Volume 4, Issue 12
December 2024
Diagnostic and Prognostic Significance of Blueberry Muffin Rash in Neonates
Salah Mohammed Alzanbagi, Mohammed Babonji, Abdulaziz Alradha, Alaa Abdallah Mohamedsalih, Mohammed Yousef Al Saleem, Mohammed Jamal Junainah, Nawaf Ali Mansour, Abdulrahman Obaid Alanazi, Hassan Meshal Almalki
DOI: http://dx.doi.org/10.52533/JOHS.2024.41203
Keywords: blueberry muffin rash, neonates, congenital infections, hematologic disorders, diagnosis, management
This review examines the diagnostic and prognostic significance of blueberry muffin rash in neonates, a distinctive dermatological presentation that often indicates serious underlying systemic conditions. The rash, characterized by purplish-blue macules or papules resembling small bruises, is associated with extramedullary hematopoiesis (EMH), a process where blood cell production occurs outside the bone marrow due to specific pathologic conditions. Common etiologies include congenital infections, particularly those in the TORCH complex—Toxoplasmosis, Other (such as syphilis), Rubella, Cytomegalovirus (CMV), and Herpes simplex virus—hematologic disorders like hemolytic disease of the newborn (HDN), and metabolic diseases, including lysosomal storage disorders. Each of these underlying conditions presents unique challenges and implications for the neonate's health. Early recognition of blueberry muffin rash, as it can prompt immediate and thorough evaluation to identify the underlying cause, which is crucial for guiding appropriate diagnostic testing and timely intervention. The prognostic implications vary significantly depending on the etiology; for example, congenital infections may lead to long-term complications such as sensorineural hearing loss or developmental delays, while hematologic disorders may require urgent interventions like blood transfusions. A comprehensive diagnostic approach, including maternal history assessment, laboratory investigations, and imaging studies, is essential for narrowing down potential causes. Management of blueberry muffin rash requires a multidisciplinary approach, involving pediatricians, neonatologists, dermatologists, and infectious disease specialists to ensure holistic care for affected infants. Immediate interventions depend on the specific diagnosis, while long-term follow-up is vital for monitoring developmental progress and addressing potential complications. Additionally, the review highlights the importance of providing family education and psychosocial support to help parents navigate the complexities of care associated with their child's condition. Finally, preventive measures, including vaccination and public health education, are crucial for reducing the incidence of congenital infections that can lead to blueberry muffin rash.
Introduction
The blueberry muffin rash in neonates, though relatively rare, is a striking dermatological finding that often signals an underlying systemic condition. Named for its resemblance to a blueberry muffin, with characteristic purplish-blue macules or papules distributed across the skin, this rash represents a distinct manifestation of extramedullary hematopoiesis (EMH) (1). While blood cell production typically takes place within the bone marrow, certain pathological conditions occurring during fetal development can trigger hematopoietic activity in other tissues, including the skin, leading to the characteristic appearance of the rash post-birth. This EMH is usually indicative of intrauterine stress, infection, or hematologic and metabolic abnormalities, making the blueberry muffin rash an important clinical sign that warrants immediate and thorough evaluation (2).
The diagnostic and prognostic significance of the blueberry muffin rash has been widely documented across multiple domains of pediatric medicine. Research has consistently linked this rash to several key etiologies, including congenital infections, hematologic conditions, and metabolic storage diseases. Notably, congenital infections associated with the TORCH complex—Toxoplasmosis, Other agents (such as syphilis), Rubella, Cytomegalovirus (CMV), and Herpes simplex virus—are among the most common causes (3). These infections, when contracted during pregnancy, can cross the placenta and infect the fetus, causing immune responses that manifest as EMH. Additionally, hematologic disorders like hemolytic diseases, such as Rh disease, and certain cases of neonatal leukemia have been identified as underlying causes, as the body attempts to produce blood cells outside the marrow to compensate for an increased demand (4). Metabolic disorders, though less common, are also associated with blueberry muffin rash, as abnormal lipid or cellular accumulation can lead to skin infiltration and discoloration.
Understanding the significance of this dermatologic presentation in neonates is crucial for pediatricians and neonatologists. Since the rash can signal potentially serious conditions, early recognition is essential to prompt appropriate diagnostic testing. Identifying the underlying etiology is not only diagnostically important but can also provide valuable prognostic insights, as outcomes vary significantly depending on the underlying cause. For instance, neonates with TORCH infections often face risks of developmental delays and sensorineural impairments, while cases related to hematologic conditions like neonatal leukemia may require urgent intervention with chemotherapy or supportive therapies (5).
This literature review aims to provide an in-depth examination of the diagnostic and prognostic implications of blueberry muffin rash in neonates, focusing on the various underlying etiologies, available diagnostic approaches, and their associated outcomes.
