Volume 4, Issue 8
August 2024
The Significance of Nitroglycerin in Emergency Medicine Across Multidisciplinary Conditions: A Comprehensive Systematic Review
Ahmed Abdulrahman Aldahash, Abdulaziz Saud AlGhazwani
DOI: http://dx.doi.org/10.52533/JOHS.2024.40804
Keywords: nitroglycerine, emergency, management, heart failure, pulmonary edema
Background: Nitroglycerin, a fast-acting vasodilator, is often used in the emergency department as a first-line treatment for angina and chest pain caused by acute coronary syndrome. It can also be used to treat other conditions such as acute heart failure, pulmonary edema, and aortic dissection. In patients with decompensated congestive heart failure with acute pulmonary edema, intravenous bolus nitroglycerin can reduce the requirement for intubation, intensive care admission rate and hospital duration of stay. Through this systematic review, we aim to elaborately analyse the existing literature to define the beneficial role of the administration of nitroglycerine across diverse cohorts of patients reporting to emergency medicine settings.
Methods: Our study aimed to assess the significance of nitroglycerine in emergency medicine settings for various multidisciplinary conditions. As a result, we included original studies that defined the role and utilization of nitroglycerine across various diseases among emergency medicine patients specifically. Studies including the pediatric population were excluded. Newcastle-Ottoman Castle and Cochrane risk of bias assessment tools were utilized to assess the quality of included studies.
Results: Final inclusion incorporated a total of 6 studies encompassing 9452 patients, published between 2006 and 2022. The findings highlight the beneficial role of nitroglycerine in the management of various conditions. The majority of the patients presented with heart failure followed by cases of hypertension, pulmonary oedema, circulatory shock, stroke, acute coronary syndrome or myocardial infarction, and chest pain. The utilization of nitroglycerine resulted in significant symptomatic relief and improvement in the patient's condition.
Conclusion: This review extensively explores the role and utilization of nitroglycerine for the management of diverse conditions treated in emergency settings. Nitroglycerine offers a wide range of clinical applications in the emergency department and is reinforced by established guidelines for angina, heart failure, acute coronary syndrome, pulmonary edema and other conditions. Other uses for nitroglycerine exist; however, most indications suffer from a lack of stringent, randomized trial evidence, emphasizing the need for more research into this time-tested medicine.
Introduction
Global awareness of the need for emergency care and the specialization of emergency medicine are both continuously expanding. In the era of 1960s and 1970s, emergency medicine became a distinct specialty as a result of the growing demand for rapid, high-quality emergency care for patients who were admitted to hospitals with acute medical issues. It has been demonstrated that emergency medicine enhances care and outcomes for patients with emergency concerns (1). Emergency medicine is a branch of medicine that focuses on diagnosing and treating unexpected injuries or diseases. Emergency medicine encompasses the initial assessment, diagnosis, treatment, multi-provider coordination of care, and discharge of patients in need of immediate medical, surgical, or mental health attention. The practice of emergency medicine is not spatially restricted; it can take place in both hospital-based and out-of-hospital emergency departments, urgent care facilities, observation medicine units, emergency medical response vehicles, disaster sites, and via telemedicine. Planning, supervision, and medical guidance for community emergency medical response, medical control, and catastrophe preparedness are all included in emergency medicine. Emergency departments and other parts of the healthcare delivery system benefit greatly from the clinical, administrative, and leadership services that emergency medicine specialists offer (2).
Diverse multidisciplinary conditions are managed in emergency medicine settings. In the chain of survival for acute diseases including myocardial infarction, stroke, and trauma, the emergency care system is vital. Depending on the age group, the most frequent reasons for emergency visits include heart failure, pneumonia, sepsis, trauma, asthma, and chronic obstructive pulmonary disease. Although its characteristics remain timely in-hospital diagnosis and treatment, emergency care has evolved over the last 20 years to include a wider range of treatments. These encompass both pre- and post-emergency department activities such as urgent care routes for lower-acuity patients and transfers of patients to higher-acuity inpatient settings or return to their usual source of care and post-emergency department activities (3). The prompt medical attention provided to the populace in situations of emergency poses a significant challenge to the healthcare system and is becoming more and more necessary. As a result of this advancement, clinical acute and emergency medicine has advanced significantly and is currently undergoing additional professionalism. Providing emergency patients with the best care possible must be the primary goal (4).
