Volume 4, Issue 8
August 2024
Non-adherence to Medication and Associated Factors Among Type 2 Diabetes: Systematic Review
Sakinah Hassan Alzaher
DOI: http://dx.doi.org/10.52533/JOHS.2024.40806
Keywords: non-adherence, medication, diabetes, association, significant
Non-adherence to medication among Type 2 diabetes mellitus (T2DM) patients is a complex and multifactorial issue, with various contributing factors. Patient-related factors such as socioeconomic status, health literacy, beliefs and attitudes toward medication, and psychosocial factors like depression, anxiety, and stress can all play a role. Healthcare system-related factors can also contribute to non-adherence. A systematic review was conducted to identify and synthesize the available evidence on non-adherence to medication and related factors among T2DM patients. Included studies that report medication non-compliance and related variables in T2DM individuals were used. Excluded studies had non-original investigations, non-human investigations, incomplete data, and abstract-only articles. Electronic databases were searched and eligible studies were selected. Data extraction was conducted independently by two researchers and quality assessment was performed using standardized tools. The search identified 8 studies involving 2030 patients published from 2009 to 2024. These studies revealed varied rates of medication non-adherence ranging from 10.3% to 77.3%. The research showed diverse findings, indicating that older age consistently acts as a protective factor against non-adherence, particularly among individuals aged over 60. Only one study indicated a significant association with male gender. Education level yielded mixed results. Additionally, one study highlighted a significant relationship between depressive symptoms and non-adherence. Employment status exhibited varying associations. Overall, these findings highlight the complex interplay of demographic and treatment-related factors influencing adherence to diabetic medication. The studies reviewed revealed wide-ranging rates of non-adherence, illustrating a significant challenge in managing this chronic condition effectively. These findings underscore the need for personalized approaches in diabetes management, addressing not only clinical factors but also socio-demographic and psychological influences to improve medication adherence and ultimately health outcomes for patients. Future research should focus on comprehensive strategies that integrate these diverse factors to optimize treatment adherence in individuals with T2DM.
Introduction
Type 2 diabetes mellitus (T2DM) is a chronic metabolic disorder characterized by hyperglycemia and insulin resistance (1). This global public health problem is becoming increasingly prevalent worldwide, with an estimated 463 million people affected in 2019. This number is projected to increase to 700 million by 2045 (2). T2DM is linked to significant morbidity, mortality and healthcare costs due to complications including cardiovascular disease, neuropathy, nephropathy and retinopathy (3, 4). Although there is no cure for T2DM, the condition can be effectively managed through medication, lifestyle modifications and regular monitoring of blood glucose levels.
Medication non-adherence is defined as the failure to follow healthcare professionals' prescribed medication regimen, which includes missed doses, incorrect dosages, and early discontinuation of medication (5). Around half of non-adherence is intentional, while the remaining instances occur because patients are either unaware that they are not taking medications as prescribed, or the regimen is too complex for them (6). The World Health Organization reports that globally, non-adherence to T2DM medication is approximately 50%, with adherence rates likely to be lower in developing countries due to limited resources (7, 8). As such, non-adherence to diabetic treatment varies widely, ranging from 36% to 93% (9, 10). Non-adherence to medication poses a significant barrier to achieving optimal glycemic control and preventing complications in T2DM patients.
Non-adherence to medication among T2DM patients is a complex and multifactorial issue, with various contributing factors. Patient-related factors such as socioeconomic status, health literacy, beliefs and attitudes toward medication, and psychosocial factors like depression, anxiety, and stress can all play a role. Healthcare system-related factors like access to care, communication between healthcare providers and patients, and the complexity of medication regimens can also contribute to non-adherence (11).
Several studies have been conducted to assess the frequency of medication non-adherence among T2DM patients and the factors associated with it. However, the findings of these studies have been inconsistent, with some studies reporting higher rates of non-adherence than others. Additionally, the factors linked to non-adherence have differed across studies, underscoring the importance of a systematic review to consolidate the existing evidence and determine the main factors connected to non-adherence to medication in T2DM patients.
Numerous studies have reported a high prevalence of medication non-adherence in patients with T2DM. A meta-analysis of 13 studies with T2DM and Type 1 diabetes mellitus (T1DM) patients reported that the pooled prevalence of non-adherence to antidiabetic medication was 43.4% (95% CI: 17.5-69.4; P < 0.001) (12) while another meta-analysis of studies conducted in Ethiopia with T2DM and T1DM patients found a pooled prevalence of adherence to the anti-diabetic medication of 69.5% (95% CI: 61.1-78.0) (13). These findings highlight the pressing need to understand the contributing factors of non-adherence.
Multiple factors have been identified as causative agents of medication non-adherence in T2DM patients, with socioeconomic status (SES) being the most cited contributor. Several studies have reported that low SES is associated with reduced medication adherence, particularly among patients with lower income and education levels (14, 15). In general, non-adherence to T2DM medication is typically influenced by a combination of patient-related factors, such as psychosocial and demographic factors, disease-related factors including comorbidities, blood glucose monitoring, and complications, as well as factors related to the medical system (16, 17). Comorbidities were found to be significantly associated with medication non-adherence by Piparva et al. (18). In Saudi Arabia, a systematic review identified various factors associated with medication non-adherence among diabetic patients. These factors included forgetting to take medication doses, medication complexity resulting from multiple drugs and regimens, medication side effects, belief in the ineffectiveness of medication, and discontinuation of medication due to perceived improvement in health (19). Studies have demonstrated that patients who lack social support from family and friends are more likely to be non-adherent to their medication, highlighting the importance of social support in medication adherence (20). Moreover, low health literacy has been recognized as a crucial predictor of medication non-adherence, as studies have demonstrated that individuals with inadequate health literacy are more prone to be non-adherent (21).
