Volume 3, Issue 11
November 2023
An Overview of Vascular Malformations in the Oral and Maxillofacial Region
Ayman Bukhsh, Abdulrhman Almohammadi, Abdulkarim Alkhulaifi, Faisal Albaqawi, Hamzah Aloqayli, Abdullah Alsamnan, Rawan Alshahrani, Abdullah Alqahtani, Asim Aljohani, Ali Alshehri, Abdulaziz Zahid
DOI: http://dx.doi.org/10.52533/JOHS.2023.31103
Keywords: malformations, maxillofacial region, vascular anomalies
This review provides a comprehensive overview of vascular malformations in the oral and maxillofacial region, focusing on their historical context, classifications, clinical characteristics, and treatment options. Vascular anomalies (VA) encompass a diverse range of medical conditions affecting the body's vasculature. The study highlights the challenges in diagnosing and managing these conditions due to their varied presentations. It delves into the historical terminology, highlighting how terms like cherry, port-wine stain, and strawberry were used to describe these anomalies. The paper discusses the classification system proposed by the International Society for the Study of Vascular Anomalies (ISSVA), which categorizes vascular anomalies into tumors and malformations based on the presence or absence of endothelial mitotic activity. The importance of accurate histopathological descriptions in diagnosing and treating these anomalies is emphasized. Furthermore, the article provides a detailed discussion of the major types of vascular anomalies, including capillary malformations, venous malformations, arteriovenous malformations, and lymphatic malformations. Each type is characterized by its own unique features, clinical presentations, and associated complications. In terms of treatment, the review discusses various options, including laser therapy, sclerotherapy, embolization, and surgical resection, highlighting the factors that influence treatment decisions, such as lesion type, location, and extent.
Introduction
The term vascular anomalies (VA) encompass a wide range of medical conditions affecting the vascular structures within the human body. Mulliken and Glowacki's classification provide an understanding of these conditions on a biological level. However, the difficulty in diagnosing and treating VA largely stems from the diverse ways it can manifest (1). Treatment options for VA span from medical approaches to less invasive interventions and, in some cases, more aggressive methods. In 1818, a London surgeon named Wardrop was the first to distinguish vascular malformations from hemangiomas (2). However, this differentiation did not contribute to the development of a treatment philosophy. Notably, in 1846, William Green Morton conducted the first public demonstration of ether anesthesia for the surgical removal of a venous vascular malformation (3). Throughout history, medical professionals have often referred to cutaneous vascular nevi using familiar food-related terms. Expressions like "cherry," "port-wine stain," and "strawberry" to describe vascular lesions can be traced back to the erroneous belief in maternal impressions (1). As histopathology emerged in the mid-nineteenth century, these anomalies came to be known as angiomas. However, over the next century, clinical and histological terminology became muddled, hindering the progress of this field.
Vascular anomalies are conditions involving the endothelium and surrounding cells, which can impact any part of the body's vascularity (4). They are typically diagnosed during infancy or childhood, with an estimated prevalence of 4.5% (5). Among the challenges associated with vascular anomalies, psychological distress due to disfigurement and functional impairments is common, particularly when lesions affect the head and neck. These anomalies can lead to various local complications, such as bleeding, infection, obstruction, pain, thrombosis, ulceration, and damage to anatomical structures. They can also result in general complications like congestive heart failure, disseminated intravascular coagulation, pulmonary embolism, thrombocytopenia, and sepsis (6). Accurate histopathological descriptions play a crucial role in diagnosing and treating these anomalies, in conjunction with clinical and radiological assessments. However, traditional terminology has continued to lead to misdiagnoses, inappropriate treatments, and hindered research. Recognizing this issue, the International Society for the Study of Vascular Anomalies (ISSVA) developed a classification system based partly on the work of Mulliken and Glowacki (7). This system categorizes vascular anomalies into tumors and malformations, considering the presence or absence of endothelial mitotic activity. Nevertheless, it has become clear that relying solely on endothelial mitotic activity is insufficient for classification, as mitotic activity can occur as a secondary response to ischemia and turbulence.
In this article, we provide an overview of the current clinical characteristics that distinguish the major types of vascular anomalies affecting the head and neck.
Methodology
This study is based on a comprehensive literature search on October 7, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed vascular malformations in the oral and maxillofacial regions. There were no restrictions on date, language, participant age, or type of publication.
