Volume 3, Issue 11
November 2023
Surgical and Non-Surgical Root Canal Treatment in Diabetic Patients
Ainaa Alsharif, Talal Alkahlan, Yousif Abduldaiem, Areej Sunbul, Naif Alzahrani, Saif Alzahrani, Jana Asubail, Hussain Munthiri, Abdulelah Alharbi, Ahmad Baz, Asem Babaier
DOI: http://dx.doi.org/10.52533/JOHS.2023.31104
Keywords: Diabetes, oral health, root canal treatment, endodontic outcomes, surgical root canal
Oral diseases encompass various conditions affecting teeth, gums, and oral structures and, although preventable, their increasing prevalence and associated issues like pain and aesthetics are concerning. Root canal treatment is a type of treatment that becomes necessary when dental caries reach the dental pulp, causing inflammation and severe pain and impacting oral function. Systemic health conditions are known to influence treatment efficacy, with diabetes being a significant comorbidity affecting oral health. Diabetic individuals must prioritize oral hygiene and regular dental care due to delayed healing and infection complications. Investigating surgical and non-surgical root canal outcomes in diabetic patients is vital, considering the interplay between diabetes and endodontic results. This study, initiated on October 3rd, 2023, conducted a comprehensive literature review using databases like PubMed, Web of Science, and Cochrane. The study discussed that root canal treatment involves two primary types: non-surgical RCT and surgical RCT. The choice depends on the case, with non-surgical being the initial preference. Surgical RCT is considered when non-surgical options fail or in cases of persistent apical periodontitis. In diabetic patients, complexity arises due to an elevated risk of complications, primarily delayed wound healing, necessitating a comprehensive approach. This involves meticulous blood sugar control, judicious antibiotic use, post-operative care, and collaboration with healthcare providers to enhance overall health and well-being.
Introduction
Dental diseases, also known as oral health conditions or oral diseases, encompass a range of disorders that affect the teeth, gums, and other structures within the oral cavity. These diseases include dental caries, periodontal (gum) disease, tooth loss, oral cancer, dental trauma, and birth defects such as cleft lip and palate (1). Dental disorders are usually preventable; however, their growing prevalence and impacts, such as pain, discomfort, and aesthetic issues, are a major concern (2). Populations from low socioeconomic backgrounds pose a higher burden of oral health issues across the globe (1). Evidence from the WHO Global Oral Health Status Report from 2022 suggests that worldwide, approximately 3.5 billion individuals are affected by oral disease, of which 75% belong to middle-income countries (3). Multiple sources of evidence conclude that the prevalence of dental caries is as high as 70% in lower-middle-income countries (LMICs), as compared to a 1-12% prevalence in developed countries (4). Dental caries can pose serious threats to both the oral as well as general health of an individual. Although caries has been previously identified as a disease with multifactorial causes, many risk factors are associated with it, especially in the LMICs (5). Risk factors such as oral hygiene maintenance (6), congenital and hereditary tooth defects (7), diet and eating habits (8), knowledge and practices (9, 10), socioeconomic factors (11), and health system-related factors (12) were found to be commonly associated with the increasing incidence of dental caries. Restorative treatments are usually the best standard of care in the case of dental caries, which include fillings, inlays and onlays, and root canal treatments. A root canal treatment is typically performed when the decay from dental caries reaches the dental pulp, causing inflammation of the surrounding tissues. The condition can be extremely painful, making the tooth sensitive and affecting the oral functionality of the patient. Systematic health concerns are often known to affect the efficacy of such treatments and hence should be considered before the implementation of the treatment plan. Oral infections and other diseases found in the human body usually have similar risk factors and, hence, can be associated with each other (13, 14). One notable aspect of this relationship is the shared risk factors and associations between dental diseases and systemic diseases. This interplay between oral health and systemic health underscores the importance of addressing both aspects to ensure the patient's well-being. Diabetes mellitus (DM) is a serious non-communicable comorbidity that affects the oral health of an individual. Individuals with diabetes need to be especially vigilant about maintaining good oral hygiene and seeking regular dental care. The relationship between diabetes and dental health is bidirectional, meaning that diabetes can influence oral health, and oral health can, in turn, affect diabetes management. One of the significant oral health concerns for individuals with diabetes is an increased risk of gum disease, particularly periodontitis. Diabetes can affect blood vessels, reducing the blood supply to the gums and making them more susceptible to infection. This can result in gum tissue damage and tooth loss if not properly managed (15). Another concerning issue is the association between diabetes and delayed wound healing, which extends to oral tissues. This delayed healing response can complicate dental procedures such as extractions, root canals, and oral surgeries (16). High blood sugar levels can also complicate the body's response to infection, making it essential for dental professionals to carefully consider a patient's diabetic status when planning and performing endodontic procedures.