Medication non-adherence can have a substantial impact on diabetes management, resulting in suboptimal glycemic control, increased diabetes-related complications, and diminished quality of life (22, 23). It can result in higher healthcare costs, including increased hospitalizations, emergency department visits, and outpatient care (22). Furthermore, non-adherence can affect the mental health of patients, leading to increased stress, anxiety, and depression (24).
The objective of this systematic review is to identify and synthesize the available evidence on non-adherence to medication and related factors among T2DM patients without T1DM patients. The research hypothesis suggests that medication non-adherence in individuals with T2DM is influenced by diverse factors that vary across populations, including socioeconomic status, comorbidities, medication-related factors, lack of social support, and health literacy. To better understand these influences, this review aims to compile and analyze existing studies to provide a comprehensive overview of the determinants of medication non-adherence in T2DM patients.
Material and methods
Definition of outcomes and inclusion criteria
The parameters assessed include study characteristics, demographics, incidence, and factors related to non-adherence to T2DM medication. We included original investigations that meet the following criteria: studies that report on medication non-compliance and related variables in individuals diagnosed with T2DM. Observational study designs (cross-sectional and cohort study designs) collect data prospectively or retrospectively were included. We applied a language restriction. Protocols, theses, and articles that weren’t published in English or with no available English information had been excluded. Case reports of less than five sample sizes and those without descriptive statistics or outcomes also had been excluded from this review. Other exclusion criteria are non-original investigations, non-human investigations, incomplete data, and abstract-only articles.
Search Strategy
The following electronic databases were searched from 2010 to February 2023: PubMed, Science Direct, and Google Scholar. Specific search strings were used, which were modified in accordance with the requirements.
Search strategy for PubMed: (("Type 2 diabetes"[MeSH Terms] OR "Diabetes Mellitus, Type 2"[Title/Abstract] OR "diabetic patients"[Title/Abstract]) AND ("Medication Adherence"[MeSH Terms] OR "Treatment Refusal"[MeSH Terms] OR "Medication non-adherence"[Title/Abstract] OR "Medication non-compliance"[Title/Abstract])) AND ("Risk Factors"[MeSH Terms] OR "Predictors"[MeSH Terms] OR "Associated Factors"[Title/Abstract] OR "Demographic factors"[Title/Abstract] OR "Clinical factors"[Title/Abstract] OR "Social factors"[Title/Abstract] OR "Psychological factors"[Title/Abstract]) AND ("Glycemic Control"[MeSH Terms] OR "Hyperglycemia"[MeSH Terms] OR "Hypoglycemia"[MeSH Terms] OR "Diabetic Complications"[MeSH Terms] OR "Morbidity"[MeSH Terms] OR "Mortality"[MeSH Terms])
Search strategy for other databases: (Type 2 diabetes" OR "Diabetes Mellitus) AND ("Treatment Refusal" OR "Medication non-adherence" OR "Medication non-compliance") AND ("Risk Factors" OR "Predictors" OR "Associated Factors")
Search for other resources
A manual search was performed to search the reference lists of the relevant articles. Review papers and references of the selected studies were hand searched to include the missing articles.
Screening and extraction
The eligibility of potentially relevant papers was assessed by screening the title and abstract. Articles with no relevant titles and keywords were excluded. In the second phase, the abstract and full text of articles were reviewed to include those articles matching the inclusion criteria. Reference management (Endnote X8) used for organizing and assessing the titles and abstracts, as well as for identifying any duplicate entries. The final selection was made based on the predefined selection criteria after a full-text review. One review author initially conducts the literature search and selection process, which was subsequently checked by the other author. Any disagreements were resolved through discussion between the two authors.
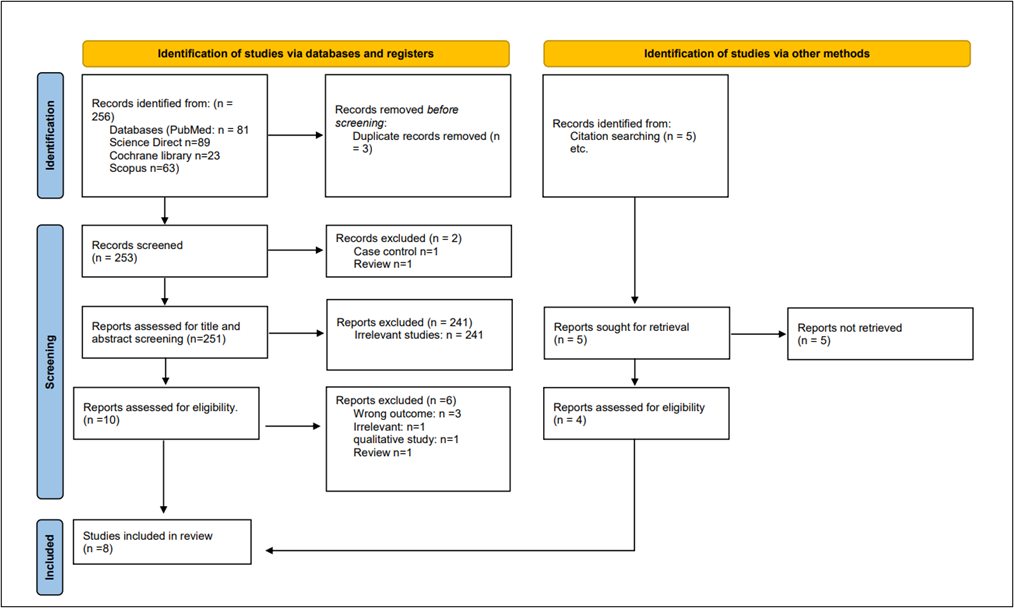
All studies identified by both electronic and manual searches were recorded in a screening sheet, including the reasons for excluding studies. A PRISMA flow chart was prepared to show the study screening process.