Vasodilators are valuable in the management of acute heart failure, a condition frequently encountered in emergency medicine settings, especially when increasing afterload is the underlying cause of decompensation. The time-honored strategy of afterload reduction has primarily depended on the use of intravenous nitrovasodilators, which, when appropriately dosed, may provide significant symptom alleviation for patients with acute hypertensive heart failure (5). Moreover, a hypertensive emergency is a significant clinical phenomenon that can cause damage to the cardiovascular, neurological, and renal systems, among other organs. It may lead to potentially fatal repercussions if it is not identified and addressed promptly. Vasodilators are the cornerstone of care for hypertensive crises. Vasodilators are classified into many classes according to their site and mode of action. The most often used vasodilators are peripheral dopamine agonists, calcium channel blockers, beta, alpha, and beta blockers, as well as directly acting medications that work through the vascular nitric oxide route. By lowering peripheral resistance, the diverse types of vasodilators lower blood pressure through distinct neurohormonal signaling pathways (6).
Nitrovasodilators such as nitroglycerin, isosorbide mononitrate, isosorbide dinitrate, and sodium nitroprusside have long been regarded as first-line treatments for acute hypertensive heart failure. These drugs function by delivering an exogenous source of nitric oxide, which subsequently binds to soluble guanylate cyclase, resulting in cyclic GMP and vascular smooth muscle relaxation (5). The hemodynamic effects of vasodilators differ considerably across drugs. Some vasodilators, such as nitrates, function predominantly on the venous side of the circulatory system, redirecting circulating blood volume away from the heart and into the venous capacitance system. As a result, both ventricular preload and venous return to the heart diminish. Intravenous nitrates significantly increase nitric oxide-induced vasodilation and have an effect within 2-3 minutes. The immediate effects include venous dilation, blood volume redistribution, reduced venous return, less congestion, and symptom relief. Higher nitrate doses, in addition to sodium nitroprusside, dilate the arteries, lowering blood pressure and left ventricular afterload. Nitrates reduce afterload, myocardial oxygen consumption, and intra-ventricular pressures. Because of their modes of action, intravenous vasodilators are thought to be beneficial in patients with acute heart failure and acute pulmonary edema, where raised cardiac and systemic blood pressures are dramatically elevated in the absence of or with low systemic fluid accumulation (7).
Nitroglycerin, a fast-acting vasodilator, is often used in the emergency department as a first-line treatment for angina and chest pain caused by acute coronary syndrome. It can also be used to treat other conditions, such as acute heart failure, pulmonary edoema, and aortic dissection. In the body, nitroglycerin is converted to nitric oxide, a strong vasodilator, resulting in vasodilation at lower dosages and arteriodilation at higher dosages, which reduces preload and afterload, respectively. Although nitroglycerin has traditionally been delivered as a sublingual pill and/or spray, it is frequently administered intravenously in emergency departments since it allows for titration with predictable pharmacokinetics (8). In patients with decompensated congestive heart failure with acute pulmonary edema, intravenous bolus nitroglycerin can reduce the requirement for intubation, ICU admission rate, and hospital duration of stay, in line with evidence from recent emergency department findings. While sublingual nitroglycerin effectively treats decompensated congestive heart failure patients with acute pulmonary edema in the prehospital situation (9).
