Volume 4, Issue 9
September 2024
The Role of Immunotherapy in Managing Chronic Respiratory Conditions with Infectious Etiologies
Nashwa Mohammad Alkhotani, Mohammad Saud Khoj, Najwa Essa Almahfoudh, Ghofran Naji Alshammer, Nawaf Khalid Andijani, Tawfiq Ali Shihab, Abdulmalik Muhammed Alamro
DOI: http://dx.doi.org/10.52533/JOHS.2024.40910
Keywords: Chronic respiratory conditions, Immunotherapy, Chronic infections, Vaccines, Monoclonal antibodies, Cystic fibrosis, Chronic obstructive pulmonary disease
Chronic respiratory conditions with infectious etiologies encompass a range of diseases where long-term respiratory issues arise due to persistent or recurrent infections. These conditions, including Chronic Obstructive Pulmonary Disease (COPD), bronchiectasis, tuberculosis (TB), cystic fibrosis (CF), chronic fungal infections, and nontuberculous mycobacterial (NTM) infections, severely impact the quality of life and require ongoing medical management. Traditional management involves antibiotic and antifungal therapies, pulmonary rehabilitation, vaccination, airway clearance techniques, and lifestyle modifications. Immunotherapy has emerged as a promising adjunctive approach, significantly enhancing the immune response to persistent infections, reducing chronic inflammation, and improving overall outcomes. This review explores specific immunotherapies, including vaccines, monoclonal antibodies, allergen-specific immunotherapy, and cytokine therapies, detailing their roles in managing chronic respiratory conditions and highlighting the potential of personalized and combination therapies. The integration of immunotherapy into standard clinical practice holds the potential to transform the management of these challenging conditions.
Introduction
Chronic respiratory conditions with infectious etiologies encompass a range of diseases where long-term respiratory issues arise due to persistent or recurrent infections. These conditions can severely impact the quality of life and may require ongoing medical management. Some of the most common chronic respiratory conditions with infectious etiologies include Chronic Obstructive Pulmonary Disease (COPD), which is often caused by repeated infections, particularly from bacteria such as Haemophilus influenzae, Streptococcus pneumoniae, and Moraxella catarrhalis, with viral infections also playing a role (1). COPD is characterized by chronic bronchitis and emphysema, leading to difficulty in breathing, frequent respiratory infections, and reduced airflow (2). Bronchiectasis, another chronic condition, is caused by chronic bacterial infections leading to permanent dilation and damage of the bronchial walls, with common pathogens including Pseudomonas aeruginosa and Mycobacterium avium complex (3). This condition is characterized by chronic cough, production of large amounts of sputum, recurrent lung infections, and airway obstruction.
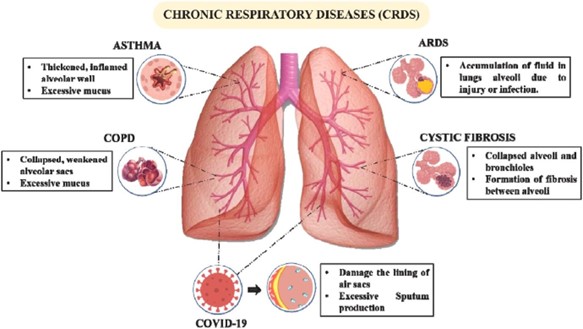
Tuberculosis (TB), caused by Mycobacterium tuberculosis, can lead to chronic lung damage and persistent respiratory issues if not properly treated (4). Symptoms include a persistent cough, hemoptysis (coughing up blood), chest pain, night sweats, and weight loss. Cystic Fibrosis (CF) is a genetic disorder that leads to the production of thick, sticky mucus that can trap bacteria, causing repeated lung infections (5). Common pathogens include Pseudomonas aeruginosa and Staphylococcus aureus, and the condition is characterized by a chronic cough, recurrent lung infections, bronchiectasis, and progressive lung damage. Chronic fungal infections, caused by fungal pathogens like Aspergillus spp., can result in conditions such as chronic pulmonary aspergillosis (CPA) or allergic bronchopulmonary aspergillosis (ABPA), with symptoms including a persistent cough, wheezing, hemoptysis, and weight loss (6). These conditions often affect individuals with pre-existing lung diseases. Nontuberculous Mycobacterial (NTM) infections, caused by mycobacteria other than Mycobacterium tuberculosis, such as Mycobacterium avium complex (MAC), can lead to chronic respiratory symptoms, including chronic cough, fatigue, weight loss, and recurrent lung infections (7) (Figure 1).