Data extraction and management
We used a predetermined standard data extraction form to collect the following information from the selected studies: publication year, study design, country, sample size, and gender distribution characteristics. Additionally, we extracted data on the incidence of non-adherent patients to medication and the influencing factors, such as socio-demographics, healthcare system associated, and other treatment-associated risk factors.
Quality Assessment
In our systematic review, we employed the Newcastle-Ottawa Scale (NOS) (25) as a critical tool for assessing the quality of non-randomized studies included in our analysis. The NOS is widely recognized for its utility in evaluating the methodological quality and risk of bias in observational studies, including cohort and case-control studies. It provides a structured framework for evaluating key aspects of study design, including selection of study groups, comparability, and ascertainment of outcomes. By using the NOS, we were able to systematically appraise the included studies and ensure that only high-quality evidence contributed to our analysis, thereby enhancing the robustness and reliability of our findings.
Results
Search Results
We executed the search methodologies outlined previously, resulting in the identification of a total of 256 citations, subsequently reduced to 253 following the removal of duplicates. Upon screening titles and abstracts, only 14 citations met the eligibility criteria for further consideration. Through full-text screening, this number was further refined to 8 articles (26-33) aligning with our inclusion and exclusion criteria. (Figure 1) provides an in-depth depiction of the search strategy and screening process.
Results of Quality Assessment
The NOS assessment of several studies based on three criteria: Study Selection, Comparability, and Outcome, leading to a Total Score for each. Upon evaluating the quality of the studies included, it was determined that overall, the studies exhibited good quality with minimal risk of bias except one study by Hamalaw et al., 2024, which received the lowest score of 5, primarily due to lower ratings in comparability and outcome (28). Detailed findings of the quality assessment are presented in (Table 1). Overall, this evaluation highlights that while most studies were robust in their selection and outcome measures, there was some variability in how well they controlled confounding variables.
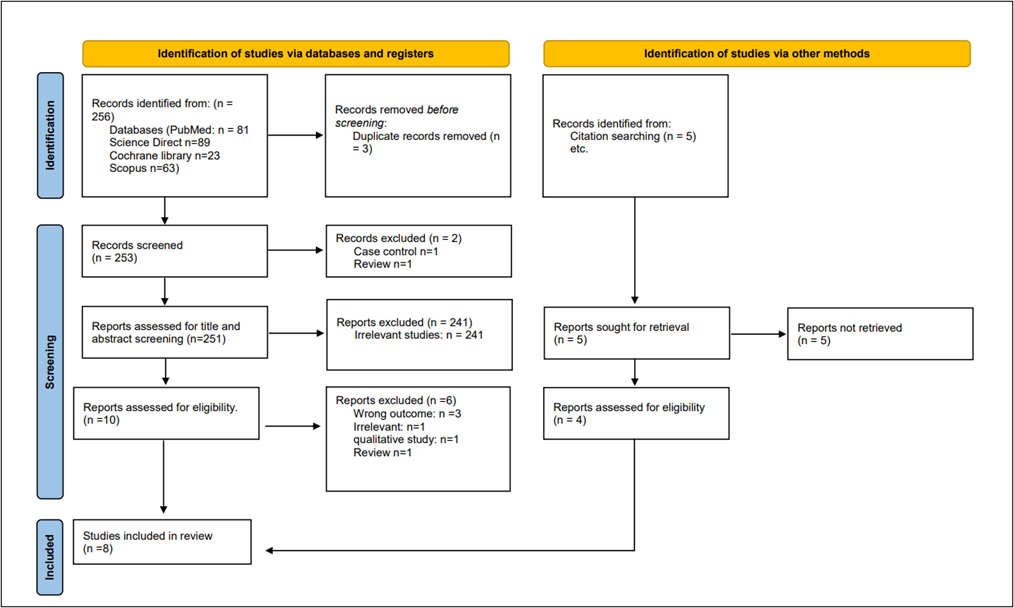
Figure 1: PRISMA flowchart
|
Table 1: Quality assessment of Newcastle–Ottawa scale (NOS) for included studies. |
||||
|
Study |
Selection |
Comparability |
Outcome |
Total Score |
|
Adisa et al., 2009 (26) |
3 |
1 |
2 |
6 |
|
Aminde LN, et al., 2019 (27) |
2 |
2 |
3 |
7 |
|
Hamalaw et al., 2024 (28) |
2 |
1 |
2 |
5 |
|
Horvat et al., 2018 (29) |
3 |
2 |
3 |
8 |
|
Karymsakov et al., 2024 (30) |
3 |
2 |
3 |
8 |
|
Murwanashyaka et al., 2022 (31) |
3 |
2 |
3 |
8 |
|
Saraiva et al., 2020 (32) |
3 |
2 |
3 |
8 |
|
Teklay et al., 2013 (33) |
2 |
2 |
3 |
7 |
Characteristics of the included studies
We incorporated a total of 8 studies encompassing 2030 patients, published between 2009 and 2024. The average age of the participants ranged from 52.4±11.9, with a median age of 61 (ranging from 51.5 to 68.0). Two studies indicated that 5% and 6.19% of the study population fell within the age groups of 18-30 and 30-49 years, respectively. Among the included studies, 41.75% of the study population were male while 56.42% were females. Diverse rates of non-adherence to medication were observed ranging from 10.3% to 77.3%. Notably, all the studies were observational in nature. Geographically, each study was represented by diverse countries including Nigeria, Ethiopia, Bosnia and Herzegovina, Cameroon, Brazil, Rwanda, Iraq and Kazakhstan. A comprehensive summary of the baseline characteristics of these studies can be found in (Table 2). Discrepancies in sample sizes across the included papers likely stem from differences in study objectives and inclusion criteria.