Sublingual, topical, or intravenous nitroglycerin infusion is indicated as a first-line blood pressure management treatment in acute hypertension, pulmonary edema and acute coronary syndrome due to its beneficial effect on lowering preload and cardiac output. It is advantageous as a second-line therapy in hypertensive situations owing to acute sympathetic crises such as cocaine, amphetamines, monoamine oxidase inhibitor toxicities, and Irukandji Syndrome. Sublingual nitroglycerin is extensively utilized due to its antianginal effects. However, its convenience, ease of administration, and early onset of action make it a suitable drug for rapid blood pressure management in emergency medicine settings until definitive therapy is initiated (10). Since various multidisciplinary conditions are encountered in emergency medicine settings, the role of nitroglycerine in each remains underdefined in the literature. Through this systematic review, we aim to elaborately analyze the existing literature to define the beneficial role of the administration of nitroglycerine across diverse cohorts of patients reporting to emergency medicine settings. The findings will provide deep insights into the efficacious role of nitroglycerine for various diseases witnessed in the emergency department, and they can additionally help guide clinical practice to achieve optimal outcomes and increase patient satisfaction
Methods
Definition of Outcomes and Inclusion Criteria
Our study aimed to assess the significance of nitroglycerine in emergency medicine settings for various multidisciplinary conditions. As a result, we included original studies that defined the role and utilization of nitroglycerine across various diseases among emergency medicine patients specifically. Within the context of this review of multidisciplinary conditions, we considered the patient population suffering from diverse diseases necessitating emergency treatment including heart failure and other cardiovascular diseases, stroke, and pulmonary edema among others. Studies including the pediatric population were excluded. Moreover, this review excluded case reports featuring small sample sizes and lacking descriptive statistics. Nonhuman or laboratory studies, non-original or incomplete investigations, abstract-only articles, protocols, theses and articles not published in English or lacking English information were also excluded based on predetermined criteria.
Search Strategy
After achieving our desired outcomes, we conducted a brief manual screening of potential studies to extract relevant keywords for crafting an optimal search query. Our search strategy encompassed terms such as (significance OR importance OR utilization OR role) AND (nitrates OR nitroglycerine OR nitro-glycerine) AND (emergency OR ‘emergency department’ OR ‘emergency medicine’) AND (management OR treatment) AND (‘diverse diseases’ OR ‘multidisciplinary conditions’ OR ‘critical diseases’). We utilized PubMed, Science Direct, Web of Science, and the Cochrane Library as our databases for the search. To ensure inclusivity of pertinent research, we limited our search to the titles and abstracts of retrieved results. Subsequently, we employed EndNote software to compile and eliminate duplicates across all databases. Additionally, we manually scrutinized the reference lists of included studies, related reviews, and relevant sections of comparable articles in PubMed to identify any potentially overlooked papers. Throughout this systematic review, we adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Screening and Extraction
Articles with irrelevant titles were excluded from consideration. In the subsequent phase, both the full text and abstracts of the papers were meticulously reviewed to determine their compliance with the inclusion criteria. To streamline the process, titles and abstracts were organized, assessed, and scrutinized for any duplicate entries using reference management software (Endnote X8). To ensure the highest quality of selection, a dual screening approach was adopted, involving one screening for the evaluation of titles and abstracts, and another for the comprehensive examination of the entire texts. Once all relevant articles were identified, a structured extraction sheet was created to capture pertinent information aligned with our specific objectives. This included delineating the desired outcomes and baseline characteristics such as study design and period, age, gender, disease or condition and the geographical location of the study, among certain others.
Quality Assessment
We collected data from the encompassed studies to evaluate the potential bias they might entail. For assessing the quality of observational studies, we employed the modified Newcastle-Ottawa Scale (11), encompassing four domains: methodological quality, comparability, outcome/exposure assessment, and outcome/exposure reporting. Each study was rated on a scale from 0 to 10 according to the extent of bias, categorized as excellent, good, satisfactory, or unsatisfactory. For the assessment of the quality of a randomized trial, the Cochrane risk of bias tool was utilized (12). This tool assesses the quality of the study by assessing risk in seven domains, including random sequence generation, allocation concealment, blinding of participants and outcomes, incomplete outcome data, selective reporting, other biases, and the overall risk of bias.