Methodology
This study employs a comprehensive literature search conducted on October 31, 2024, utilizing the Medline and Cochrane databases. We applied medical subject headings (MeSH) along with a combination of relevant terms to ensure a thorough exploration of the topic. To capture all pertinent research, we also conducted a manual search via Google Scholar, referencing the citations from identified studies as a foundation for our inquiry. Our focus was on identifying valuable insights related to the diagnostic and prognostic significance of blueberry muffin rash in neonates. No restrictions were placed on the date of publication, language, participant age, or type of study, allowing for a broad spectrum of relevant literature to be included in our review.
Discussion
Etiology and Pathogenesis of Blueberry Muffin Rash
The blueberry muffin rash in neonates serves as a visible manifestation of EMH (2). Under normal circumstances, blood cell production in the fetus begins in the liver and spleen and gradually shifts to the bone marrow during the later stages of development. By the time of birth, hematopoiesis outside the bone marrow is typically minimal or absent. However, when certain pathologic conditions arise in utero, they can stimulate blood cell production in non-marrow sites, including the dermis. This results in the appearance of deep blue or purplish macules or papules across the skin, resembling small bruises or "blueberries." Understanding the etiology and pathogenesis of blueberry muffin rash requires examining the conditions that stimulate this unusual hematopoietic activity, specifically congenital infections, hematologic disorders, and metabolic diseases.
Congenital infections are among the most common causes of blueberry muffin rash in neonates, often associated with the TORCH infections. When transmitted from mother to fetus during pregnancy, these infections can lead to significant fetal immune responses and systemic complications. Rubella, one of the classical causes of blueberry muffin rash, is particularly dangerous if contracted during the first trimester, as the virus can cross the placenta and infect the fetus, impairing liver and bone marrow hematopoiesis and forcing blood cell production to occur in the skin. Neonates with rubella-induced blueberry muffin rash often face long-term complications such as sensorineural deafness, cardiac defects, and developmental delays, underscoring the importance of early identification and vaccination for prevention (6). CMV is another leading cause of blueberry muffin rash, with infected fetuses developing EMH due to CMV-induced inflammation, increasing the risk of other serious outcomes like microcephaly, hepatosplenomegaly, and cerebral calcifications (7). Identification of blueberry muffin rash in a neonate with suspected CMV often prompts further testing for neurodevelopmental sequelae. Toxoplasmosis and syphilis are also associated with EMH and the characteristic rash (8). In toxoplasmosis, the rash is often accompanied by chorioretinitis and intracranial calcifications, while in congenital syphilis, it may co-occur with copper-colored rashes or bullae.

Figure 1: Neonate with a Blueberry Muffin Appearance Associated with Congenital Cytomegalovirus Infection. Classically described “blueberry muffin” appearance of a neonate with congenital CMV consisting of a diffuse petechial or purpuric rash and jaundice (conjugated) (9).
Certain hematologic conditions can also cause blueberry muffin rash in neonates. These conditions typically involve either abnormal blood cell production or destruction, necessitating compensatory EMH to meet blood cell needs. Hemolytic disease of the newborn (HDN), arising from Rh or ABO incompatibility, is a primary hematologic cause (10). In HDN, maternal antibodies cross the placenta and destroy fetal red blood cells, leading to anemia and stimulating EMH in non-marrow tissues, including the skin. The presence of blueberry muffin rash in neonates with HDN suggests significant in utero hemolysis and anemia, often requiring urgent intervention, such as phototherapy or exchange transfusions. Rarely, neonatal leukemia can present with blueberry muffin rash. Leukemic blast cells infiltrate the skin, causing bluish lesions, indicating an advanced stage of disease that typically requires aggressive chemotherapy. Differentiating leukemic infiltration from other causes of blueberry muffin rash is critical, as management and prognosis differ significantly (11).
Metabolic storage diseases, though less frequently associated with blueberry muffin rash, are an important group of conditions that can cause similar skin manifestations. These disorders generally involve the abnormal accumulation of cellular or biochemical substances in organs, including the skin, which may mimic the appearance of EMH. Niemann-Pick disease, a lysosomal storage disorder characterized by sphingomyelin accumulation, can cause bluish or purplish skin lesions that resemble blueberry muffin rash (12). Affected neonates often present with hepatosplenomegaly and neurological impairment and typically have a poor prognosis without treatment. Gaucher disease, another lysosomal storage disorder involving glucocerebroside accumulation, can cause hepatosplenomegaly and similar skin findings (13). However, the lesions in Gaucher disease are not due to EMH, and diagnosis generally requires genetic testing and enzyme assays.