|
Table 2: Baseline characteristics of included studies |
||||||||
|
Author |
Country |
Publication Year |
Study period |
Study design |
Total participants |
Prevalence of non-adherence (%) |
Mean age (years) |
Gender ratio (M/F) |
|
Adisa et al., 2009 (26) |
Nigeria |
2009 |
April to May 2008 |
cross-sectional |
121 |
49.6% |
NR |
49.6%/ 50.4% |
|
Aminde LN, et al., 2019 (27) |
Cameroon |
2019 |
August to September 2016 |
cross-sectional |
195 |
54.4% |
60.5 ± 13.6 |
29.7%/70.3% |
|
Hamalaw et al., 2024 (28) |
Iraq |
2024 |
February to April 2022 |
cross-sectional |
300 |
64% |
57.8±9.95 |
39.7%/60.3% |
|
Horvat et al., 2018 (29) |
Bosnia and Herzegovina |
2018 |
January to December 2015 |
retrospective chart review |
323 |
47.68% |
30–49: 6.19% 50-59:16.41% 60–69: 34.98% >70: 42.41% |
42.11%/57.89% |
|
Karymsakov et al., 2024 (30) |
Kazakhstan |
2024 |
NR |
Questionnaire survey |
324 |
10.3% |
59.08±12.175 |
34.8%/50.6% |
|
Murwanashyaka et al., 2022 (31) |
Rwanda |
2022 |
March to September 2019 |
cross-sectional |
200 |
53.5% |
18–30: 5% 31–50: 35.5% More than 50: 59.5% |
47%/53% |
|
Saraiva et al., 2020 (32) |
Brazil |
2020 |
January to December 2017 |
cross-sectional |
300 |
77.3% |
Median (QR): 61 (51.5–68.0) |
35.7%/64.3% |
|
Teklay et al., 2013 (33) |
Ethiopia |
2013 |
February to April 2011 |
cross-sectional |
267 |
24.3% |
52.4±11.9 |
55.4%/44.6% |
Study outcome measures
The included studies examined several factors that predict non-adherence to medication among individuals with T2DM. A study by Aminde et al. (27) depicted those individuals aged over 60 years had significantly lower odds of non-adherence (adjusted odds ratio [aOR]: 0.44, 95% CI: 0.25 - 0.78, P = 0.02*). Gender, specifically being male, showed no significant association with non-adherence (aOR: 1.07, 95% CI: 0.05 - 2.28, P = 0.81). Regarding education level, there were no significant differences observed in non-adherence rates among those with primary (aOR: 1.71, 95% CI: 0.71 - 4.10), secondary (aOR: 1.58, 95% CI: 0.54 - 4.62), or high school/university education (aOR: 1.60, 95% CI: 0.49 - 5.20, P = 0.52). Regarding the duration of diabetes, individuals with 6-10 years (OR: 2.28, 95% CI: 1.08 - 4.84) or 11-20 years (OR: 1.69, 95% CI: 0.82 - 3.50) did not significantly differ in non-adherence rates compared to those with more than 20 years (OR: 0.53, 95% CI: 0.13 - 2.26, P = 0.22). Although higher odds were observed for individuals having diabetes from 6-10 years (27). While Horvart et al. (29) indicated that age was significantly associated with non-adherence to medication (OR: 0.47, 95% CI: 0.28 - 0.79, P = 0.004*), indicating that older individuals were less likely to be non-adherent. Occupation, including unemployment (OR: 0.88, 95% CI: 0.37 - 2.09, P = 0.773), retirement (OR: 1.20, 95% CI: 0.50 - 2.85, P = 0.682), and receiving disability pension (OR: 1.95, 95% CI: 0.43 - 8.87, P = 0.195), did not show significant associations with non-adherence. Similarly, marital status—single (OR: 1.24, 95% CI: 0.46 - 3.40, P = 0.671), divorced (OR: 1.56, 95% CI: 0.49 - 5.02, P = 0.453), and widowed (OR: 1.39, 95% CI: 0.70 - 2.76, P = 0.354) also did not significantly predict non-adherence. Education level showed a trend towards significance (OR: 0.64, 95% CI: 0.40 - 1.01, P = 0.053), suggesting that higher education might be associated with lower non-adherence rates. Lastly, the duration of diabetes did not significantly influence non-adherence (OR: 1.48, 95% CI: 0.86 - 2.54, P = 0.161) (29).