Results
Search Results
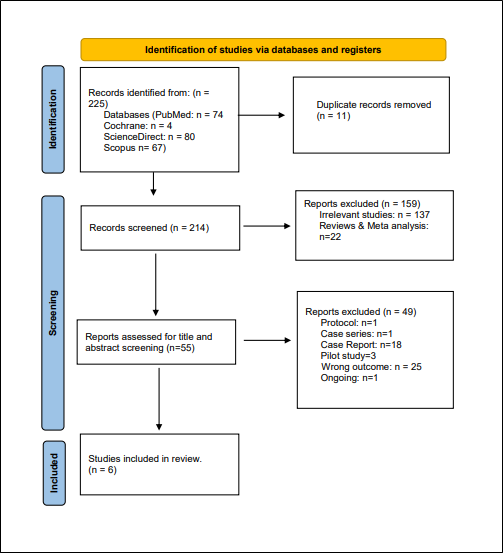
We executed the search methodologies outlined previously, resulting in the identification of a total of 225 citations, subsequently reduced to 214 following the removal of duplicates. Upon screening titles and abstracts, only 55 citations met the eligibility criteria for further consideration. Through full-text screening, this number was further refined to 6 articles aligning with our inclusion and exclusion criteria. Figure 1 provides an in-depth depiction of the search strategy and screening process.
Results of Quality Assessment
Upon evaluating the quality of the studies included, it was determined that overall, the studies exhibited good quality with minimal risk of bias, except for one study, which showed unsatisfactory quality. The detailed findings of the quality assessment are presented in Tables 1 and 2.
|
Table 1: Newcastle-Ottawa Scale of each included non-randomized studies. |
|||||
|
Study |
Selection |
Comparability |
Outcome |
Total score |
Quality |
|
Greenwood JC, et al. (2022) (13) |
4 |
0 |
2 |
6 |
Good |
|
Bosson N, et al. (2019) (14) |
4 |
2 |
1 |
7 |
Good |
|
Aziz EF, et al. (2011) (15) |
4 |
1 |
2 |
7 |
Good |
|
Vuylsteke A, et al. (2011) (16) |
3 |
0 |
1 |
4 |
Unsatisfactory |
|
Steele R, et al. (2006) (17) |
4 |
0 |
2 |
6 |
Good |
|
Table 2: Cochrane risk of bias for randomized controlled study. |
||||||||
|
Studies |
Random sequence generation |
Allocation concealment |
Blinding of participants and personnel |
Blinding of outcome assessment |
Incomplete outcome data |
Selective reporting |
Other bias |
Overall |
|
Cerbin LP, et al. (2018) (18) |
Moderate |
Unclear |
Low |
Low |
Low |
Low |
Low |
Low |
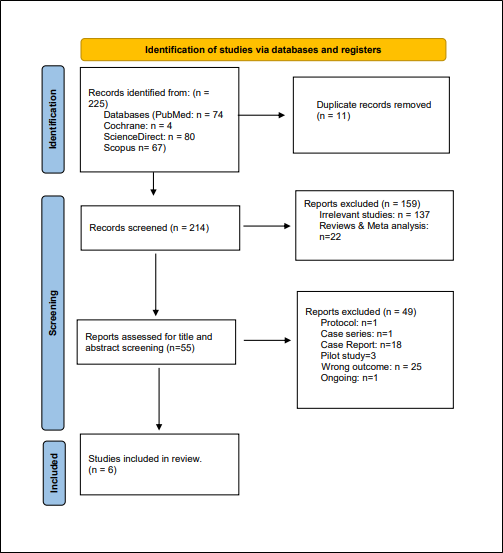
Figure 1: PRISMA Flow diagram
Characteristics of the included studies
We incorporated a total of 6 studies encompassing 9452 patients, published between 2006 and 2022 (13-18). All participants in these studies were aged above 60 years of age, with 57.29% being male and 42.70% female. Notably, all the studies were observational with a single post-hoc analysis, multicentre study. Geographically, all the studies were from United States except one study which was from Europe. A comprehensive summary of the baseline characteristics of these studies can be found in Table 3. Discrepancies in sample sizes across the included papers likely stem from differences in study objectives and inclusion criteria.
