Volume 4, Issue 11
November 2024
Clinical Challenges and Solutions in Treating Adult Patients with Severe Dental Crowding
Ayed Ali Alqahtani, Shoroug Khaled Alsulemi, Faris Eid Alqarafi, Samirah Hashim Jabir, Alyaa Hussain Omdah, Elaf Dawood Alshdokhe
DOI: http://dx.doi.org/10.52533/JOHS.2024.41111
Keywords: Severe dental crowding, adult orthodontics, relapse prevention, interdisciplinary care, surgical interventions
Severe dental crowding in adults poses significant challenges due to the lack of skeletal growth potential, pre-existing periodontal conditions, and the complexity of achieving both aesthetic and functional goals. Accurate diagnosis involves detailed assessments of occlusion, tooth alignment, and periodontal health, supported by advanced imaging modalities such as CBCT and digital orthodontic planning. Treatment strategies often require balancing non-extraction techniques, such as interproximal reduction and arch expansion, with extraction-based approaches to achieve optimal space management while maintaining facial aesthetics. Orthodontic options, including fixed appliances and clear aligners, are tailored to individual needs, with fixed appliances offering greater control in complex cases. Adjunctive surgical interventions, such as corticotomies and orthognathic procedures, enhance treatment outcomes in severe cases by creating additional space and addressing skeletal discrepancies. Temporary anchorage devices further expand the scope of orthodontic treatments by enabling precise and controlled tooth movement. Long-term maintenance strategies focus on preventing relapse, which is a common challenge in adult cases. Fixed retainers provide reliable stability but require meticulous oral hygiene to prevent complications. Removable retainers offer flexibility but depend heavily on patient compliance. Adjunctive periodontal procedures, such as fiberotomy, and patient education on retainer care enhance long-term success. This multifaceted approach emphasizes the importance of personalized, interdisciplinary care in managing severe dental crowding. Advances in digital orthodontics, surgical techniques, and retention protocols continue to improve outcomes, ensuring both functional and aesthetic benefits while minimizing relapse risks. The integration of innovative tools and strategies offers promising avenues for further advancements in the management of this complex condition.
Introduction
Severe dental crowding in adults presents a significant clinical challenge, often resulting from genetic, environmental, or developmental factors that impede proper tooth alignment. This condition is associated with functional and aesthetic concerns, including impaired mastication, speech difficulties, and diminished self-esteem due to compromised dental aesthetics. Additionally, dental crowding can increase the risk of periodontal disease, dental caries, and temporomandibular joint disorders due to difficulty in maintaining adequate oral hygiene (1, 2). Addressing these challenges requires a multidisciplinary approach that integrates orthodontic, restorative, and sometimes surgical strategies to optimize outcomes. The complexity of treating severe dental crowding in adults stems from factors such as reduced skeletal growth potential, limited periodontal adaptability, and the presence of restorative or prosthetic work. Unlike pediatric cases, where skeletal modifications can be harnessed during growth phases, adult treatments are constrained by the need for non-growth-dependent solutions. Furthermore, adults often seek minimally invasive and aesthetic solutions, prioritizing treatments that align with their personal and professional lifestyles (3).
In recent years, advances in orthodontics and surgical techniques have expanded the options available for managing severe crowding in adults. Innovations such as clear aligners, temporary anchorage devices, and digital orthodontic planning have made treatment more precise and patient friendly. Similarly, interdisciplinary approaches involving periodontics and restorative dentistry have been emphasized to ensure long-term stability and functionality of outcomes (4). Despite these advances, challenges persist, including patient compliance, treatment duration, and the risk of relapsing, necessitating ongoing research and refinement of strategies. This review explores the clinical challenges and solutions in managing severe dental crowding in adults.
Review
The treatment of severe dental crowding in adults remains a challenging endeavor due to the multifactorial nature of the condition and the limitations inherent in adult orthodontics. Unlike younger patients, adults lack the skeletal growth potential necessary for significant structural modifications, necessitating a reliance on dental compensations, extractions, or adjunctive surgical procedures. Orthodontic solutions, such as clear aligners and fixed appliances, have been widely employed to address crowding, but these approaches require meticulous planning to avoid complications such as root resorption and periodontal compromise (5). The introduction of temporary anchorage devices (TADs) has provided a novel means of achieving controlled tooth movement in complex cases, thereby reducing dependence on patient compliance.
