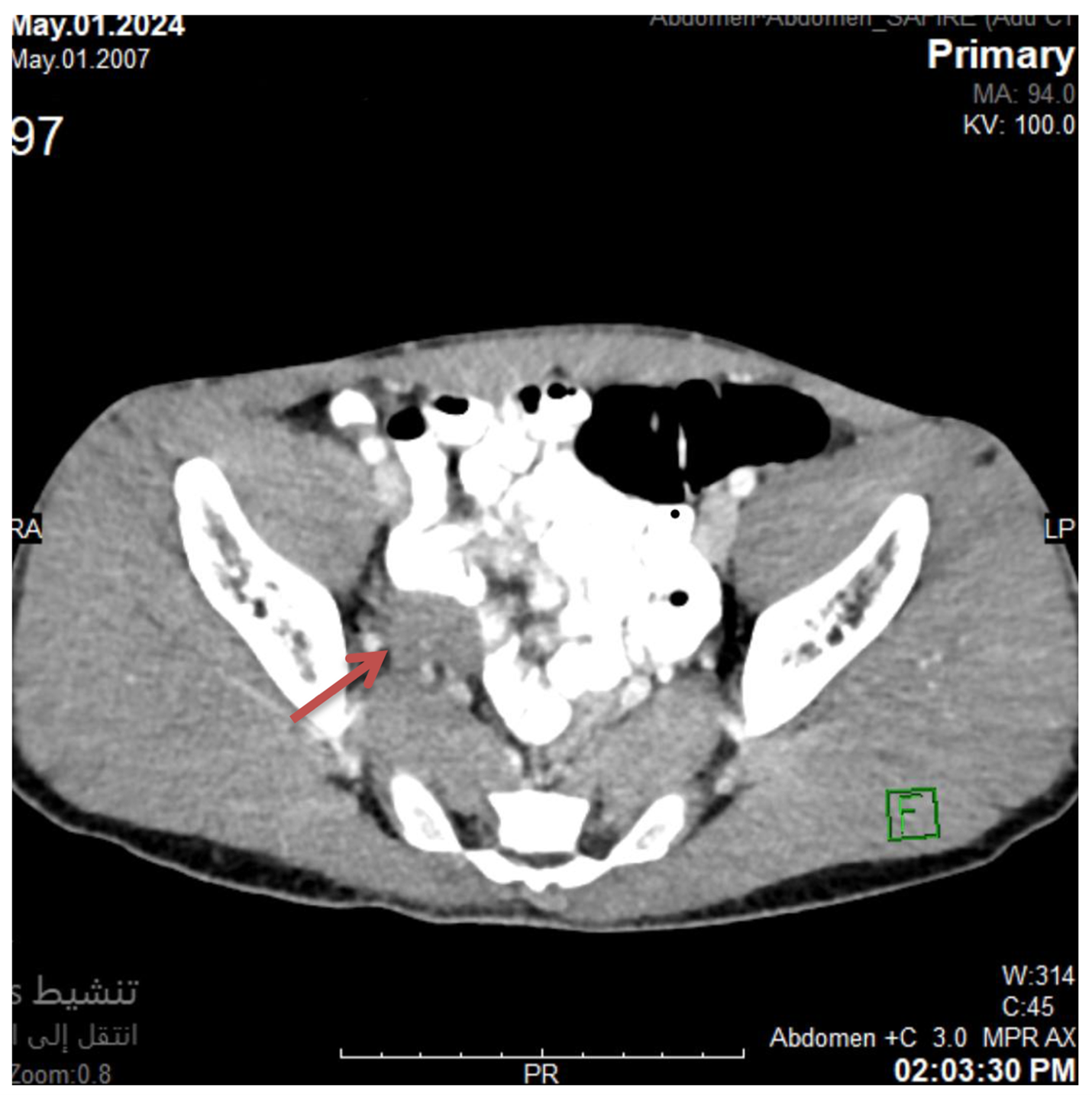
Figure 5: Axial CT image from the right iliac fossa and pelvis.
Figure 5 - Axial CT image from the right iliac fossa and pelvis: shows that the right pelvic mass decreased in size (3.1 x 2.1 x 3 cm) compared to the previous measurements (4.4 x 6 x 8 cm).
Discussion
GIB is an emerging fungal infection that presents significant diagnostic and therapeutic challenges, particularly in endemic regions. This case report of a 17-year-old male with GIB mimicking appendicitis contributes to the growing body of literature on this rare condition and highlights several important clinical considerations.
While GIB has a worldwide distribution, it is predominantly reported in tropical and subtropical regions. Our case aligns with the geographical prevalence noted in the literature, with Saudi Arabia being a hotspot for GIB cases (9-11). While previous cases have often involved adults, such as Ejtehadi et al. (2014) (12) who reported on a 41-year-old woman, and Alsaeed et al. (2023) (13) described a case involving a 69-year-old male, the occurrence of GIB in this younger patient highlights the necessity of considering this diagnosis across a broader age spectrum, not just in older individuals.
The present case shares several similarities with previously reported cases of GIB, particularly in terms of initial presentation. Our patient's symptoms of abdominal pain, fever, and a palpable mass align with the clinical picture described by Meeralam et al. (2024) (14), Mirmoosavi et al. (2023) (10) and Alabdan et al. (2020) (11). The initial misdiagnosis as appendicitis is not uncommon in GIB cases. Alsaeed et al. (2023) (14) and Mirmoosavi et al. (2023) (10) reported similar instances where GIB mimicked diverticulitis and Crohn’s disease, respectively leading to delayed diagnosis. Additionally, in the case series reported by Meeralam et al. (2024) (12), many patients were initially misdiagnosed as malignancies or inflammatory bowel disease. This pattern of misdiagnosis highlights the nonspecific nature of GIB symptoms and the importance of maintaining a high index of suspicion, especially in endemic areas.
