Volume 2, Issue 11
November 2022
Prevalence and Management of Renal Impairment in Adults with Type 2 Diabetes Mellitus in specialized diabetes clinics in Primary Care in the Kingdom of Bahrain
Abeer AlSaweer, Fatema Qambar, Hanan Humaidan, Sumaya Al Doseri, Najat Shabeeb, Taghreed AlAlayan, Taybaa AlAradi, Ghadeer Ahmed, Fatima Hussain, Khulood AbdulJaleel, Ruqaya Al Ekri, Salman Taheri
DOI: http://dx.doi.org/10.52533/JOHS.2022.21116
Keywords: diabetes mellitus, diabetes nephropathy, estimated GFR, albuminuria
Introduction: Diabetes nephropathy is a consequence of Diabetes Mellitus (DM) and is a leading cause of End-Stage Renal Disease (ESRD). Diabetes nephropathy is a metabolic disease and can be prevented through the proper monitoring of glycaemic control levels and kidney function, which is done using estimated glomerular filtration rate (eGFR). There is a sparsity of data addressing diabetes nephropathy in the Kingdom of Bahrain; hence, this research was undertaken to the prevalence of diabetes nephropathy in Bahrain, its associated risk factors, and clinical management practices.
Methodology: A retrospective cross-sectional study took place in the central diabetes clinics (CDCs) of seven primary healthcare units (PHUs) in Bahrain, for the period from February to April 2020. Inclusion criteria included type 2 diabetes patients, aged 18 years and above, following up with the CDCs during the period from February to April 2020. The exclusion criteria included type 1 diabetes patients, patients under the age of 18, patients with renal transplants, and pregnant women. Other variables included demographic data, biochemical and clinical data, e-GFR, albuminuria status, medication prescriptions, and secondary care nephrology referrals.
Results: A total of 2,125 patients were enrolled in the study, with 16.3% suffering from chronic kidney disease at stages 3, 4 and 5. Strong correlations were found between low eGFR and certain variables, including HbA1c, blood pressure and age. A multivariate logistic regression analysis revealed that increased age, HbA1c, and systolic blood pressure were associated with a higher risk of an eGFR of less than 60 mL/min/1.73 m2.
Conclusion: This study highlighted that the prevalence of renal impairment in people with DM in Bahrain is high with a detrimental economic impact. Further studies with longitudinal patterns need to be performed to verify the true impact of this illness.
Introduction
Worldwide, Diabetes Mellitus (DM) is the main leading cause of Chronic Kidney Disease (CKD) and End-Stage Renal Disease (ESRD) (1-7). In such cases, it is referred to as Diabetic Nephropathy (DN) or Diabetic Kidney Disease (DKD) (8). It is defined as the progressive deterioration of the renal structure or function through different stages (2, 5, 9, 10).
Increases in the prevalence of DM have raised the incidence of its associated microvascular complications like DN (1, 4-6, 10, 11). A third of patients with DM suffer from CKD. In fact, every 24 hours, 160 patients with DM commence treatment for renal failure (11, 12). Various modifiable and non-modifiable risk factors contribute to the development and progression of DN. Non-modifiable risk factors include age, gender, ethnicity and family history. On the other hand, modifiable risk factors include hyperglycaemia, elevated glycosylated haemoglobin (HbA1c), high blood pressure, dyslipidaemia, metabolic syndrome, cardiovascular disease, alcohol consumption, nutritional status, obesity, smoking, presence of diabetic retinopathy and/or neuropathy (1, 4, 6-8).
In addition to increased morbidity and mortality, CKD is linked to a rise in economic costs (1, 2, 4-6, 8, 11-13), thus, the proper management of DM and DN is crucial. Moreover, in patients with Type 2 DM, DN screening by testing for albuminuria, using the Albumin to Creatinine Ratio (ACR) and estimated Glomerular Filtration Rate (eGFR), is initially recommended at the time of diagnosis, and is repeated on an annual basis if normal, or as indicated if abnormal (5, 6, 8, 9, 12).