Discussion
The International Society for the Study of Vascular Anomalies (ISSVA) proposed its first classification in 1988 in Hamburg, which is known as the Hamburg classification. It has been reviewed and modified several times since then: in 1992 in Colorado, in 1996 in Rome, and most recently in 2014 in Melbourne (8). The author introduced a more practical classification to aid in decision-making with respect to diagnostic imaging and surgical planning, as follows (Table 1) (2):
|
Table 1: Classification of vascular anomalies based on their location and depth within the head and neck region, along with the corresponding surgical approaches and reconstruction methods required for each type. |
||
|
Type |
Anatomy and Depth Consideration |
Surgical Approach and Reconstruction |
|
Type I |
Superficial |
Excision of Skin or Mucosa, Utilization of Local or Regional Flaps for Reconstruction |
|
Type II |
Submucosal |
Complete Excision Following Elevation of Skin Flaps |
|
Type III |
Gland-Related |
Excision Along with the Affected Gland |
|
Type IV |
Intraosseous |
Excision Involving the Affected Bone, Reconstructive Procedures as Needed |
|
Type V |
Deep Visceral |
Skeletal Access Osteotomy for Full Exposure and Total Excision |
Vascular Malformations
Vascular malformations are abnormalities in the development of blood vessels and are characterized by the presence of stable, mature vascular endothelium. They affect both males and females equally and are congenital, although some may not become apparent until later in life. Unlike hemangiomas, vascular malformations do not proliferate or spontaneously regress but rather grow gradually throughout a person's life, simultaneously with the individual's growth (9, 10). Trauma, puberty, and pregnancy can accelerate their growth. These malformations are classified based on the predominant vessel type and flow characteristics. Notably, they are often associated with skeletal abnormalities in up to 35% of cases.
Venous Malformations
Venous malformations are characterized by an abnormal collection of veins that lack demonstrable mitotic activity in endothelial or pericyte cells and often lack a uniform smooth muscle layer. The extent of dilation increases with age, and clinical features depend on the depth and size of the lesion. These lesions are typically soft and compressible and enlarge when venous pressure increases (Figure 1) (11).

Figure 1: Venous malformation of the upper lip in an adult (11).
Phleboliths may also be present within the lesion. It is not uncommon to observe changes in the adjacent skeleton, often taking the form of bony hypertrophy or distortion. Venous malformations can occasionally be entirely intraosseous, with the mandible being the most frequently affected bone, although maxillary, nasal, and frontal lesions have been reported. It is believed that many lesions described as "intraosseous hemangiomas" are actually venous malformations. The choice of treatment for venous malformations depends on factors such as the lesion's depth, extent, anatomical location, and the clinician's experience and preference. Available methods include lasers, excision, sclerotherapy, or combinations thereof (11). Smaller lesions may be effectively treated with excision or sclerotherapy. Complete resection is essential for preventing recurrence, and appropriate imaging is crucial for assessing the full extent of the lesion, especially in cases of large lesions. Acquired adult venous malformations, often observed as small venous lakes in the lower lip and face, can be treated with laser photocoagulation or excision. Cryotherapy may benefit small intraoral lesions but can result in hypopigmentation and scarring in cutaneous lesions. Nd:YAG lasers are commonly used for treating superficial lesions or the superficialcomponent of a compound lesion, as these lesions often involve large vessels (12). Initial laser treatment can create a relatively avascular plane for raising a flap to access deeper lesions while preserving the cutaneous and mucosal surfaces. However, laser treatment is often palliative, and recurrences that require repeated treatments are common. For larger venous malformations, a combination of sclerotherapy and excision or sclerotherapy alone is often employed. Various sclerosing agents, such as sodium tetradecyl sulfate, 100% ethanol, and Ethibloc, have been used, but comparative trials are lacking. Resection can be challenging, especially for extensive lesions. Complete excision is necessary to prevent recurrence, but this must be balanced against the potential complications of radical surgery. Contact lasers and thermoscalpels can help minimize blood loss, and staging the resection may be necessary for more extensive lesions. Residual or recurrent lesions can be treated with excision or sclerotherapy.
Lymphatic Malformations
Lymphatic malformations represent a range of disorders that manifest in various ways, often during childhood and adolescence. Over 75% of lymphatic malformations are found in the neck, and their clinical presentation varies based on factors such as the extent and depth of the lesions and the degree of fibrous reaction surrounding them (13-15). Mucosal and cutaneous involvement leads to the formation of multiple fluid-filled vesicles, which may communicate with larger and deeper lymphatic cisterns. These malformations are classified into microcystic, macrocystic, and combined lesions based on the size of the vesicles (11). Typically, cervical lesions are of the macrocystic variety, known as cystic hygromas, while those affecting the floor of the mouth, cheek, and tongue are more likely to be diffuse microcystic lesions, referred to as lymphangiomas. High-grade lesions, which present earlier in life, tend to be more aggressive and prone to complications such as infection, bleeding, airway obstruction, speech disturbances, and abnormal facial growth. These complications can lead to hypertrophy of both soft tissue and the skeleton, with the skeletal changes thought to result from distortion of the functional matrix or direct involvement of the bone by abnormal lymphatic channels (Figure 2).