Study outcome measures
The use of nitroglycerine across various multidisciplinary conditions encountered in the emergency medicine setting was assessed. The majority of the patients presented with heart failure, followed by cases of hypertension, pulmonary oedema, circulatory shock, stroke, acute coronary syndrome or myocardial infarction, and chest pain. Almost three studies reported that significant symptomatic relief was observed post nitroglycerine administration (14, 17, 18), while another two of the included studies demonstrated that improvement in symptoms were also noted (13, 15). Regarding the utilization of nitroglycerin in the emergency medicine setting, a study by Bosson et al. noted that almost 44% of the patients received nitroglycerin, while Cerbin et al. observed that intravenous nitroglycerin administration was higher for patients presenting in off-hours (18% vs. 11%) (14, 18). Moreover, a study by Steele et al. indicated that 66% of the participants responded well to nitroglycerine, whereas 34% did not (17). Primarily, two of the included studies assessed the adverse events among which one study did not find any difference between patients receiving nitroglycerine and those not receiving this vasodilator (14). However, another study by Vuylsteke et al. observed hypotension within 72 hours of initiation of treatment (16) (Table 4). Overall, the findings demonstrate the efficacious role of nitroglycerine in the management of various multidisciplinary conditions encountered in emergency medicine settings; however, the generalizability of these findings is constrained due to the limited evidence available in this regard, which highlights the need for further clinical research.
|
Table 3: Baseline characteristics included studies. |
|||||||||
|
Studies |
Publisher journal |
Year of publication |
Country of the patients |
Study design |
Study period |
Total Number of participants |
Treatment group/control group |
Age |
Gender of total participants Male %/Female% |
|
Greenwood JC, et al. (13) |
Sci Rep. |
2022 |
USA |
observational |
2021 |
40 |
20/20 |
64 ± 9/ 67 ± 11 |
75%/25% |
|
Bosson N, et al. (14) |
Prehospital Emerg Care. |
2019 |
USA |
prospective |
2015-2016 |
780 |
340/440 |
median= 63 years |
61%/39%% |
|
Cerbin LP, et al. (18) |
JACC Heart Fail |
2018 |
US |
Post hoc analysis, multicenter |
NR |
7141 |
Regular Hours :3843/off-Hours:3298 |
median=67 years |
65.78%/34.22% |
|
Aziz EF, et al. (15) |
Hospital practice (1995) |
2011 |
USA |
retrospective study |
NR |
430 |
diuretics and NTG: 46 |
72 ± 13 |
43%/57% |
|
Vuylsteke A, et al. (16) |
Crit Care |
2011 |
European countries, multicenter |
observational study |
2009 |
791 |
ED/Perioperative: |
median =70 years |
48%/52% |
|
Steele R, et al. (17) |
Canadian Journal of Emergency Medicine |
2006 |
USA |
Prospective observational cohort |
NR |
270 |
177/93 |
64 years |
51%/49% |
NR: Not reported
|
Table 4: outcome measures of included studies |
||||||
|
Study |
Treatment usage/response rate |
Disease/condition |
Symptom relief |
BP reduction |
Improvement |
Adverse events |
|
Greenwood JC, et al. (13) |
NR |
circulatory shock, microcirculatory blood flow and cardiovascular disease |
NR |
NR |
Increase in MFI (2.57 vs. 2.97, p < 0.001), Increase in TVD (22.47 vs. 27.51 mm/mm2, p < 0.009), Increase in PPV (90.76 vs. 95.91%, p < 0.001), Increase in PVD (20.44 vs. 26.41 mm/mm2, p < 0.001), Increase in RBC velocity (402.2 vs. 693.9 µm/s, p < 0.0004), Decrease in MHI (0.33 vs. 0.04, p < 0.001). |
NR |
|
Bosson N, et al. (14) |
NTG Administration by EMS to 44% of patients. |
STEMI (80% NTG received) |