The management of glycaemic (HbA1c < 7%) and blood pressure (BP <140/90 mmHg) levels, in addition to using Angiotensin-Converting Enzyme (ACE) inhibitors or Angiotensin Receptor Blockers (ARB), is recommended to mitigate nephropathy. Patients with macroalbuminuria or Stage 4 CKD at an eGFR of less than 30 ml/min/1.73m2, should be referred to a nephrologist (12).
The Gulf Cooperation Council (GCC) countries have the world’s second highest age-adjusted prevalence of DM at a rate of 10.8%. In fact, Bahrain’s national health survey estimated a 14.3% prevalence of DM, among 20 to 64 year olds, representing the most socially and economically productive groups (14). In 2015, the cost brought about by DM in Bahrain was estimated to be USD 277.9 million; this includes costs of admissions and complications. Thus, the prevalence of Type 2 DM put a significant socioeconomic burden on the healthcare system (15).
Several studies were conducted in the GCC focusing on this very field. For instance, a 2014 registry-based retrospective study was carried out in Saudi Arabia by Rubean et al., where 54,670 patients were sampled, resulting in an overall estimated prevalence of DN in DM patients at 10.8%, categorised into microalbuminuria in 1.2%, macroalbuminuria in 8.1%, and ESRD in 1.5% (7). Moreover, another study was carried out in Saudi Arabia by Alrehaili et al. in 2018, where DN was identified in 16.4% of 122 patients undergoing renal biopsy, regardless of the presence or absence of additional non-diabetic renal diseases (10).
Another Kuwaiti 2012 study conducted by Aboelnasr et al., showed that among 153 newly diagnosed DM patients, 43.5% had albuminuria, categorised into 27.3% microalbuminuria and 16.2% macroalbuminuria (16). While, in Oman, a 2006 observational study conducted by Al-Futaisi et al. estimated a 27% prevalence of proteinuria in 251 DM patients (17). Another Omani 2012 cross-sectional study, by Alrawahi et al. which was conducted on 699 DM patients showed a 42.5% prevalence of DN in DM patients (13).
Similarly, in the Kingdom of Bahrain, a 2009 study conducted by Salman et al. on 712 DM patients attending nine primary healthcare centres showed a 27.9% prevalence of albuminuria, of which 22% was microalbuminuria and 5.9% was macroalbuminuria. The study also revealed an association between age, DM duration, and poor DM control with the development of albuminuria (5).
With the consideration of several factors, including the lack of detailed recent studies regarding this issue in the Kingdom of Bahrain, this study was conducted to assess the prevalence and proper management of renal impairment to decrease the progression of DN among adults with Type 2 DM attending primary healthcare centres.
Methodology
Study Setting and Sample Population
This cross-sectional study was conducted on adults with Type 2 DM, aged 18 years and above, attending primary healthcare centres in Bahrain for DM care. Electronic medical records of patients attending the central diabetes clinics at seven Primary Healthcare Units (PHU) during the period from February to April 2020, were included in the study. All patients who met the inclusion criteria were enrolled in the study. Patients were identified using assigned identification numbers, to avoid bias and maintain their anonymity.
The inclusion criteria consisted of DM patients aged 18 years and above, following up at central diabetes clinics in PHUs during the period from February to April 2020. The exclusion criteria ruled out patients with Type 1 DM, Type 2 DM but younger than 18 years old, non-diabetic kidney disease, renal transplants, recent CT scans done with contrast, pregnancy, and patients undergoing treatments that can affect blood glucose control levels or kidney function – specifically cancer therapy and immunosuppressants.