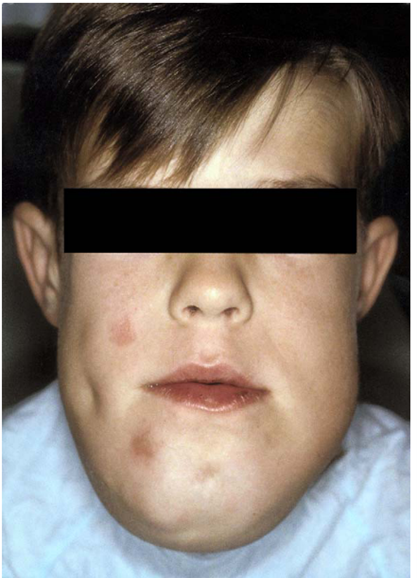
Figure 2: Lymphatic malformation of the floor of mouth and submental region with mandibular hypertrophy (11).
The primary defect is believed to be at the level of the efferent channels, and obstruction at this level (either relative or absolute) results in the dilation of proximal channels that contribute to the mass. Treatment options include laser ablation, excision, and sclerotherapy (16). Carbon dioxide laser is suitable for superficial mucosal lesions. When performing laser ablation, it's essential to ensure the destruction of most or all connected cisterns, as fluid-filled vesicles are typically linked to deeper cisterns (14, 15). Recurrences can occur and should be treated similarly. Excision is the preferred method for treatment, particularly for localized macrocystic lesions, while diffuse microcystic lesions may require multiple surgeries. Care must be taken to identify and preserve vital structures, as tissue planes are often distorted. Postoperative lymphedema can be a significant issue, especially after lesions in the floor of the mouth, where swelling and protrusion of the tongue may take up to a year to subside. Skeletal hypertrophy and malocclusion may necessitate orthognathic techniques for correction. Sclerotherapy is a promising option, but its efficacy is not yet fully evaluated. It can be used as a definitive treatment or for palliation when surgery's morbidity outweighs the benefits.
Capillary Malformations
Capillary malformations, like other vascular malformations, do not regress spontaneously. They tend to darken and thicken with age, and the rate of progression may be influenced by factors such as the degree of autonomic nerve innervation, hormonal influences, and trauma. Recent studies have highlighted the psychological impact of these birthmarks and suggested earlier interventions to mitigate undesirable psychosocial effects. Pulsed dye laser therapy, utilizing wavelengths such as 577 nm, and more recently, 585 nm, is considered the treatment of choice for capillary malformations (17-21). The concept of selective thermolysis, which involves coagulating a specific target chromophore (oxyhemoglobin) without damaging surrounding tissues, is crucial for effective treatment. While pulsed dye laser is the preferred choice, lesions resistant to this treatment may respond to other lasers, such as KTP, copper vapor, argon, or new laser technologies (22, 23). However, it is important to note that complications like scarring and pigmentation changes are more common with some of these alternative lasers. Multiple treatments, typically ranging from two to six sessions, may be necessary, with response rates varying widely. The depth, color, and location of the lesion, age at treatment, and the number of treatments administered can all impact the response to treatment. Recurrence rates have been reported, necessitating potential follow-up treatments depending on the rate of recurrence.
Arteriovenous Malformations
Arteriovenous malformations typically exhibit slow but relentless growth. High-grade lesions present earlier in life and expand more rapidly, while low-grade lesions present later and expand more slowly. Timely intervention is advisable to prevent complications and reduce the extent of the required resection. The decision to intervene should consider factors like the patient's age, lesion location, flow characteristics, treatment morbidity, and the risks of leaving the lesion untreated. Treatment should aim to completely eliminate the nidus, which is the fundamental abnormality, as even a small residual nidus can expand and lead to recurrence. Treatment options include embolization, resection, or combinations of both. Embolization is beneficial for larger arteriovenous malformations and can be used as a sole treatment or as an adjunct before excision (11). When embolization is performed, it should proceed "distal to proximal" to ablate both the nidus and its blood supply. Surgery aims for complete nidus removal and may require the sacrifice of structures, including muscle, skin, mucosa, cartilage, and bone, depending on the lesion's extent. Early access to feeding vessels is crucial for hemostasis and contact lasers and thermoscalpels can help minimize blood loss. Proximal ligation of feeding vessels should be avoided if they do not enter the nidus to allow further embolization and prevent collateral development from the internal carotid system. Intraoperative doppler examination and bleeding patterns at the resection margin can point to the completeness of the resection.
Conclusion
Vascular malformations in the oral and maxillofacial regions shed light on their historical context, classifications, clinical characteristics, and treatment options. Vascular malformations are complex conditions with diverse manifestations, often causing physical and psychological distress. Accurate histopathological descriptions and the ISSVA classification system are crucial for diagnosis and management. Various treatment modalities, including laser therapy, sclerotherapy, embolization, and surgery, offer options tailored to the type, location, and extent of the lesions.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, and final writing of the manuscript.