The rationale for investigating the outcomes of surgical and non-surgical root canal treatments in diabetic patients is rooted in the critical need to comprehend the impact of diabetes on the success and complications of these dental procedures. Diabetes, a highly prevalent chronic condition globally, necessitates a thorough assessment of its potential ramifications for dental care, ensuring the development of evidence-based guidelines tailored to diabetic individuals. Given the clinical dilemma often faced by dental professionals when selecting between surgical and non-surgical root canal treatments based on individual patient factors, understanding the nuanced impact of diabetes in this decision-making process is paramount. Moreover, an exploration of whether diabetic patients exhibit varying outcomes and complications associated with surgical versus non-surgical root canal treatments can provide valuable insights for the effective allocation of healthcare resources. This study also aligns with patient-centered care by empowering diabetic individuals with comprehensive information about their root canal treatment options, enabling them to make informed decisions about their oral health.
Methods
This study, initiated on October 3rd, 2023, was conducted following a comprehensive literature review utilizing databases like PubMed, Web of Science, and Cochrane. A wide range of medical terminology combinations were employed during this literature search. Additionally, Google Scholar was utilized for manual searches of pertinent research terms. The primary focus of this literature review encompassed various aspects, including the burden of dental diseases, their pathogenesis, predisposing factors, the types of root canal treatments, the impact of diabetes on endodontic outcomes, as well as preventive and management strategies for endodontic treatment in diabetic patients. It's important to note that the selection of articles for inclusion in the study was based on multiple criteria, ensuring a thorough and robust review process.
Discussion
Root canal treatment, also known as endodontic therapy, is a dental procedure performed to treat the infected or damaged pulp (the innermost part) of a tooth. There are two primary types of root canal treatment: non-surgical RCT and surgical RCT.
Non-Surgical Root Canal Treatment
This is the most common type of root canal treatment. It starts with a local anesthesia administration to numb the affected tooth and the surrounding area to ensure that the patient does not feel any pain during the procedure. In most cases, a rubber dam is also used, which keeps the tooth isolated and free from any saliva. The dental surgeon exposes the dental pulp by creating an opening in the crown of the tooth. The infected dental pulp is then removed from the chamber as well as the canals using specialized instruments. Next, the canals are cleaned thoroughly, shaped, and disinfected to remove any remaining debris or bacteria. The canals are filled with a biocompatible material called gutta-percha to seal them off and prevent reinfection. Finally, a temporary or permanent filling material is placed in the access opening to seal the tooth. The process of a non-surgical root canal treatment has been illustrated in Figure 1. In cases where a previous root canal treatment has failed or a new infection has developed, retreatment may be necessary. The procedure is similar to a conventional root canal but involves removing the existing filling material and addressing any new infection (17).