A multivariate regression analysis performed by Teklay et al. indicated depressive symptoms showed a strong association with non-adherence (aOR: 2.404, 95% CI: 1.323 - 4.366, P = 0.004*), indicating that individuals experiencing depressive symptoms were more likely to be non-adherent to their medication regimen. Other factors contributing to non-adherence included experiencing side effects (aOR: 1.868, 95% CI: 1.012 - 3.446, P = 0.046) and facing a complex medication regimen (aOR: 3.413, 95% CI: 1.652 - 7.05, P = 0.001*). These findings suggest that patients who perceive their treatment as complex or experience side effects are at higher risk of non-adherence. However, factors such as diabetes complications (aOR: 1.569, 95% CI: 0.701 - 3.512, P = 0.273), fasting blood glucose levels (aOR: 1.469, 95% CI: 0.732 - 2.949, P = 0.28), and previous hospitalizations (aOR: 2.42, 95% CI: 1.174 - 4.992, P = 0.017*) did not show significant associations with non-adherence in this analysis (33). Findings of a study by karymsakov et al. demonstrated that age categories showed varying associations with non-adherence to medication among diabetic patients. Specifically, individuals aged 60-69 years ( [OR]: 0.23, 95% CI: 0.08 - 0.71, P = 0.01*) and 70-79 years (OR: 0.19, 95% CI: 0.06 - 0.61, P = 0.006*) had significantly lower odds of non-adherence compared to younger age groups (40-49 years: OR: 0.36, 95% CI: 0.11 - 1.22, P = 0.102; 50-59 years: OR: 0.41, 95% CI: 0.13 - 1.31, P = 0.134). Gender (female) did not significantly influence non-adherence (OR: 0.98, 95% CI: 0.60 - 1.60, P = 0.93), while employment status showed significant associations, with fully employed individuals having higher odds of non-adherence (OR: 2.11, 95% CI: 1.22 - 3.67, P = 0.01*) compared to unemployed (OR: 0.78, 95% CI: 0.33 - 1.89, P = 0.59) or partially employed individuals (OR: 1.83, 95% CI: 0.55 - 6.10, P = 0.32). Marital status and education level did not show significant associations with non-adherence. Specifically, being not married (OR: 2.07, 95% CI: 0.72 - 5.93, P = 0.83), widowed (OR: 0.73, 95% CI: 0.32 - 1.68, P = 0.462), divorced (OR: 1.24, 95% CI: 0.17 - 9.01, P = 0.174), having specialized education (OR: 0.7, 95% CI: 0.25 - 1.94, P = 0.49), bachelor's degree (OR: 1.44, 95% CI: 0.65 - 3.20, P = 0.37), or master's degree (OR: 2.45, 95% CI: 0.83 - 7.20, P = 0.1) did not significantly affect non-adherence rates (30).
Murwanashyaka et al. reported in their study findings age groups did not show significant associations with medication adherence: 18–30 years (OR: 1, P = 0.32), 31–50 years (OR: 2.71, 95% CI: 0.67 - 11.01, P = 0.16), and more than 50 years (OR: 0.9, 95% CI: 0.499 - 1.63, P = 0.73). Gender was significantly associated with medication adherence, with males having higher odds of non-adherence (OR: 1, P = 0.032*) compared to females (OR: 1.85, 95% CI: 1.05 - 3.24, P value not provided). Marital status did not significantly influence medication adherence: single (OR: 1, P = 0.26), married/cohabiting (OR: 2.02, 95% CI: 0.682 - 6.01, P = 0.204), and divorce (OR: 0.96, 95% CI: 0.44 - 2.1, P = 0.917). Duration with diabetes and medications showed varying associations: 1-3 years (OR: 1, P = 0.031*), 4-10 years (OR: 2.18, 95% CI: 1.09 - 4.34, P = 0.027*), and more than 10 years (OR: 1.03, 95% CI: 0.43 - 2.42, P = 0.954). Education level significantly influenced medication adherence: no formal education (OR: 1, P = 0.036*), primary education (OR: 2.87, 95% CI: 1.27 - 6.5, P = 0.012*), and secondary education (OR: 1.834, 95% CI: 0.94 - 3.58, P = 0.075). Employment status also showed significant associations: jobless (OR: 1, P = 0.008**), public employee (OR: 2.36, 95% CI: 1.24 - 4.48, P = 0.009*), and private employee (OR: 0.8, 95% CI: 0.38 - 1.72, P = 0.57) (31). Findings of a study by Adisa et al. observed significant associations with age (P = 0.02*), gender (P = 0.005*), occupation (P = 0.024*) (26). A study by Saraiva et al. compared pharmacotherapy factors between low and high adherence groups among which only anti-diabetic therapy was the significant factor, patients receiving metformin were observed more likely to be adherent (32). Hamalaw et al. observed association between patient behavior and beliefs regarding diabetes medication adherence. Higher prevalence of non-adherence was reported among those who self-modify their drug doses (p=00.042) and those who adjust the timing of their anti-diabetic medication (28). Overall, the findings highlight the multifaceted nature of non-adherence to diabetic medication, with various demographic and treatment-related factors playing significant roles (Table 3).