Definitions
Five stages of kidney disease are identified based on eGFR:
Stage 1: normal or high eGFR of ?90 mL/min/1.73m2
Stage 2: mildly decreased eGFR of 60-89 mL/min/1.73m2
Stage 3a: mildly to moderately decreased eGFR of 45-59 mL/min/1.73m2
Stage 3b: moderately to severely decreased eGFR of 30-44 mL/min/1.73m2
Stage 4: severely decreased eGFR of 15-29 mL/min/1.73m2
Stage 5: kidney failure at eGFR of <15 mL/min/1.73m2
In terms of ACR, a normal ACR is at less than 30 mg/g, while an ACR of 30 to 299 mg/g is categorised as microalbuminuria and an ACR of more than or equal to 300 mg/g is categorised as macroalbuminuria. Two out of three abnormal ACR specimens taken within a period of 3 to 6 months are required in order to confirm the presence of albuminuria in the absence of other causes (12).
The targeted sample size was calculated using the sample size formula for infinite populations. By quoting a prevalence of albuminuria in DM patients in Bahrain in 2009 of 28%(5), a margin of error of 5% and a confidence interval of 95%, a sample size of at least 306 central diabetes clinic patients from each PHU was determined.
Data Instrumentation
The data instrument devised for the study included
Demographic data, BMI (kg/m2), and the latest recorded blood pressure (mmHg), HbA1c (mmol/mol) and LDL (mmol/L) reports within the past year; as well as, any antidiabetic, ACE or ARBs medications, and lipid-lowering agents.
The status of dysalbuminuria within the past two years, recorded as either positive, negative, or undetermined. The status was determined by reviewing spot urine ACR over the past two years. The patient was considered to be dysalbuminuric if two out of the three samples were above 3.5 mg/mmol over a period of 3 to 6 months.
The latest e-GFR mL/min/1.73 m2 readings recorded over the past year. Metformin dosage and nephrology referrals were also recorded.
Statistical Analysis
Statistical Package for Social Sciences (SPSS) software Version 22 was used for data entry and statistical analysis. Frequencies and percentages were used to represent categorical data, while means and standard deviations were used to represent quantitative data. A Chi-squared test was used to test relationships between categorical variables, a t-test was used to test the significant differences between the two combined eGFR stage groups as opposed to other continuous variables, and an analysis of variance F-test was used to calculate the difference between quantitative variables in more than two groups. The “Enter” method was used on a multivariate logistic regression model to depict the association of eGFR (<60, or ?60 ml/minute/1.73 m2) and other risk factors, such as age, BP, and HbA1c. A p-value of less than 0.05 was considered as statistically significant.
Ethical Approval
The approval to conduct the study was obtained from the Primary Care Ethical Committee. Patient confidentiality was ensured by assigning them with identification numbers, which were disposed of after the end of the research. In addition, the beneficence and non-maleficence of Type 2 DM patients, from screening to comprehensive management, were set as an objective.
Results
This retrospective cross-sectional multi-centric study was undertaken to estimate the prevalence of renal impairment in Type 2 DM patients attending PHUs in Bahrain. Data cleaning was performed by omitting duplicates, unifying HbA1c measures, and deleting cases with >20% of missing data.
Patient Characteristics
A number of 2,125 central diabetes clinics patients from the seven health centres were enrolled in the study. After data cleaning, 2,090 eligible candidates were identified for analysis. Both genders were almost equally represented, with 53.7% females and 46.3% males. The mean age of the cohort was at (59.3 ± 10.1) years. Glycaemic control analyses showed a mean HbA1c of (70.5 ± 20.4) mmol/mmol. The mean of total cholesterol, triglyceride, and LDL were at (4.0±1.0) mmol/L, (1.8±1.8) mmol/L, (2.0±0.9) mmol/L, respectively. Mean systolic and diastolic blood pressure were at (131.5±22.0) mmHg and (75.2±12.6) mmHg, respectively. The mean BMI was (29.9± 9.6) kg/m2. The mean eGFR for patients in this cohort was at (86.3±30.3) mL/min/1.73m2 (Table 1).