Surgical options, including corticotomies and orthodontic extractions, are often considered for severe cases where orthodontics alone is insufficient. These procedures, when performed in conjunction with orthodontic treatment, can significantly reduce treatment time and improve outcomes. However, they carry inherent risks, such as post-operative complications and patient apprehension (6). Long-term success is heavily reliant on effective retention protocols to minimize relapse, a common issue in adult cases. The integration of multidisciplinary approaches, including restorative and periodontal interventions, is essential to ensure both aesthetic and functional outcomes in these challenging cases.
Diagnostic Complexities in Severe Dental Crowding
Severe dental crowding in adults demands a comprehensive and multifaceted diagnostic approach. Accurate diagnosis begins with a detailed patient history to identify underlying causes such as genetic predisposition, childhood habits like thumb-sucking, or traumatic dental injuries that may have altered occlusal development. Clinical examination plays a critical role, where factors such as the degree of crowding, malocclusion type, and presence of compensatory tooth movements must be thoroughly evaluated. Adult patients often present with unique diagnostic challenges due to pre-existing dental restorations, periodontal conditions, or tooth loss, which complicate treatment planning and execution (7).
Advanced imaging techniques have transformed the diagnostic landscape for dental crowding. Cone-beam computed tomography (CBCT) provides high-resolution, three-dimensional imaging, allowing for precise assessment of tooth positioning, root angulations, and spatial relationships. Such imaging is especially useful in cases where crowding is accompanied by impacted or supernumerary teeth, as it offers unparalleled detail for surgical planning. Additionally, digital models and orthodontic software facilitate virtual treatment simulations, enabling clinicians to predict outcomes and identify potential challenges (8). Crowded teeth are often associated with increased plaque accumulation and compromised oral hygiene, leading to an elevated risk of gingivitis and periodontitis. Periodontal probing and radiographic analysis are essential to gauge the extent of bone loss or soft tissue recession. Adults with advanced periodontal disease may require pre-treatment interventions such as scaling, root planing, or regenerative procedures to stabilize the dentition before orthodontic therapy can commence (9). Furthermore, periodontal considerations directly influence the choice of treatment, as excessive forces applied during orthodontic correction can exacerbate bone resorption and jeopardize tooth stability.
Occlusal analysis is equally critical in diagnosing severe crowding. Functional assessments, including evaluation of temporomandibular joint (TMJ) health, are necessary to identify occlusal interferences or parafunctional habits such as bruxism. These factors can significantly affect the feasibility of orthodontic interventions and the longevity of treatment outcomes. Diagnosing occlusal discrepancies often requires articulator-mounted models, which allow for dynamic simulation of mandibular movements. Such detailed analyses can reveal hidden occlusal challenges, helping to refine the treatment strategy (10).
Psychological and aesthetic considerations also form an integral part of diagnosis. Adults often present with heightened expectations regarding treatment aesthetics and outcomes, which can influence their acceptance of traditional orthodontic appliances or extraction-based approaches. Understanding patient priorities and apprehensions through detailed consultations is essential in tailoring treatment options that align with their lifestyle and preferences. Severe crowding diagnosis is a meticulous process requiring a holistic evaluation of dental, periodontal, and functional parameters, supported by advanced imaging and patient-specific considerations. This structured approach lays the foundation for successful treatment planning.
Treatment Planning: Balancing Aesthetics and Functionality
Treatment planning for severe dental crowding in adults involves a careful balancing act between achieving optimal aesthetics and preserving or enhancing functionality. This process begins with a comprehensive analysis of the patient’s occlusion, dental health, and aesthetic goals. Adult patients often seek discreet treatment options that minimize social or professional disruptions, which has led to increased popularity of clear aligners and lingual braces as alternatives to traditional orthodontic appliances. However, these options may not be suitable for all cases, particularly those involving extreme crowding or significant skeletal discrepancies, necessitating a blend of different modalities (11).