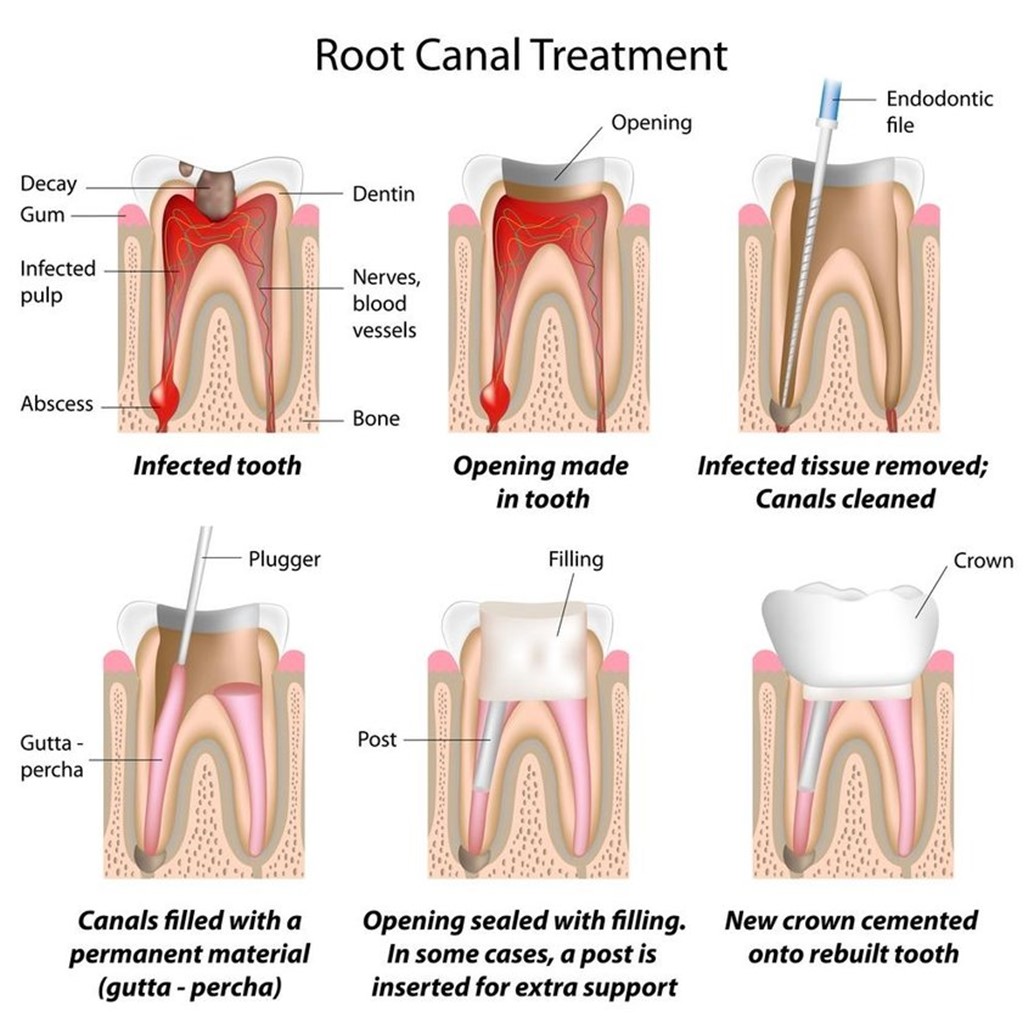
Figure 1: Non-surgical root canal treatment procedure (25)
Surgical Root Canal Treatment
This type of root canal treatment is performed when a non-surgical approach is insufficient to treat the infection or damage. This procedure is often recommended when a non-surgical root canal has not resolved the issue or when it's challenging to access and treat the root tip through the crown of the tooth (18). This approach also starts with the induction of local anesthesia to numb the affected area. A small incision is then made in the gum tissue near the affected tooth, providing access to the root tip. The infected or damaged tip of the root is removed, along with any surrounding infected tissue, and a small filling material is placed at the end of the root to seal the canal. Following the filling, the gum tissue is sutured back into place.
Endodontic outcomes and diabetes
The choice between non-surgical and surgical root canal treatment depends on the specific circumstances of the case. Non-surgical root canals are typically the first choice and are successful in most cases. Surgical root canal treatment is considered when non-surgical options are not feasible or have not yielded the desired results. Surgical root canal treatments are also the best care option in cases where apical periodontitis is persistent, causing delays in the healing of the endodontically treated tooth (18). Both surgical and non-surgical root canal treatments can be performed on diabetic patients, but there are some important considerations to keep in mind due to the unique challenges posed by diabetes. Endodontic outcomes in patients with diabetes can be influenced by various factors associated with this chronic metabolic condition. Diabetes, characterized by elevated blood sugar levels, can impact the body's healing processes, immune response, and susceptibility to infection (19). Several research studies have shed light on the connection between diabetes and endodontic outcomes, revealing important insights into the challenges faced by diabetic patients in managing their oral health (19). One notable finding is that diabetes can contribute to poor endodontic outcomes. This can be attributed to several factors, including:
Increased Risk of Periapical Abscess
Studies have shown that patients with diabetes are significantly more likely to have a higher prevalence of periapical abscesses. Periapical abscesses are localized infections around the root tip of a tooth, often resulting from a bacterial infection. The increased susceptibility to these infections in diabetic patients can complicate endodontic treatment (20).