|
Table 1: Patients’ characteristics |
||
|
Frequency |
Mean ± SD |
|
|
Gender Female Male |
1122(53.7%) 968(46.3%) |
|
|
Age |
59.3(10.1) years |
|
|
HbA1c |
70.5 (20.4) mmol/mmol |
|
|
Total Cholesterol |
4.0(1.0) mmol/L |
|
|
Triglycerides |
1.8(1.8) mmol/L |
|
|
LDL |
2.0(0.9) mmol/L |
|
|
Systolic BP |
131.5(22.0) mmHg |
|
|
Diastolic BP |
75.2(12.6) mmHg |
|
|
BMI |
29.9(9.6) kg/m2 |
|
|
E-GFR |
86.3(30.3) mL/min/1.73m2 |
|
Medications and Nephrology Referrals
Out of the 2,090 cases with recorded eGFR levels, 1,253 (59.95%) used renin-angiotensin-aldosterone system (RAAS) inhibitors, 1,883 (90.09%) used statins, and a majority of 1,842 (88.13%) used metformin, which was the most prescribed antidiabetic medication, at an average dose of 1,860 mg. Furthermore, 1,565 (74.88%) used DDP-4 inhibitors, 1,410(67.46%) used sulphonylureas, and 1,005 (48.09%) used insulin. In addition, SGLT-2 inhibitors and GLP-1 analogue were prescribed for 255 (12.20%) and 53 (2.53%) cases, respectively. Out of all cases in this sample, 237 (11.34%) were referred to nephrology clinics in secondary care.
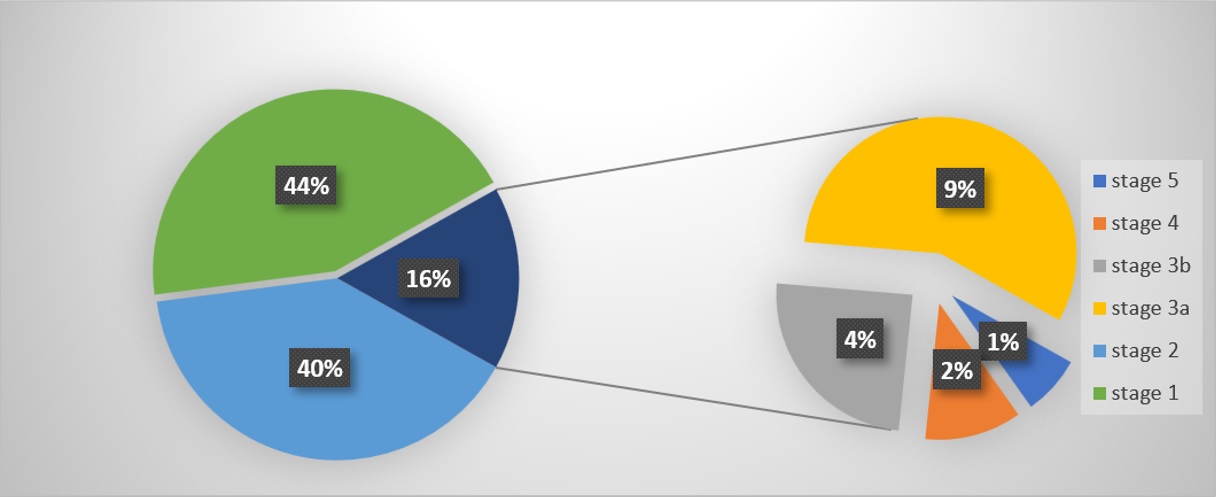
CKD Staging – eGFR
With respect to CKD stages, eGFR data were available for 2,090 (98.4%) patients. The number of CKD Stage 3a (eGFR, 45-59mL/min/1.73m2), Stage 3b (eGFR, 30-44mL/min/1.73m2), Stage 4 (eGFR, 15-29mL/min/1.73m2), and Stage 5 (eGFR, <15 mL/min/1.73m2) cases were 193(9.23%), 85(4.07%), 39(1.87%), and 24(1.15%) respectively, collectively constituting 16.31% of this cohort (Figure 1).