A major consideration in treatment planning is whether to preserve or extract teeth. While non-extraction approaches are preferred by many due to their aesthetic appeal and patient acceptability, they are often limited by the degree of crowding and arch space available. Interproximal reduction, arch expansion, or distalization techniques are commonly employed in these scenarios, but their success depends on individual anatomical factors such as arch form and alveolar bone support. On the other hand, extraction-based treatment may provide superior outcomes in cases where severe crowding cannot be resolved by conservative methods. The decision to extract is influenced not only by crowding severity but also by considerations such as facial profile, lip support, and overall harmony of the soft tissues (12). Functional assessments are critical to ensure that the treatment plan does not compromise masticatory efficiency or lead to long-term complications such as temporomandibular joint disorders. This often requires detailed occlusal analysis to identify and eliminate interferences while planning for proper intercuspation. Achieving a stable occlusion becomes even more challenging in adult patients who may already exhibit significant wear, missing teeth, or restorations. In such cases, an interdisciplinary approach involving restorative and prosthetic specialists may be necessary to restore both form and function (13).
Advances in digital orthodontics have significantly enhanced treatment planning precision. Three-dimensional imaging and virtual treatment simulations allow clinicians to visualize various treatment outcomes and share these simulations with patients. These tools are particularly useful in balancing aesthetics and functionality by enabling precise predictions of tooth movements, arch form adjustments, and final smile design. They also facilitate patient involvement in the planning process, fostering better compliance and satisfaction. Digital workflows are further complemented by the use of customized appliances, such as patient-specific brackets or aligners, which enhance treatment efficiency and accuracy (14).
The integration of surgical interventions may also play a role in treatment planning for severe cases. Procedures such as corticotomies or surgically assisted orthodontic expansion can significantly expedite tooth movement and reduce treatment duration. Additionally, orthognathic surgery may be indicated in cases where skeletal discrepancies contribute to crowding. While such surgical options add complexity and potential risks to treatment, they offer a means to achieve superior outcomes in terms of both aesthetics and functionality, especially in patients with severe skeletal or dental imbalances.
Orthodontic and Surgical Interventions: Approaches and Limitations
The management of severe dental crowding in adults often necessitates a combination of orthodontic and surgical interventions, particularly when traditional orthodontic techniques alone are insufficient to achieve optimal results. Orthodontic approaches are generally the first line of treatment, with fixed appliances and clear aligners being the most commonly employed tools. Fixed appliances offer superior control over tooth movement, making them particularly useful in cases involving complex crowding or significant root angulation issues. However, their aesthetic limitations often lead patients to seek alternatives like clear aligners, which, while more discreet, may lack the biomechanical force necessary for severe corrections. The choice between these options depends on the extent of crowding, patient preferences, and treatment goals (15).
Surgical interventions are often considered when orthodontic measures alone cannot address the underlying skeletal or dental discrepancies contributing to crowding. One commonly utilized technique is corticotomy-assisted orthodontics, which accelerates tooth movement by inducing a transient state of bone remodeling. This approach not only shortens treatment time but also increases the feasibility of addressing severe crowding without extractions. Despite these advantages, corticotomies carry risks such as post-operative discomfort, swelling, and the potential for periodontal complications if not executed with precision (16).
Orthognathic surgery represents a more invasive yet highly effective solution for cases involving significant skeletal discrepancies. This approach is particularly valuable in patients whose crowding is compounded by jaw size imbalances or malocclusions that cannot be corrected through dental compensation alone. Procedures such as maxillary expansion, mandibular setback, or advancement can create the necessary space to realign crowded teeth and establish a harmonious facial profile. However, the invasive nature of orthognathic surgery, coupled with its associated costs and recovery period, often makes it a last-resort option, reserved for patients who have exhausted other less invasive alternatives (17).
TADs have emerged as a valuable adjunct to both orthodontic and surgical approaches, offering a minimally invasive means of achieving anchorage in challenging cases. These devices provide a fixed point of support that enables precise tooth movement without relying on patient compliance or auxiliary appliances. TADs have been particularly effective in managing posterior intrusion, molar distalization, and other movements essential for creating space in crowded arches. However, their use is not without limitations, as they require surgical placement and carry the risk of failure or patient discomfort if improperly managed (18).