|
Table 3: Outcome measures of included studies |
||
|
Study |
Method of Measurement |
Findings |
|
Adisa et al., 2009 (26) |
Chi square |
- Age: (chi square: 5.40, P-value: 0.02*) - Gender: (chi square: 14.85, P-value: 0.005*) - Occupation: (chi square: 5.08, P-value: 0.024*) - Marital Status: (chi square: 2.30, P-value: 0.513) |
|
Aminde et al., 2019 (27) |
Adjusted multivariable logistic regression and bivariate analysis |
- Age: > 60 years (aOR: 0.44, 95% CI: 0.25 - 0.78, P: 0.02*) - Gender: Male: (aOR: 1.07, 95% CI: 0.05 - 2.28, P: 0.81) - Education: Primary: (aOR: 1.71, 95% CI: 0.71 - 4.10) Secondary: (aOR: 1.58, 95% CI: 0.54 - 4.62) High school/University: (aOR: 1.60, 95% CI: 0.49 - 5.20, P: 0.52) - Duration of Diabetes: 6–10 years: (OR: 2.28, 95% CI: 1.08 - 4.84) 11-20 years: (OR: 1.69, 95% CI: 0.82 - 3.50) > 20 years: (OR: 0.53, 95% CI: 0.13 - 2.26, P: 0.22) |
|
Hamalaw et al., 2024 (28) |
Chi square |
Higher prevalence of non-adherence was reported among those who self-modify their drug doses (p=00.042) and those who adjust the timing of their anti-diabetic medication |
|
Horvat et al., 2018 (29) |
Multivariate logistic regression |
- Age: (OR: 0.47, 95% CI: 0.28 - 0.79, P: 0.004*) - Occupation: Unemployed: (OR: 0.88, 95% CI: 0.37 - 2.09, P: 0.773) Retired: (OR: 1.20, 95% CI: 0.50 - 2.85, P: 0.682) Disability pension: (OR: 1.95, 95% CI: 0.43 - 8.87, P: 1.95) - Marital Status: Single: (OR: 1.24, 95% CI: 0.46 - 3.40, P: 0.671) Divorced: (OR: 1.56, 95% CI: 0.49 - 5.02, P: 0.453) Widowed: (OR: 1.39, 95% CI: 0.70 - 2.76, P: 0.354) - Education: (OR: 0.64, 95% CI: 0.40 - 1.01, P: 0.053) - Duration of diabetes: (OR: 1.48, 95% CI: 0.86 - 2.54, P: 0.161) |
|
Karymsakov et al., 2024 (30) |
Bivariate analysis |
- Age: 40-49 years: (OR: 0.36, 95% CI: 0.11 - 1.22, P: 0.102) 50-59 years: (OR: 0.41, 95% CI: 0.13 - 1.31, P: 0.134) 60-69 years: (OR: 0.23, 95% CI: 0.08 - 0.71, P: 0.01*) 70-79 years: (OR: 0.19, 95% CI: 0.06 - 0.61, P: 0.006*) - Gender: Female: (OR: 0.98, 95% CI: 0.60 - 1.60, P: 0.93) - Occupation: Unemployed: (OR: 0.78, 95% CI: 0.33 - 1.89, P: 0.59) Fully employed: (OR: 2.11, 95% CI: 1.22 - 3.67, P: 0.01*) Partially employed: (OR: 1.83, 95% CI: 0.55 - 6.10, P: 0.32) - Marital Status: Not married: (OR: 2.07, 95% CI: 0.72 - 5.93, P: 0.83) Widowed: (OR: 0.73, 95% CI: 0.32 - 1.68, P: 0.462) Divorced: (OR: 1.24, 95% CI: 0.17 - 9.01, P: 0.174) - Education: Specialized: (OR: 0.7, 95% CI: 0.25 - 1.94, P: 0.49) Bachelor: (OR: 1.44, 95% CI: 0.65 - 3.20, P: 0.37) Master: (OR: 2.45, 95% CI: 0.83 - 7.20, P: 0.1) School: (OR: 1) |
|
Murwanashyaka et al., 2022 (31) |
Bivariate regression |
- Age: 18–30 years: (OR: 1, 95% CI: Not provided, P: 0.32) 31–50 years: (OR: 2.71, 95% CI: 0.67 - 11.01, P: 0.16) More than 50 years:(OR: 0.9, 95% CI: 0.499 - 1.63, P: 0.73) - Gender: Male: 47 (OR: 1, 95% CI: Not provided, P: 0.032*) Female: (OR: 1.85, 95% CI: 1.05 - 3.24, P: Not provided) - Marital Status: Single: (OR: 1, 95% CI: Not provided, P: 0.26) Married/cohabiting: (OR: 2.02, 95% CI: 0.682 - 6.01, P: 0.204) Divorce: (OR: 0.96, 95% CI: 0.44 - 2.1, P: 0.917) - Duration with diabetes and medications: 1-3 years: (OR: 1, 95% CI: Not provided, P: 0.031*) 4-10 years: (OR: 2.18, 95% CI: 1.09 - 4.34, P: 0.027*) More than 10 years: (OR: 1.03, 95% CI: 0.43 - 2.42, P: 0.954) - Education: No formal education: (OR: 1, 95% CI: Not provided, P: 0.036*) Primary: (OR: 2.87, 95% CI: 1.27 - 6.5, P: 0.012*) Secondary: (OR: 1.834, 95% CI: 0.94 - 3.58, P: 0.075) - Employment status: Jobless: (OR: 1, 95% CI: Not provided, P: 0.008**) Public employee: (OR: 2.36, 95% CI: 1.24 - 4.48, P: 0.009*) Private: (OR: 0.8, 95% CI: 0.38 - 1.72, P: 0.57) |
|
Saraiva et al., 2020 (32) |
Chi square |
- Number of prescribed medicines: p = 0.369 - Antidiabetic therapy: Metformin: p = 0.014* - Non-prescribed drugs: Total: p = 0.083 Over-the-counter drugs: p = 0.090 Prescription drugs: p = 0.432 |
|
Teklay et al., 2013 (33) |
Multivariate regression |
- Depressive symptoms: (aOR: 2.404, 95% CI: 1.323 - 4.366, P: 0.004*) - Side Effects: (aOR: 1.868, 95% CI: 1.012 - 3.446, P: 0.046) - Complexity of Regimen: (aOR: 3.413, 95% CI: 1.652 - 7.05, P: 0.001*) - Diabetes complications: (aOR: 1.569, 95% CI: 0.701 - 3.512, P: 0.273) - Fasting blood glucose level: (aOR: 1.469, 95% CI: 0.732 - 2.949, P: 0.28) - Hospitalization: (aOR: 2.42, 95% CI: 1.174 - 4.992, P: 0.017*) |
Discussion
This systematic review analyzed current literature to identify factors influencing medication adherence among diabetic patients. The cumulative prevalence of medication non-adherence in our study is 47.63%. The studies presented a range of findings, with a consensus that older age consistently acts as a protective factor against non-adherence. Specifically, individuals aged over 60 were consistently found to be less likely to miss their medication regimens. Similarly, findings of a study by Alqarni et al. demonstrated that medication adherence is positively associated with patient age which could be attributable to the fact that elderly people have comorbidities and are expected to have a higher number of medications on their prescription. Experience with drug therapy may lead to improved awareness of adherence. The authors observed that only a third of the study population were adherent (34). On the contrary, a cross-sectional study by Faisal et al. indicated that patients above the age of 60 were six times more likely to not adhere to their anti-diabetic medications. Their non-adherence rate (38.1%) was lower than our reported prevalence (35). A recent meta-analysis noted a lower pooled prevalence of non-adherence (37.3%) among diabetic patients in comparison to our findings (36).