CKD Staging – eGFR and albuminuria
Table 2 shows the diagnosis of kidney disease in people with DM using eGFR and albuminuria. Out of the 2,087 (98.21%) cases with recorded albuminuria values, 26.42%, 37.65%, 52.50%, and 70.08% were positive at stages 3a, 3b, 4 and 5, respectively. Whereas 569 (28%) patients’ albuminuria statuses were undetermined.
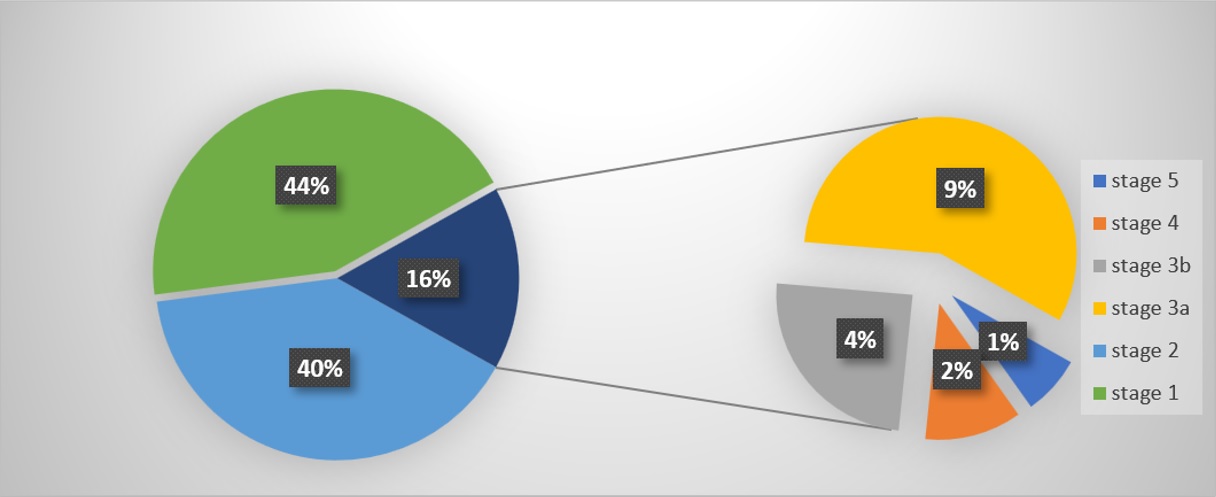
Figure 1: Percentages of stages of CKD
|
Table 2: CKD staging by e-GFR and albuminuria |
|||||||
|
CKD results based on Albuminuria status and e-GFR |
Albuminuria categories% |
||||||
|
Total# |
Negative 1215 |
Positive 304 |
Undetermined 569 |
||||
|
e-GFR categories |
G1 |
Normal or high |
?90 |
916 |
613 (66.92%) |
82 (8.95%) |
221 (24.13%) |
|
G2 |
Mildly decreased |
60-89 |
830 |
479 (57.71%) |
101 (12.17%) |
250 (30.12%) |
|
|
G3a |
Mildly to moderately decreased |
45-59 |
193 |
86 (44.56%) |
51 (26.42%) |
56 (29.01%) |
|
|
G3b |
Moderately to severely decreased |
30-44 |
85 |
26 (30.59%) |
32(37.65%) |
27 (31.76%) |
|
|
G4 |
Severely decreased |
15-29 |
39 |
10 (25.00%) |
21 (52.50%) |
9 (22.50%) |
|
|
G5 |
Kidney Failure |
<15 |
24 |
1 (0.04%) |
17 (70.08%) |
6 (25.00%) |
|
# 2 Missing Albuminuria data
DM and BP Control
Out of the 2,090 patients, a majority of 918(43.92%) patients’ HbA1c was from (53 to 75mmol/mmol), and 764 (36.55%) patients had HbA1c levels of (75mmol/mmol and above). On the other hand, 415 (19.86%) patients achieved their therapeutic target of HbA1c (<53mmol/mmol). Furthermore, 1,405 (67.22%) patients achieved systolic blood pressure (<140), and 1,892 (90.53%) patients achieved diastolic blood pressure (<90). According to the American Diabetes Association’s standards, DM patients with stages 1 and 2 of CKD are grouped under one category, while stages 3 to 5 are grouped under another.