Long-Term Maintenance and Relapse Prevention Strategies
Ensuring the long-term stability of orthodontic outcomes in adult patients with severe dental crowding remains a formidable challenge. Relapse, characterized by the partial or complete return of the initial malocclusion, is a common concern, particularly in cases where significant tooth movements or extractions have been employed. A well-designed retention strategy is critical to minimizing the risk of relapse and maintaining the functional and aesthetic benefits achieved through treatment. Retention plans must be tailored to the individual, taking into account factors such as the extent of initial crowding, periodontal health, and patient compliance (19).
Fixed retainers are widely used for their reliability in maintaining alignment, particularly in the mandibular anterior region, where relapse rates are notoriously high. These retainers, typically bonded to the lingual surfaces of the teeth, provide continuous support and require minimal patient intervention. However, they are not without drawbacks. Fixed retainers can complicate oral hygiene, increasing the risk of plaque accumulation and gingivitis if not properly maintained. Regular professional monitoring and meticulous oral care are essential to mitigate these risks (20). Removable retainers, such as Hawley or vacuum-formed devices, are another option, offering flexibility in wear schedules and ease of cleaning. These retainers are especially useful in cases where patient compliance is high, as they allow for periods of relief from wear while still maintaining alignment. Yet, their reliance on patient adherence can be a double-edged sword; inconsistent use often leads to relapse. Moreover, they may not provide the same level of stability as fixed retainers for certain tooth movements, particularly rotations or diastema closures (21).
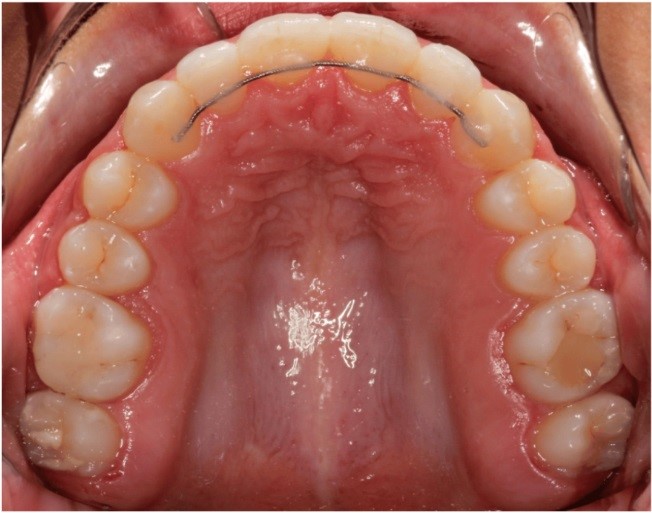
Figure 1: Example of a fixed permanent retainer at the upper canine to canine flexible cylindrical wire (22).
Adjunctive therapies are increasingly being explored as a means to enhance retention and reduce relapse risks. Periodontal considerations play a significant role in this context, as weakened periodontal structures are less capable of withstanding occlusal forces, thereby predisposing to relapse. Procedures such as gingival fiberotomy, performed during or after orthodontic treatment, have shown promise in reducing relapse by severing the elastic fibers that contribute to tooth rebound. While effective, this procedure is not universally applicable and is often reserved for cases involving significant rotations or crowding (23). Behavioral strategies and patient education also form a cornerstone of relapse prevention. Educating patients about the importance of long-term retention, proper retainer care, and regular follow-up visits enhances compliance and facilitates early intervention in case of relapse signs. Clinicians must emphasize that retention is a lifelong process for many individuals, particularly those treated for severe crowding. Periodic check-ups allow for adjustments to retention protocols as needed, ensuring sustained success in maintaining dental alignment.
Conclusion
In treating severe dental crowding in adults, a multidisciplinary approach is essential to address the complex interplay of aesthetic, functional, and periodontal factors. Accurate diagnosis, personalized treatment planning, and a combination of orthodontic and surgical interventions are pivotal for successful outcomes. Long-term retention strategies are crucial to maintaining alignment and preventing relapse. Ongoing research and innovation continue to refine these approaches, offering hope for even more effective and patient-centered solutions.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical Consideration
Not applicable.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author Contribution
The authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