Another cross-sectional analysis from Saudi Arabia described that age, marital status, occupation, comorbidities, diagnosis time, and prior complaints of diabetes mellitus (DM) complications all had significant effects on DM medication compliance (37). Although their prevalence of reported non-adherence was 34.7%, below our observed frequency, we did not find any significant association between medication non-adherence and marital status, although similarly, we noted age to be a significant predictor of non-adherence. However, a systematic review from Asia indicated that the medication adherence rate among individuals with diabetes was low to moderate. Four particular characteristics inconsistent with diabetes medication adherence included older age, gender, diabetes duration, and family history/comorbidities (38). Even in our review, we observed that gender did not consistently predict non-adherence, with only one study showing a significant association with male gender while another study showed overall significant association among those reviewed. Furthermore, compared to our findings, Khan et al. noted that the total prevalence of treatment noncompliance among participants was 67.9% (n = 318; 95% CI 63.59-72.02%). Males (69.34%) were less likely to comply than females (65.45%, P =.003). Urban individuals were substantially more noncompliant than rural participants (71.04 vs. 60.15%, P =.023). There was a statistically significant difference in the prevalence of noncompliance among participants of varying educational levels. On bivariate analysis, the following factors were found to be significantly associated with non-compliance: female gender (OR = 1.90, CI = 1.32-4.57), level of education (illiteracy) (OR = 5.27, CI = 4.63 - 7.19), urban population (OR =5.22, CI = 3.65 - 8.22), irregularity of the follow-up (OR = 8.41, CI = 4.90 - 11.92), non-adherence to drug prescription (OR = 4.55, CI = 3.54 - 5.56), non-adherence to exercise regimen (OR = 5.55, CI = 4.26 - 6.), insulin (OR = 1) (39).
On the contrary, a recent study from the United Arab Emirates reported high adherence rates of 91% and 90% among males and females, respectively. The authors further observed that some of the most common causes of noncompliance with antidiabetic medications were forgetfulness, severe side effects, the use of numerous treatments, and protracted treatment duration (40). Results of another recent study from Saudi Arabia highlighted that overall, 293 (77.1%) participants were adherent, with 87 (22.9%) non-adherents. Several sociodemographic factors, such as marital status, nationality, geographic region, and employment status, were substantially linked with DM treatment adherence (P = 0.001, 0.002, 0.003, and 0.002, respectively) (41). Both of these studies reported non-adherence rates lower than ours; however, in our review, we identified that employment status demonstrated varying associations, with fully employed individuals occasionally exhibiting higher odds of non-adherence compared to other employment statuses. Marital status generally did not significantly predict non-adherence.
Findings from another systematic review of recent times reported that the major determinants of non-adherence to treatment among T2DM patients are unaffordable care, patients' lack of knowledge about the disease process, a lack of family support in daily self-care management, polypharmacy drug prescriptions, and unsatisfactory health messages from health providers (42). Contrarily we did not observe any of these factors in our findings which may be explained due to the difference in intrinsic characteristics of studies. Results of a mixed-method study showed that the rate of non-adherence to medication was almost 46.6%. The reasons for medication non-adherence were classified into five categories: perceived benefit of complementary and alternative medicine, attitude toward drawbacks of western medication, poor healthcare provider-patient relationship, undesirable emotional response to medication intake, and restraints in daily routine or cognitive function (43). Although their reported prevalence of non-adherence is closer to our observed frequency in this study their reported factors are heterogenous of our findings.
One of the included studies in our review showed a significant association between depressive symptoms and non-adherence (33). Similarly, an Iranian study by Roohafza et al. showed that stress levels, regardless of age, gender, or education level, had an independent effect on compliance, particularly medication adherence in both hypertensive and diabetic patients (44). Additionally, evidence from research suggests that medication nonadherence may be associated with emotional distress and poor diabetes treatment outcomes (45).
Moreover, results from a qualitative content analysis by Pourhabibi et al. demonstrated several reasons for treatment nonadherence among diabetic patients with low health literacy. Therefore, this domain should be considered while developing promotional, educational, and supportive interventions. Given the importance of treatment adherence for patients, it appears vital to create empowered family-based treatments that focus on improving health literacy (46). In this review, we noted that education level showed mixed results, with higher education potentially linked to lower non-adherence rates in certain analyses. Similarly, Shaikh et al. depicted in their study findings that participants who had completed secondary school were more likely to adhere to their antidiabetic drugs (96.26%). Adherence rates among patients with bachelor's and master's degrees were 87.80% and 88.88%, respectively. Illiterate participants reported an adherence rate of 78.94%; however, the results were not statistically significant (40).