Patients' Characteristics and Biochemical Data
Table 3 shows that groups with lower eGFR were at a more advanced age at (65.7±8.49) years (P<.001), had lower HbA1c levels at (67.2±21.6), and had higher systolic blood pressure at (134.5±26.3) (P=.004) and lower diastolic blood pressure at (72.7±14.8) (P<.001).
|
Table 3 Difference in patients' characteristics and biochemical data between categories of CKD. |
|||
|
1-2 (1749) |
3-5 (341) |
P Value |
|
|
Gender: Female Male |
976(55.8%) 773(44%) |
183(53.7%) 158(46.3%) |
.468 |
|
Age |
(58 ±9.93) years |
(65.7±8.49) years |
<.0001** |
|
HbA1c |
(70.9±20.2) mmol/mmol |
(67.2±21.6) mmol/mmol |
.0015** |
|
Total Cholesterol |
(4.05±1.06) mmol/L |
(4.04±1.08) mmol/L |
.882 |
|
Triglycerides |
(1.82±2.8) mmol/L |
(1.88±1.2) mmol/L |
.6833 |
|
LDL |
(2.16±2.69) mmol/L |
(2.1±1.09) mmol/L |
.70 |
|
Systolic BP |
(130.85±21.2) mmHg |
(134.5±26.3) mmHg |
.0044** |
|
Diastolic BP |
(75.68±12.16) mmHg |
(72.7±14.8) mmHg |
<.0001** |
|
BMI |
30.0(9.13) kg/m2 |
(29.8±11.7) kg/m2 |
0.78 |
** Sig (α<0.01)
Medication Prescriptions and Nephrology Referrals
Table 4 depicts differences in medication prescription trends between both CKD groups. It identifies that groups with lower eGFR were prescribed more RAAS (ACE and ARB) inhibitors and insulins (P<.001), and less DDP-4 inhibitors, metformin, sulphonylureas, and SGLT-2 inhibitors (P<.001). Furthermore, lower doses of metformin were prescribed at (1315.8±796.00) (P<.001). Additionally, secondary care nephrology referrals were more common in patients with lower eGFR (P<.001).
|
Table 4 difference in medication use between both groups of CKD |
|||
|
Stage 1-2 (1749) |
Stage 3-5 (341) |
P Value |
|
|
RAAS # ACE ARB Neither |
490(28%) 507(29%) 752(43%) |
127(37.2%) 104(30.7%) 110(32.25) |
<.001** |
|
Statin Yes No |
1558(89.1%) 191(10.9%) |
300(88%) 41(12%) |
.553 |
|
DPP-4 inhibitors### Yes No |
1327(75.9%) 422(24.1%) |
225(66.1%) 116(33.9%) |
<.001** |
|
Sulphonylureas Yes No |
1202(68.7%) 547(31.3%) |
193(56.7%) 148(43.3%) |
<.001** |
|
GLP-1 Yes No |
47(2.7%) 1702(97.3%) |
7(2%) 334(98%) |
.50 |
|
Metformin : Yes No |
1625(92.9%) 124(7%) |
206(60.4%) 135(39.6%) |
<.001** |
|
Insulin : Yes No |
780(44.6%) 969(55.3%) |
202(59.2%) 139(40.8%) |
<.001** |
|
SGLT-2 inhibitors Yes No |
229(13.1%) 1520(86.9%) |
25(7.4%) 316(92.6%) |
.003** |
|
TZDs Yes No |
1728(98.8%) 21(1.1%) |
339(99.3%) 2(0.7%) |
.567 |
|
Metformin dose (mg) Mean ± SD |
1934.0± 737.85 |
1315.8± 796.00 |
<.001** |
|
Nephrology referral Yes No |
75(4.3%) 1674(95.7%) |
139(40.9%) 202(59.1%) |
<.001** |
* Sig (α<0.01)
Lower CKD Stages Practices
Further analysis is required to verify certain clinical practices for patients with lower eGFR. Referrals to secondary care nephrology were significantly higher and metformin doses were significantly lower with stage 4 and 5 cases, when compared to stage 3 (Table 5).