Diagnosing GIB preoperatively remains a challenge due to its nonspecific symptoms and limitations in diagnostic tools. Elevated eosinophil counts, as observed in this case, are a characteristic feature of GIB and align with findings from prior studies (9, 11-14). Eosinophilia may indicate an immune response attributed to the host's attempt to combat the fungal organism, as eosinophils play a crucial role in the defense against certain fungal pathogens (15). This eosinophilia, coupled with the presence of an abdominal mass on radiological imaging, should raise suspicion for GIB in endemic regions.
The CT findings in our case, showing a heterogeneous, slightly hypodense pelvic mass, align with the imaging characteristics described in a previous report where abdominal CT revealed a right mesenteric mass (11). Nevertheless, the initial interpretation as an abscess secondary to a perforated appendix highlights the nonspecific nature of these radiological findings and the potential for misdiagnosis. Diagnosis of GIB is challenging to establish preoperatively. Although several case reports have utilized preoperative diagnostic methods such as endoscopy and biopsy, these approaches have largely been unsuccessful in confirming the diagnosis (16). Similar to prior cases, fungal culture was not performed as it was not considered prior to surgery. It has been reported that a positive culture for B. ranarum is obtained in only 50% to 65% of cases; therefore, a negative culture does not definitively exclude the diagnosis (8, 16).
The definitive diagnosis of GIB in our case was made through histopathological examination of surgical specimens, revealing fibrous tissue with extensive inflammation and numerous invasive fungal organisms. This aligns with the consensus in the literature that histopathology remains the gold standard for diagnosis (9-14). The characteristic Splendore-Hoeppli phenomenon, mentioned in our histopathology report, was also found in the GIB case studied by Alabdan et al. (11).
The management of GIB in this case involved a combination of surgical resection and antifungal therapy and offers several advantages. Surgical intervention allows for debulking of the fungal mass and obtaining tissue for definitive diagnosis, while antifungal therapy targets residual infection and prevents recurrence. This approach is consistent with the current standard of care for GIB (5, 11, 14). The positive response to this treatment regimen, evidenced by symptomatic improvement and reduction in mass size on follow-up imaging, supports the efficacy of this approach.
The treatment duration, initially set at six months and extended by three months, was guided by the patient’s clinical response and imaging findings, aligning with reported durations of 4–18 months (10-12, 14). The decision to extend treatment was based on the patient's clinical response and imaging findings, emphasizing the need for individualized treatment plans and close follow-up in GIB cases. However, this approach has potential drawbacks to consider. Surgical intervention carries inherent risks, including the possibility of spreading the infection or causing complications. Moreover, the optimal duration of antifungal therapy remains unclear, with the potential for side effects increasing with prolonged treatment.
Alternative approaches, such as antifungal therapy alone, have shown success in some cases (10, 12). This approach may be preferable in patients who are poor surgical candidates or when the infection is diagnosed early. However, it may be less effective in cases with extensive tissue invasion or when rapid symptom relief is necessary as reported by Alsaeed et al. (2023) who found that medical treatment alone was unsuccessful, ultimately resulting in a fatal outcome (13). The choice of antifungal agent is another important consideration. While itraconazole is commonly used and was effective in our case, some studies have reported success with other agents such as voriconazole (9). Thus, the selection of antifungal therapy should be guided by susceptibility testing, when possible, as demonstrated by Khan et al. (2001) (6), who found varying susceptibility patterns among different antifungal agents.
This case contributes important insights into the diagnosis and management of GIB. It expands the known demographic range by demonstrating GIB's occurrence in a younger patient, emphasizing the need for clinicians to consider this diagnosis across all age groups. It also illustrates GIB's ability to mimic common conditions like appendicitis, highlighting the importance of increased awareness among healthcare providers, especially in endemic regions. The successful outcome using a combined surgical and antifungal approach provides insights into effective GIB management strategies, while underscoring the value of personalized treatment duration based on individual clinical and radiological responses. Additionally, the improvement of atypical symptoms like polyuria post-treatment suggests potential systemic effects of GIB, opening new avenues for investigating this fungal infection's broader impact on various body systems.
Although this case report adds valuable insights to the existing literature on GIB, it has some limitations. As a single case study, it cannot provide general conclusions about the optimal management of GIB. Furthermore, the lack of long-term follow-up data limits our understanding of potential recurrence rates or long-term complications. Also, this condition is rare, and existing studies are mostly case reports or small case series, limiting the generalizability of findings.
Future research should focus on developing more specific diagnostic tools for GIB, potentially including serological tests or molecular techniques. In addition, prospective studies comparing different antifungal regimens and treatment durations could help establish more standardized treatment protocols for this rare but potentially severe fungal infection. The role of newer antifungal agents and combination therapies in managing GIB also warrants further investigation.
Conclusion
This case underscores the importance of maintaining a high index of suspicion for GIB in patients presenting with atypical abdominal masses, even in younger age groups. It highlights the critical role of histopathological examination in diagnosis and the efficacy of combined surgical and antifungal therapy in managing this challenging condition. As our understanding of GIB continues to evolve, cases like this contribute to the growing knowledge base and help refine diagnostic and treatment strategies for this emerging fungal infection.
Disclosures
Author Contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
An informed consent was provided by the patient to include the data anonymously. Furthermore, the institute where the case was reported from approved the publication of the case.
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not Applicable