Figure 1: Various chronic respiratory diseases (8)
Review
Management and treatment of these chronic respiratory conditions typically involve long-term or recurrent antibiotic treatments to control bacterial infections and antifungal therapy for chronic fungal infections (9). Pulmonary rehabilitation, including exercise and education programs, helps improve lung function and quality of life. Preventive vaccines against common respiratory pathogens are also essential. Airway clearance techniques are employed to help clear mucus from the lungs, and lifestyle modifications, such as smoking cessation, a healthy diet, and avoiding exposure to pollutants, are recommended (10).
Immunotherapy has emerged as a promising approach in managing these conditions by modulating the immune system to enhance the body's ability to fight infections and reduce chronic inflammation (11) (Figure 2). Specific immunotherapies, such as vaccines, monoclonal antibodies targeting inflammatory pathways, and allergen-specific immunotherapy, play a crucial role in improving outcomes. For instance, in COPD, monoclonal antibodies like benralizumab reduce eosinophilic inflammation (12), while in cystic fibrosis, CFTR modulators correct defective protein function, improving immune responses (13). Additionally, host-directed therapies in tuberculosis enhance the immune response to infection (14). Overall, early diagnosis and appropriate treatment, including immunotherapy, are crucial in managing these chronic respiratory conditions and preventing further complications. Immunotherapy encompasses several critical roles and applications, each with specific scientific underpinnings and clinical examples.
Immunotherapy can significantly enhance the immune response to persistent infections that contribute to chronic respiratory conditions. This enhancement can be achieved through the development and use of vaccines targeting specific pathogens. For example, the Bacillus Calmette-Guérin (BCG) vaccine is traditionally used to prevent tuberculosis (TB) and is being explored as a potential immunotherapeutic agent to boost immune responses against Mycobacterium tuberculosis (15). Studies have shown that the BCG vaccine can induce a broad, non-specific activation of the immune system, which can enhance the body's ability to fight off a range of pathogens, including those causing chronic respiratory conditions.
Additionally, adjuvants play a crucial role in enhancing the efficacy of vaccines. Adjuvants like aluminum salts (alum) and oil-in-water emulsions are used to stimulate stronger and more prolonged immune responses (16). These substances work by creating a depot effect at the injection site, slowly releasing the antigen and providing continuous stimulation to the immune system. This prolonged exposure helps to generate a robust and long-lasting immune response, which is particularly beneficial in managing chronic infections.
The ongoing development of vaccines against Pseudomonas aeruginosa, a common pathogen in cystic fibrosis (CF) patients, further exemplifies the potential of immunotherapy (17). Pseudomonas aeruginosa is notorious for its resistance to antibiotics and its ability to form biofilms, which protect it from the host immune response and antimicrobial treatments. Vaccine development against this pathogen aims to elicit a strong and specific immune response that can prevent infection or reduce its severity, thereby improving the quality of life for CF patients.
Research into vaccines for Pseudomonas aeruginosa includes multiple approaches. One approach is the use of outer membrane proteins and lipopolysaccharides as antigens to stimulate a targeted immune response (18). Another strategy involves the use of attenuated or inactivated forms of the bacteria to induce immunity without causing disease. Additionally, conjugate vaccines, which link polysaccharides to proteins, are being explored to enhance immunogenicity and provide better protection against the pathogen.
Furthermore, advancements in mRNA vaccine technology, exemplified by the rapid development and deployment of COVID-19 vaccines, offer new possibilities for creating effective vaccines against chronic respiratory pathogens (19). mRNA vaccines can be designed to encode specific antigens from pathogens like Pseudomonas aeruginosa, enabling the host cells to produce these antigens and stimulate a robust immune response.