In patients with an initial pain score >0, those who received NTG experienced an average reduction in pain score of -2.6 (95% CI): -3.0 to -2.2). |
Patients treated with NTG had a median change in SBP of -10 mmHg. The median difference in SBP reduction: -6 mmHg between the groups. |
NR |
There were no significant differences between the NTG and non-NTG groups in terms of frequencies of ED hypotension, bradycardia, drop in SBP ≥30mmHg, OHCA. |
|
Cerbin LP, et al. (18) |
Off-hours patients were more likely to receive IV nitroglycerin (18% vs. 11%) |
AHF |
Dyspnea Relief at 24 Hours: OR (95% CI): 1.14(1.04–1.24), p = 0.01 |
NR |
NR |
NR |
|
Aziz EF, et al. (15) |
NR |
ADHF |
NR |
NR |
a significant reduction in discharge BNP levels: 295 ± 298 pg/mL |
NR |
|
Vuylsteke A, et al. (16) |
NR |
hypertension, heart failure or pulmonary oedema, stroke, acute coronary syndrome or myocardial infarction, and chest pain |
NR |
NR |
NR |
hypotension within 72 hours of the start of treatment (4.4% of ED patients) |
|
Steele R, et al. (17) |
66% showed a positive response to NTG vs. 34% showed a negative response. |
AMI (13%) |
66% chest pain relieve in enrolled patients. |
NR |
NR |
NR |
NR: Not reported, NTG: Nitroglycerin, ED: Emergency department, SBP: systolic blood pressure, OHCA: out of hospital cardiac arrest, PD: Pharmacodynamic, MFI: microvascular flow index, TVD: total vessel density, PPV: proportion of perfused vessels, PVD: perfused vessel density, RBC: red blood cell, MHI: microcirculation heterogeneity index, OR (95% CI): Odds ratio (95% confidence interval).AMI: Acute myocardial infraction, STEMI: ST-segment Elevation Myocardial Infarction, ,ADHF: Acute Decompensated Heart Failure, EMS: emergency medical service.
Discussion
This review extensively explores the role and utilization of nitroglycerine for the management of diverse conditions treated in emergency settings. The findings highlight the beneficial role of nitroglycerine in the management of various conditions, primarily heart failure, cardiovascular diseases, pulmonary edema, and stroke. The utilization of nitroglycerine resulted in significant symptomatic relief and improvement in the patient's condition. The role of nitroglycerin is further comprehensively discussed below in these domains.
Clinical practice and implications
The majority of the patients in our study reported heart failure, acute coronary syndrome, circulatory shock, chest pain, and myocardial infarction. Administration of nitroglycerine resulted in efficacious management of the conditions. Similarly, results of a retrospective study by Wilson et al. demonstrated that in emergency department patients with acute heart failure, intermittent intravenous nitroglycerin bolus was linked with a lower ICU admission rate and a shorter hospital duration of stay than continuous infusion (19). Additionally, Miro et al. described that early prehospital intravenous nitroglycerine administration was linked to lower mortality and post-discharge events, whereas intravenous nitroglycerine initiated in the emergency room only improved post-discharge event rates (20). However, on the contrary, another study by Miro et al., almost a year later than the previous, indicated that intravenous nitroglycerine may be risky in patients with just minor clinical congestion. The phenotypic classification of acute heart failure based on congestion/hypoperfusion upon emergency room presentation does not identify subgroups of individuals in whom intravenous nitroglycerin might reduce mortality. However, it may be useful in patients with a left ventricular ejection fraction of less than 50% (21). This hypothesis will need to be proven in the future with evidence-based research.