Higher Need for Surgical Procedures
Patients with diabetes have been found to require surgical endodontic procedures more frequently. This suggests that non-surgical root canal treatments may be less effective for these individuals, necessitating more extensive surgical interventions (20).
Delayed Healing
Diabetes is associated with delayed wound healing, which extends to oral tissues. Studies have observed that endodontic procedures in diabetic patients may exhibit slower healing processes compared to non-diabetic individuals. Delayed healing can lead to prolonged discomfort and recovery times (21).
Persistent Periapical Infections
Research supports the idea that endodontic treatment can effectively reduce tooth inflammation. However, non-surgical root canal treatments are more prone to failure in patients with diabetes due to persistent periapical infections. These lingering infections can hinder the success of the procedure (22).
Radiographic Evidence
Studies have noted that the size of periapical radiolucency, a radiographic sign of periapical infection or inflammation (Figure 2), tends to be larger in patients with diabetes compared to those without the condition. This radiographic evidence reflects the challenges posed by diabetes in achieving optimal endodontic outcomes (23).

Figure 2: Preoperative radiograph revealing a periapical radiolucent lesion (26)
Considering these findings, diabetes can be regarded as a crucial preoperative prognostic factor for endodontic procedures. It underscores the need for a tailored approach to endodontic treatment in diabetic patients, with careful consideration of their unique medical condition and potential complications. While non-surgical root canal treatments remain the primary choice for most cases, the impact of diabetes on endodontic outcomes should not be underestimated.
Prevention and Management
The management of diabetic patients undergoing dental procedures, including endodontic treatments, requires careful consideration of their unique medical condition. Patients with diabetes should prioritize maintaining optimal blood glucose levels both before and after dental procedures. Elevated blood sugar levels can increase the risk of infection and significantly slow down the healing process (23). Dentists should emphasize the importance of strict glucose control, and patients should work closely with their healthcare providers to achieve and maintain target glucose levels. Moreover, dental professionals should provide detailed post-operative care instructions to diabetic patients, including information on maintaining oral hygiene, managing discomfort, and monitoring for signs of infection. Close follow-up appointments can help assess healing progress and address any issues promptly (24). In some cases, dentists may prescribe antibiotics before or after the dental procedure to reduce the risk of infection, especially for diabetic patients who may be more susceptible to bacterial infections (24). The choice of antibiotics should be made judiciously, considering the patient's medical history and potential drug interactions with diabetes medications. Collaboration between the dentist and the patient's primary healthcare provider, such as an endocrinologist or internist, can also be highly beneficial (24). Dentists should communicate with the patient's healthcare team to ensure coordinated care and to discuss any adjustments needed to the patient's diabetes management plan before and after the dental procedure. This collaboration can help optimize the patient's overall health and well-being.
Conclusion
In summary, whether it's the non-surgical or surgical approach, root canal treatment plays a pivotal role in preserving dental health when a tooth's pulp is compromised due to infection or damage. Non-surgical root canal procedures are typically the primary choice and are successful in most cases, but surgical methods are considered when non-surgical options prove inadequate, particularly in cases of persistent apical periodontitis. When dealing with diabetic patients, a complex interplay arises between diabetes and the outcomes of endodontic procedures. Diabetes, characterized by elevated blood sugar levels, introduces distinct challenges, including an elevated risk of periapical abscesses, a greater likelihood of necessitating surgical interventions, delays in the healing process, and an inclination towards persistent periapical infections. Radiographic evidence further underscores the intricacies of achieving favorable endodontic results in individuals with diabetes. It's imperative to recognize diabetes as a pivotal preoperative factor, necessitating a tailored approach to endodontic care. While non-surgical root canal treatments remain the primary preference in most cases, a comprehensive approach must be adopted. This includes maintaining strict control over blood glucose levels, prudent use of antibiotics, providing thorough post-operative care instructions, and fostering effective collaboration with healthcare providers. Such a multifaceted strategy ensures that dental care is not only efficacious but also attuned to the unique requirements and potential complications of diabetic patients, ultimately enhancing their overall health and well-being.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