In rare cases, a blueberry muffin rash may be idiopathic or arise from non-specific inflammatory responses. Benign vascular conditions, such as congenital hemangiomas, can sometimes mimic blueberry muffin rash, though they are usually distinguishable through imaging or biopsy (14). Idiopathic cases of blueberry muffin rash, where no cause is identified, are generally self-limiting and may resolve without significant intervention, although monitoring is advised to rule out delayed onset of underlying conditions.
Prognostic Implications of Blueberry Muffin Rash in Neonates
The blueberry muffin rash in neonates carries a range of prognostic implications, varying widely based on the underlying cause. Although the rash itself poses no direct harm, it serves as a visible indicator of potentially serious systemic conditions. The prognosis largely depends on whether the cause is a congenital infection, a hematologic disorder, or a metabolic disease. Congenital infections, particularly those in the TORCH complex, can significantly impact an infant's long-term health. For instance, neonates with rubella face a risk of sensorineural hearing loss, heart defects, and developmental delays, especially if infected early in pregnancy (15). Similarly, congenital CMV infection often leads to neurodevelopmental impairments, with up to 50% of symptomatic infants developing sensorineural hearing loss and other complications (16). Early antiviral treatment can reduce some of these risks, but many affected neonates may still experience lasting disabilities.
In cases of hematologic conditions, such as HDN, the blueberry muffin rash indicates severe anemia caused by maternal antibodies attacking fetal red blood cells (17). The prognosis in HDN is generally favorable with timely interventions like blood transfusions, although neonates may require neurodevelopmental monitoring if bilirubin levels reach neurotoxic levels. On the other hand, neonatal leukemia, a rare cause of blueberry muffin rash, has a poorer prognosis due to the aggressive nature of the disease and the challenges of chemotherapy in young infants. However, some types, such as those associated with transient abnormal myelopoiesis in Down syndrome, may have a more favorable outlook. Metabolic and genetic disorders also present complex prognostic challenges. Lysosomal storage diseases like Niemann-Pick and Gaucher disease can result in significant morbidity and mortality, with progressive neurological decline and limited life expectancy in severe cases. For example, Niemann-Pick disease can lead to neurodegeneration and respiratory issues, while severe forms of Gaucher disease can impair growth and cognitive development (18, 19). Although enzyme replacement therapy exists for Gaucher disease, it is less effective in severe neurological forms, limiting the potential for full recovery.
In rarer cases, the rash may be idiopathic or associated with benign vascular conditions like congenital hemangiomas, which typically have an excellent prognosis. These conditions often resolve on their own or respond well to minimal treatment, leaving the infant with no lasting effects. Idiopathic cases of EMH, where no clear cause is identified, usually follow a benign course, with the rash disappearing within weeks or months without intervention.
Clinical Implications and Management
The clinical implications and management of blueberry muffin rash in neonates are multifaceted, primarily due to the wide range of underlying conditions that can manifest with this skin finding. The presence of blueberry muffin rash serves as an important diagnostic clue, alerting clinicians to potential systemic issues that may require immediate intervention (20). This rash is considered a cutaneous sign rather than an isolated dermatologic condition, thus demanding a multidisciplinary approach to diagnosis and management. Thorough evaluation, including a detailed maternal history, laboratory investigations, and imaging studies, is essential for determining the underlying cause and guiding appropriate management strategies.
Upon presentation of blueberry muffin rash, a comprehensive diagnostic approach is necessary to narrow down the underlying etiology. The differential diagnosis primarily includes congenital infections, hematologic disorders, and metabolic storage diseases. Clinicians often start with a maternal history review to identify any risk factors, such as exposure to infectious agents during pregnancy, maternal serologies, and any history of hematologic conditions. Laboratory tests like complete blood count (CBC), liver function tests, and blood cultures provide important baseline information on the neonate’s overall health (3). Additionally, specific infectious disease panels—especially for TORCH infections—are routinely conducted. Advanced imaging, such as ultrasound or MRI of the liver and spleen, can help detect hepatosplenomegaly, which is commonly associated with infections and storage diseases (21). Where leukemia is suspected, a skin biopsy and bone marrow aspiration may be warranted, as these can reveal blast cells or other malignant features. Genetic testing may be indicated if a metabolic or lysosomal storage disorder like Niemann-Pick or Gaucher disease is suspected. Ultimately, differentiating between these potential causes is crucial, as it influences prognosis and guides treatment plans.
Management of blueberry muffin rash depends on the underlying diagnosis, with a priority placed on addressing any life-threatening conditions. For neonates diagnosed with severe infection, early intervention with antiviral or antibiotic therapy is crucial. For instance, congenital CMV infection is often managed with antiviral agents like ganciclovir, which, if started early, can help reduce the risk of neurodevelopmental complications (23). In cases of severe anemia associated with conditions such as HDN, supportive measures like phototherapy and blood transfusions may be needed to manage hemolysis and reduce bilirubin levels (24). Phototherapy is particularly important as it helps prevent bilirubin from reaching neurotoxic levels that could cause kernicterus. Exchange transfusions may be necessary for severe cases where anemia is profound, and there is a high risk of neurologic damage.