|
Table 5 Secondary care nephrology referral and metformin dose in lower CKD stages |
|||
|
CKD Stages |
P Value |
||
|
3 N=277# |
4+5 N=63 |
||
|
Nephrology Referral Yes No |
106(38%) 171(62%) |
55(88%) 8(12%) |
<.001** |
|
Metformin dose |
1412±752.00 mg |
434±811.66 mg |
.039* |
# 1 missing case, * Sig (α<0.05), ** Sig (α<0.01)
Multivariate Logistic Regression Analysis
The adjusted multivariate logistic regression results demonstrate that several factors were associated with an increased risk of falling under the lower eGFR group, such as advanced age (OR 1.064, 95% CI:1.045,1.083), high HbA1c (OR 1.009, 95% CI:1.002,1.017), and high systolic blood pressure was associated with a higher risk of an eGFR of less than 60 mL/min/1.73 m2 (OR 1.011, 95% CI:1.003,1.020) (Table 6).
|
Table 6 Multivariate logistic regression |
||||
|
Variable |
OR |
CI 95% |
Sig |
|
|
Lower |
Upper |
|||
|
Age |
1.064 |
1.045 |
1.083 |
<.001** |
|
HbA1c |
1.009 |
1.002 |
1.017 |
.016* |
|
Sys |
1.011 |
1.003 |
1.020 |
.009* |
|
Dia |
.984 |
.969 |
.999 |
.035 |
|
BMI |
.993 |
.978 |
1.009 |
.380 |
|
Gender |
.770 |
.566 |
1.049 |
.097 |
* Sig (α<0.05), ** Sig (α<0.01)
Discussion
As far as can be determined from the research conducted, this study is the first epidemiological study on the prevalence of CKD in the Kingdom of Bahrain among PHU patients. The prevalence of CKD among the sample population, which was made up of high-risk diabetics, is comparable to that of neighbouring countries. For instance, in Saudi Arabia, a 2018 study conducted by Rehaili et al. on 122 DM patients (10) showed a prevalence of 9%. However, in Palestine, a 2020 study by Nazzal et al. sampled 386 patients with DM and reported a CKD prevalence of 23.6% (18). Such varying results on the prevalence of CKD among DM populations may be attributed to differences in the implemented diagnosis criteria and characteristics of the sampled populations. Since the central diabetes clinic is mainly a referrals clinic, there was a relatively high prevalence of CKD amongst this study’s cohort.
To demonstrate, the recorded means of HbA1c and BP were 70 mmol/mol, and 131/75, respectively, which are acceptable parameters for this study’s high-risk DM population. In comparison, a 2019 retrospective study conducted by Qaddoumi et al. on 963 DM patients attending Dasman Centre in Kuwait, reported a mean HbA1c of 69 mmol/mol, with 29.5% of patients with good glyceamic control (HbA1c level < 7%) (19). Another similar cross-sectional Kuwaiti study was conducted using electronic medical records of 7,657 DM patients and reported that only 25% realised glycaemic control (20). The practice of monitoring HbA1c as a performance indicator is done to measure change over a one-year period rather than to merely rely on a depiction of the latest HbA1c levels (19).