In chronic respiratory conditions such as COPD and bronchiectasis, immunotherapeutic vaccines targeting common bacterial pathogens like Haemophilus influenzae and Streptococcus pneumoniae are also under investigation (20). These vaccines aim to reduce the frequency and severity of respiratory exacerbations, which are often triggered by bacterial infections. Overall, the development and use of vaccines in immunotherapy represent a powerful strategy to enhance the immune response to persistent infections in chronic respiratory conditions. This approach not only aims to prevent infections but also to reduce the burden of chronic diseases by improving the body's natural defense mechanisms. As research and technology continue to advance, the potential for vaccines to transform the management of chronic respiratory conditions becomes increasingly promising.
Reducing chronic inflammation, a hallmark of many respiratory diseases, is another crucial role of immunotherapy. Monoclonal antibodies targeting specific inflammatory pathways or cytokines are at the forefront of this approach (21). For instance, mepolizumab and benralizumab, which target interleukin-5 (IL-5), are used in the treatment of severe eosinophilic asthma to reduce eosinophil counts and inflammation (22). Similarly, dupilumab, targeting IL-4 and IL-13 pathways, has shown efficacy in reducing inflammation in patients with asthma and chronic rhinosinusitis with nasal polyps (23). Tumor necrosis factor-alpha (TNF-alpha) inhibitors, such as infliximab and adalimumab, have been explored for their anti-inflammatory effects in conditions like sarcoidosis, a chronic granulomatous disease affecting the lungs (24).
Immunotherapy also modulates immune tolerance in conditions characterized by hypersensitivity or autoimmunity. Allergen-specific immunotherapy (AIT), such as subcutaneous or sublingual administration of allergen extracts, is employed in conditions like allergic bronchopulmonary aspergillosis (ABPA) to desensitize the immune system to fungal antigens (25). Regulatory T cells (Tregs) play a pivotal role in maintaining immune tolerance, and therapies aimed at expanding Treg populations, such as low-dose interleukin-2 (IL-2) therapy, are being investigated to manage chronic inflammatory lung diseases (25).
Enhancing mucosal immunity is another vital role of immunotherapy, given that the mucosal surfaces of the respiratory tract are primary barriers against pathogens. Mucosal vaccines, administered via the nasal route, are designed to elicit strong local immune responses (26). For example, the live attenuated influenza vaccine (LAIV) administered intranasally induces robust mucosal immunity, providing enhanced protection against respiratory viruses (27). Immunomodulatory agents like probiotics and oral immunoglobulin preparations aim to boost mucosal immune responses by increasing the production of secretory immunoglobulin A (IgA), which plays a crucial role in neutralizing pathogens at mucosal surfaces (28).
Specific chronic respiratory conditions are addressed through tailored immunotherapeutic interventions. In COPD, alpha-1 antitrypsin (AAT) replacement therapy is crucial for patients with AAT deficiency, which predisposes them to emphysema and chronic bronchitis (29). Roflumilast, a phosphodiesterase-4 inhibitor, is used to reduce inflammation and exacerbations in severe COPD (30). Monoclonal antibodies like benralizumab, targeting the IL-5 receptor, reduce eosinophilic inflammation in COPD patients with elevated eosinophil counts. For bronchiectasis, immunoglobulin replacement therapy is indicated for patients with primary immunodeficiencies to prevent recurrent infections. Inhaled antibiotics, such as tobramycin and aztreonam, are used to manage chronic bacterial infections and reduce inflammation. Interferon gamma therapy enhances the microbicidal activity of macrophages and neutrophils in patients with chronic granulomatous disease (CGD), which can lead to bronchiectasis (31).

Figure 2: The emergence of immunotherapy as a potential therapeutic intervention for bacterial infection.