Koroki et al., however, stated that nitroglycerin, in particular, has a strong effect on the coronary arteries, making it the ideal treatment for acute heart failure syndrome linked with myocardial ischemia. Consequently, nitroglycerin is suggested as the first-line treatment for acute heart failure syndrome in patients with coexisting hypertension, according to several guidelines (22). Furthermore, Boden et al. narrated that short-acting nitroglycerin, administered as a sublingual tablet or spray, can supplement anti-anginal therapy as part of optimal medical therapy in patients with refractory and recurrent angina, either with or without myocardial revascularization. It is most commonly used to provide rapid therapeutic relief for acute recurrent angina attacks (23). Moreover, similar to our results, Wang and Samai commented that high-dose nitrates are likely safe and may be helpful, as evidenced by several research studies. Acute heart failure patients with significant respiratory distress, systolic blood pressure ≥160 mmHg, or mean arterial pressure ≥120 mmHg may benefit from high-dose nitroglycerin (24). Likewise, findings of a study by Todoroski depicted that providing nitroglycerin 10 minutes after aspirin lowered subjective pain scores as well as the requirement for further nitroglycerin or opioids in patients with acute coronary syndromes (25). The findings of our study also indicated symptomatic relief and improvement post-nitroglycerine administration.
Similarly, results of a randomized trial from recent times showed that at 6 hours, 17 patients (65.4%) in the high-dose group experienced symptom relief, compared to only 3 (11.5%) in the low-dose group (p<0.001). After 12 hours, 88.5% of patients in the high-dose group experienced clinical resolution, compared to 19.5% in the low-dose arm. The low-dose group had a longer median hospital stay (12 hours vs 72 hours), a greater incidence of MACE (3.8% vs 26.9%, p=0.02), and a higher intubation rate (3.8% vs 19.2%, p=0.08). The only short-term side effect reported was a headache in both groups. Patients with sympathetic crashing acute pulmonary edema who received high-dose nitroglycerine (>100 mcg/min) experienced faster symptom resolution than those who received traditional low dosage nitroglycerine, with no noticeable side effects (26). Similarly, our results also suggest that nitroglycerine is safe and effective, as only one study reported hypotension as a side effect in our review studies. Results of another review also concluded that nitrates may be associated with a lower risk of side effects after three hours than placebo (27). Additionally, recent evidence demonstrates that high-dose nitroglycerin is safe and effective for treating hypertensive pulmonary edema in the emergency room (28).
Nitroglycerin is often used to treat pulmonary edema in acute heart failure cases. Although low infusion rates are frequently used, higher infusion rates have better pharmacodynamic characteristics and may enhance the efficacy of the treatment of acute pulmonary edema. Higher initial nitroglycerine dosages may be an effective strategy to reduce time to achieve blood pressure targets, and they should be the focus of future studies (29). Similarly to our findings, the administration of nitroglycerine resulted in effective management. Additionally, Patrick et al. narrated that intravenous nitrates are the principal treatment for hypertensive congestive heart failure with acute pulmonary edema in the hospital setting. Historically, emergency medical care and pharmaceutical therapy for these individuals have relied heavily on sublingual nitrates. Moreover, the findings of their study further indicated that prehospital bolus-dose intravenous nitroglycerin is safe for decompensated congestive heart failure with acute pulmonary edema, and blood pressure, heart rate, and oxygen saturation levels were also improved (28).
Adding more to this context, Ulloa and Tanzi commented that nebulized nitroglycerin is primarily retained in the pulmonary vasculature and has potent local pulmonary effects without systemic adverse effects such as hypotension. As a result, nitroglycerin is virtually liquid NO and produces the same action when nebulized and breathed. Nebulized nitroglycerin can help with a range of patient conditions, including crashing pulmonary embolism, acutely decompensating pulmonary hypertension, and deep refractory hypoxemia. These individuals have a similar pathogenesis, which can be simplified as RV failure caused by increasing afterload in the pulmonary vasculature. Pulmonary vasodilation reduces RV afterload while improving RV function. Furthermore, inhaled pulmonary vasodilators tend to be delivered to the well-ventilated alveoli, guiding blood preferentially towards better ventilated locations and enhancing ventilation perfusion mismatch (30). All these findings suggest and highlight the beneficial role of nitroglycerine in emergency conditions and settings.