As a matter of fact, the standards of DM care adopted at the central diabetes clinics include the prescription of statin, and RAAS inhibitors for lower eGFR cases, as well as insulin for higher risk cases at eGFR of less than 60. This is done in addition to lowering LDL and BP levels, decreasing doses of metformin, and providing appropriate referrals to nephrology clinics for lower eGFR cases (21). Contrastingly, such a level of commitment towards the standardisation of DM care was not observed in an earlier study that was done in Bahrain, where 0% of its sample population were tested for albuminuria (22).
Additionally, a more advanced age significantly increases the risk (p-value <0.0001) of CKD. In fact, the overall prevalence of CKD among older people may be attributed to the decrease in eGFR with normal aging, accompanied by the high rate of comorbidities among older populations. Likewise, in a 2020 study conducted by Nazzal et al. on 386 patients with DM, a multivariate regression analysis showed that cases aged ? 60 were predicted to have poorer eGFR levels (18).
Furthermore, decreased HbA1c levels are found among advanced CKD patients due to the shorter lifespan of red blood cells, in addition to the carbamylated haemoglobin molecules’ resistance to glycosylation in uremic toxin molecules (8). Age, HbA1c, and systolic blood pressure are associated with lower eGFR levels and are known risk factors of the progression of CKD (18).
The Kidney Failure Risk Equation (KFRE) devised by the National Kidney Foundation, uses the four variables of age, gender, urine ACR, and eGFR in individuals with CKD to predict the risk of ESRD, i.e., the need to undergo dialysis or kidney transplant (23-26). The equation was adopted to estimate the mean 2-year and 5-year predictions of ESRD among a subgroup of the sample, with an eGFR falling between 10 and 60 mL/min/1.73 m2. Resulting in a calculated mean of 6.3% and 14% for the 2-year and 5-year predictions of ESRD, respectively, which cautions decision-makers on a future increase in expenditure on DM cases, if no conclusive measures are initiated.
On the contrary, this study’s sample population’s mean BMI was at 29.9 but signified no correlation with lower eGFR levels. Similarly, in a 2019 study done by Elhefnawy et al. on 151 DM patients, BMI was not significantly high among lower eGFR cases (1). This may be due to the subtle BMI variances among cases at different CKD stages, alongside the relatively low BMI of the sampled patients.
Nevertheless, the study faced some limitations, including the fact that it is a cross-sectional, and not a longitudinal, analysis, which may prevent any causal associations between CKD and its risk factors. Additionally, there was insufficient data on albuminuria, hindering the proper categorisation of patients under CKD subgroups, which leads to delays in the initiation of therapeutic actions. Furthermore, there was insufficient data on the sample population’s comorbidities, drug regimens, and duration of DM, rendering the interpretation of data cautious. Also, it is of importance to note that serial and mean measurement of e-GFR is preferred to classify the patients into CKD stages appropriately. The authors recommend studying the effects of antidiabetic and anti-hypertensive medication on the deterioration of renal function, as well as evaluating the mortality rate, progression of ESRD and dialysis in the lower eGFR group. It is also recommended to take preventive measures by enhancing care for current cases and utilizing evidence-based best practices, such as providing the best screening, preventive and therapeutic modalities that prove to be beneficial in reducing and halting the progression of CKD. The authors also stress on the importance of avoiding assaults on kidney including NSAIDs and excessive PPI use to protect the kidneys
Conclusion
This study highlights the high prevalence of CKD of 16% among DM patients in Bahrain and is found to be higher among older patients and those with higher Hba1c levels and systolic blood pressure. This study is supported by a large number of sampled patients. Intensive screening and more aggressive treatment of DM patients is recommended for early detection of CKD. Furthermore, identifying the risk factors associated with CKD is crucial, particularly, the modifiable risk factors, in order to improve measures for its control and prevention.
Disclosure
Statement
There is no conflict of interest
Funding
No funding
Ethical consideration
The study was approved by Primary Health Care Research Committee of the Ministry of Health in Kingdom of Bahrain.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
authors have equally contributed to the development of the protocol, collection of data, data entry, data analysis and composition of the manuscript.