Medication adherence in chronic conditions is quite low because patients discontinue their prescriptions abruptly and drastically after the first six months of treatment. Addressing drug noncompliance is a top policy and research priority for governments, private foundations, and patient organizations. Adherence to medication by patients is linked to a lower risk of diabetes complications. However, non-compliance is a chronic concern in the execution of diabetes care. Assessing the magnitude of medication non-adherence and investigating the multi-level factors associated with medication non-adherence using various approaches constitute two areas of concern that must be addressed in order to improve medication adherence. Understanding the factors that lead to poor medication adherence is critical for developing targeted and effective interventions to improve medication adherence among diabetes patients (47).
Furthermore, Zairina et al. narrated that nonadherence to therapy could be caused by one or more of the following: the intricacy of the therapeutic regimen, contempt for the physician's instructions, or a lack of self-management skills. Nonadherence to drug regimens is a major concern for healthcare providers around the world considering the implications. Patient adherence to antidiabetic drugs is important in preventing serious medical repercussions and lowering healthcare expenditures. However, poor antidiabetic medication adherence was mostly caused by patient-healthcare provider relationships. Furthermore, culturally and gender-sensitive communication approaches for tailoring healthcare goals to patients' needs may make healthcare professionals' jobs easier (48). Additionally, Polonsky et al. described that patients are more inclined to adhere to pharmaceutical regimens when they have a clear impression that the drug is helping them achieve positive and relatively immediate results. Indeed, several research spanning a wide range of chronic medical conditions have consistently found that drug adherence correlates with perceived need. Patients are more likely to adhere to recommended medication if they believe it is truly necessary. Evidence suggests that modifiable factors influencing T2D medication adherence can be divided into two categories: treatment burden, including complexity convenience, out-of-pocket costs, and hypoglycemia risk and treatment-related beliefs (22).
This review possesses several strengths that enhance its credibility and utility. Firstly, the review employed a comprehensive search strategy, systematically scouring multiple databases and potentially including grey literature sources and expert consultations to ensure thorough coverage of relevant studies. By encompassing a diverse range of studies published over various years, the review can offer a broad perspective on non-adherence rates and factors influencing medication compliance across different populations and healthcare settings. Methodological rigor, including rigorous quality assessment of included studies and standardized data extraction methods, enhances the reliability of synthesized findings. The review's exploration of various factors contributing to non-adherence, such as demographic characteristics, treatment complexities, psychosocial influences, provides a nuanced understanding of this complex issue. Ultimately, these strengths enable the review to not only identify trends and gaps in current research but also to offer practical implications for clinical practice and policy development aimed at improving adherence and health outcomes among individuals with T2DM.
Limitations and future research directions
This review has limitations that should be considered when interpreting its findings. Specifically, the inclusion of the study by Hamalaw et al. (28) may restrict the generalizability of the results, as it was rated as low-quality according to the NOS tool. However, it was included based on consensus between two reviewers to ensure comprehensive coverage of potential information and to mitigate the risk of publication bias. Secondly, the review includes studies that vary widely in terms of methodologies, populations studied, definitions of adherence, and measurement tools, which can complicate the synthesis of results and limit the generalizability of findings across diverse settings and patient groups. Furthermore, limitations related to language bias may restrict the diversity of findings considered, potentially excluding relevant studies conducted in different regions or languages. Variability in how adherence is measured, for instance, self-report vs. objective measures like pharmacy refill records across studies, can impact comparability and the accuracy of reported adherence rates. To mitigate these limitations, future systematic reviews should strive for comprehensive inclusion criteria, rigorous assessment of study quality, and transparent reporting practices to enhance the validity and applicability of their findings regarding non-adherence to medication in T2DM. Additionally, future research on non-adherence to medication among individuals with T2DM should delve into several critical areas. Longitudinal studies are essential to track adherence patterns over time, offering insights into the dynamic nature of adherence behaviors and their impact on health outcomes. Innovative intervention strategies tailored to address specific barriers, such as medication complexity and patient beliefs, should be developed and rigorously evaluated for their effectiveness. The integration of digital health technologies, including mobile apps and wearable devices, holds promise for improving adherence through real-time monitoring, personalized reminders, and educational support. Personalized medicine approaches, leveraging genetic, physiological, and behavioral predictors of non-adherence, can inform targeted interventions and enhance treatment outcomes. Health system-level interventions, including policy changes and integrated care models, need thorough investigation to optimize healthcare delivery and support diabetes management. Understanding the influence of psychosocial factors and cultural contexts on adherence, along with conducting cost-effectiveness analyses and prioritizing patient-centered outcomes, will further refine strategies to enhance medication adherence and mitigate the complications associated with T2DM.
Conclusion
This systematic review underscores the complex landscape of medication non-adherence among individuals with T2DM. The studies reviewed revealed wide-ranging rates of non-adherence, illustrating a significant challenge in managing this chronic condition effectively. Age emerged as a consistent protective factor, with older individuals demonstrating greater adherence to prescribed regimens. Gender and education level showed mixed associations, suggesting nuanced relationships that warrant further investigation. These findings underscore the need for personalized approaches in diabetes management, addressing not only clinical factors but also socio-demographic and psychological influences to improve medication adherence and ultimately health outcomes for patients. Future research should focus on comprehensive strategies that integrate these diverse factors to optimize treatment adherence in individuals with T2D.
Disclosure
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Ethical consideration
Non-applicable
Data availability
All data is provided within the manuscript.
Author contribution
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.