Mechanistic insights
Nitroglycerin has become the most frequently prescribed medication for unstable angina pectoris, myocardial infarction, and heart failure since its discovery over 150 years ago. During the rise of the nitroglycerin industry in the twentieth century, the potential of nitroglycerin to increase vasodilation and tolerance was well demonstrated. Nitroglycerin's favourable benefits stem from its ability to stimulate vasodilation, which results in increased blood flow to the heart. Nitroglycerin effects are additionally observed in systemic veins, where the venodilator effect reduces ventricular preload and myocardial wall stress. Nitroglycerin is particularly effective at restoring the oxygen and nutrient supply-demand balance in the ischemic heart (31). Nitroglycerin's application in the treatment of angina pectoris began shortly after its synthesis in 1847. Since then, the discovery of nitric oxide as a biological effector, as well as a better understanding of its roles in vasodilation, cell permeability, platelet function, inflammation, and other vascular processes, have advanced the understanding of organic nitrate therapy's hemodynamic mostly mediated through vasodilation of capacitance and conductance arteries and non-hemodynamic effects, via both nitric oxide-dependent and independent mechanisms. Nitrates are rapidly absorbed from mucous membranes, the gastrointestinal tract, and the skin, so nitroglycerin is available in a variety of preparations for administration via various routes: oral tablets, sublingual tablets, buccal tablets, sublingual spray, transdermal ointment, and transdermal patch; it is also available in intravenous formulations (32).
Organic nitrates are extensively employed in the treatment of cardiovascular disease; however, clinical studies limit their usage to angina. They are also used to treat specific cohorts with heart failure and pulmonary hypertension. The development of tolerance is a serious issue while using nitrates. Although numerous medications have been investigated for use in the prevention of nitrate tolerance, none are currently indicated due to a lack of supporting clinical evidence. Only one approach to preventing nitrate tolerance is universally accepted: utilize a dosing strategy that offers an interval of no or low nitrate exposure during every 24 hours. Nitrates critical function in various cardiovascular disease pathways continues to push research into new approaches to influence both endogenous and external sources of this vital molecular mediator (32).
Limitations and future research directions
Our study provides an in-depth analysis of the current literature, especially emphasizing the role and utilization of nitroglycerine in emergency medicine settings, and is in accordance with the literature, which defines the advantages and strengths of our study. Moreover, the systematic search methodology and the analysis of all keywords in this field further add to the strengths of this study; however, this study also has certain limitations. The limited evidence available and the inclusion of fewer studies limit the generalizability of our findings, which is due to the scarce literature in this regard. Additionally, the inclusion of an unsatisfactory quality study, although single, further restricts our results. Moreover, efficacious comparisons between various doses, strengths, and formulations of nitroglycerine could not be performed as they were beyond the scope of this review. The limited literature available necessitates the need for future research, primarily including randomized trials and population-based studies with sufficient follow-up duration to provide more evidence-based results. Furthermore, the assessment of the efficacy of various strengths and formulations of nitroglycerine across various multidisciplinary conditions will also be addressed by clinical research in the future, which can aid in the development of more standardized protocols to achieve optimal outcomes and effective management of patients.
Conclusion
Nitroglycerine offers a wide range of clinical applications in the emergency department and is reinforced by established guidelines for angina and acute coronary syndrome. There is also accumulating evidence to support the use of intravenous nitroglycerine for acute hypertensive heart failure, either through continuous infusion or recurrent bolus delivery. Other uses for nitroglycerine exist; however, most indications suffer from a lack of stringent, randomized trial evidence, emphasizing the need for more research into this time-tested medicine.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable
Consent for publications
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not Applicable