In cystic fibrosis (CF), CFTR modulators like ivacaftor, lumacaftor, tezacaftor, and elexacaftor correct the defective CFTR protein function, thereby improving chloride transport and reducing mucus viscosity (32). Inhaled antibiotics like tobramycin, colistin, and aztreonam, along with mucolytics such as dornase alfa, are critical in managing chronic infections and improving mucus clearance (33). Azithromycin is used for its immunomodulatory effects, reducing inflammation and infection frequency. For tuberculosis (TB), host-directed therapies aim to enhance the host's immune response to the infection (34). Statins, known for their anti-inflammatory properties, and metformin, which modulates metabolism and immune responses, are being explored as adjunctive treatments in TB management (35). Interleukin-2 (IL-2) therapy enhances T-cell responses to control and clear TB infection.
Chronic fungal infections also benefit significantly from immunotherapeutic approaches, which aim to enhance the body's immune response to persistent fungal pathogens and reduce the inflammation associated with these infections. Antifungal immunotherapies, such as itraconazole and voriconazole, are pivotal in managing chronic fungal infections (36). These antifungal agents work by inhibiting the synthesis of ergosterol, a critical component of fungal cell membranes, thereby reducing the fungal burden and alleviating infection-related inflammation. Itraconazole, in particular, is often used in the treatment of chronic pulmonary aspergillosis (CPA), where it helps to control fungal growth and improve respiratory symptoms. As mentioned earlier, AIT is another important immunotherapeutic approach, especially in managing allergic bronchopulmonary aspergillosis (ABPA) (25). ABPA is a condition where the immune system exhibits hypersensitivity to Aspergillus antigens, leading to severe allergic reactions and chronic lung damage. AIT involves the administration of gradually increasing doses of Aspergillus antigens to desensitize the immune system. This process reduces hypersensitivity reactions and associated inflammation, improving respiratory function and reducing the frequency and severity of exacerbations. Monoclonal antibodies like omalizumab are also instrumental in managing conditions like ABPA (37). Omalizumab targets immunoglobulin E (IgE), a key player in allergic responses. By binding to IgE, omalizumab prevents it from interacting with its receptors on mast cells and basophils, thereby inhibiting the release of inflammatory mediators. This action reduces allergic responses and inflammation in patients with ABPA, leading to better control of symptoms and fewer respiratory complications. In addition to omalizumab, other monoclonal antibodies are being explored for their potential in treating chronic fungal infections and associated allergic conditions. For instance, benralizumab, which targets the IL-5 receptor, has shown promise in reducing eosinophilic inflammation in severe asthma and could potentially be applied to similar inflammatory pathways in fungal infections (38). Furthermore, research is ongoing into the use of cytokine therapies to modulate immune responses in chronic fungal infections. Interferon-gamma therapy, for example, enhances the microbicidal activity of macrophages and neutrophils, improving the body's ability to control fungal infections (39). This therapy is particularly relevant in patients with chronic granulomatous disease (CGD), who are prone to severe fungal infections due to their compromised immune function. Despite the promising potential of immunotherapy, several challenges and future directions remain. Personalized medicine aims to tailor immunotherapy based on individual patient profiles and specific pathogens involved, leveraging genomic and proteomic data to customize treatments (40). Combination therapies that integrate immunotherapy with traditional antibiotics or antifungals offer synergistic effects for more effective treatment (41). Ongoing research and development are crucial to better understanding the immune mechanisms involved in chronic respiratory conditions and to develop new immunotherapeutic agents.
Overall, immunotherapy holds significant potential in managing chronic respiratory conditions with infectious etiologies, offering new avenues for treatment and improved patient outcomes. As research progresses, the integration of immunotherapy into standard clinical practice is expected to transform the management of these challenging conditions.
Conclusion
Immunotherapy offers a transformative approach to managing chronic respiratory conditions with infectious etiologies by enhancing immune responses and reducing inflammation. Vaccines targeting pathogens like Mycobacterium tuberculosis and Pseudomonas aeruginosa, along with monoclonal antibodies such as omalizumab and benralizumab, play crucial roles. Allergen-specific immunotherapy and cytokine therapies provide additional benefits. Integrating immunotherapy into clinical practice, alongside personalized and combination therapies, holds great promise for improving the management and outcomes of these chronic conditions.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable
Consent for publications
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.