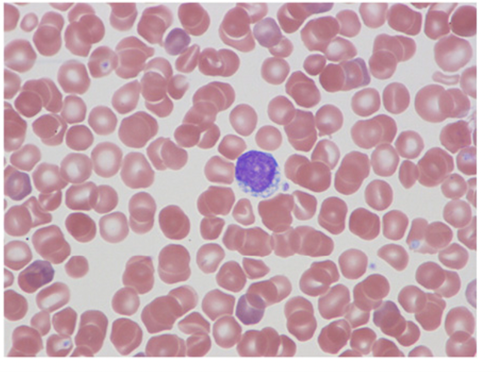
Figure 2: Cytoplasmic vacuoles within the lymphocytes on the peripheral smear (22).
For neonates diagnosed with conditions like congenital infections, metabolic disorders, or hematologic conditions, long-term monitoring and follow-up are essential components of care. Infants with congenital rubella or CMV infection, as mentioned earlier, are at significant risk of developing sensorineural hearing loss, vision impairment, and neurodevelopmental delays. Regular auditory and ophthalmologic assessments are recommended to detect and manage any progressive sensory deficits (25). Additionally, neurodevelopmental evaluations should be conducted to monitor potential cognitive or motor delays, which are common in congenital infections and some metabolic diseases. For conditions like Niemann-Pick or Gaucher disease, genetic counseling and regular follow-ups are needed to assess for disease progression, as these disorders can involve multiple organs, including the central nervous system (26, 27). In cases of neonatal leukemia, close hematologic monitoring is required to manage the effects of chemotherapy and monitor for remission. Although rare, leukemic relapse can occur, necessitating ongoing follow-up to detect any recurrence.
Blueberry muffin rash cases often require a multidisciplinary approach involving pediatricians, neonatologists, dermatologists, infectious disease specialists, and, when necessary, genetic counselors and hematologists. Collaborative care is essential, as these cases often involve multiple organ systems and require coordinated intervention across specialties (28). For example, infectious disease specialists play a key role in the diagnosis and management of TORCH infections, advising on appropriate antiviral or antibiotic therapies. Genetic counseling is also critical when metabolic disorders are involved, as parents may need support in understanding the implications of their child’s diagnosis and potential genetic risks for future pregnancies. Neonatologists and pediatricians oversee general supportive care and follow-up, monitoring for developmental progress and addressing any emerging complications.
In addition to clinical care, providing psychosocial support and education for the family is an important component of management. Parents of neonates with blueberry muffin rash may experience significant anxiety, given the potential for serious underlying conditions. Clear communication regarding the diagnostic process, expected outcomes, and potential complications is essential for supporting families and managing expectations. Educational materials can be provided to help parents understand their child’s condition and the importance of follow-up care. For families dealing with chronic or progressive conditions, such as storage diseases or congenital infections with long-term impacts, connecting them with resources like support groups and counseling can be beneficial. Psychosocial support services are particularly valuable in cases where there are likely long-term developmental or health challenges, as families may need ongoing assistance in navigating the complexities of care.
Preventive measures, especially for infections like rubella and CMV, are an important consideration in reducing the incidence of blueberry muffin rash and its associated complications (7). Vaccination programs, particularly rubella immunization, play a critical role in preventing congenital rubella syndrome. Prenatal screenings and health education for pregnant women about avoiding specific infectious risks can also reduce the incidence of TORCH infections. Public health initiatives that promote awareness of prenatal care, vaccination, and screening can help minimize the risk of congenital infections that lead to blueberry muffin rash.
Conclusion
The blueberry muffin rash in neonates is a significant clinical finding that often indicates serious underlying conditions, such as congenital infections, hematologic disorders, or metabolic diseases. Early recognition and diagnosis of this rash are crucial, as they guide timely intervention and can improve long-term outcomes for affected infants. The prognostic implications vary widely based on the underlying etiology, necessitating a comprehensive evaluation and multidisciplinary management approach. Ongoing monitoring and support are essential for addressing potential developmental complications, particularly in cases related to TORCH infections. By implementing preventive measures and fostering family education, healthcare providers can mitigate the risks associated with blueberry muffin rash and enhance care for this vulnerable population
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical Consideration
Not applicable.
Data availability
Data that supports the findings of this study are embedded within the manuscript which is based on a comprehensive literature search conducted on October 2024, in the Medline and Cochrane databases.
Author Contribution
The authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
