Volume 2, Issue 10
October 2022
Etiologies, Evaluation, and Differential Diagnosis of Dysphonia
Ashraf Abduljabbar, Theyab Alghamdi, Ohud Althagafi, Hatim Karhan, Aedah Alqrid, Abdullah Almalki, Abdullah Asiri, Mohammed AL Humaidan, Shamalah Rifdan, Saud Almahdaly, Hawra Alyaseen
DOI: http://dx.doi.org/10.52533/JOHS.2022.21005
Keywords: dysphonia, hoarseness of voice, epidemiology, etiology, differential diagnosis, evaluation, prognosis
Dysphonia is a common term that is usually used to describe abnormalities related to voice quality. The condition might also be referred to as hoarseness of voice. While dysphonia is usually used to describe impaired voice production, hoarseness of voice is used to describe altered voice quality. Laryngeal visualization and early identification of relevant signs and symptoms by the physician and patient are essential to achieving the best quality of care. However, diagnosis and evaluation of the condition are difficult due to challenges in laryngeal visualization and confusion caused by frequent laryngeal lesions. The present literature review extensively discusses the etiology, differential diagnosis, and evaluation of dysphonia. Different etiologies can attribute to this condition, including laryngeal and extra laryngeal disorders. Dysphonia does not usually persist for more than four weeks. However, when it persists beyond this, physicians should promptly evaluate the patient looking for a serious underlying disorder, most likely malignancy. Laryngeal visualization and obtaining a thorough history from the patient are the most recommended steps in evaluating a patient presenting with dysphonia. However, adequate care should also be paid to the development of evaluation-related complications that might further worsen the condition. The process should be evaluated and managed as early as possible to enhance the prognosis and survival rates, especially among patients suffering from laryngeal cancer. Increasing awareness among patients is also recommended to identify the problem and present it for evaluation as early as possible.
Introduction
Dysphonia is a common term that is usually used to describe abnormalities related to voice quality. The condition might also be referred to as hoarseness of voice. While dysphonia is usually used to describe impaired voice production, hoarseness of voice is used to describe altered voice quality (1). Dysphonia might be self-limiting in many patients. However, the condition might persist in many others, indicating the need to pay a visit to a healthcare physician for proper visualization and assessment of the larynx and vocal cords. This is usually indicated when the condition persists for more than four weeks (2-4). There are no physiological causes of dysphonia except during the aging process in teenagehood. Besides, the condition might be an indicator of a serious underlying illness that requires extensive management approaches. It can affect both children and adults. Early presentation and evaluation of the condition are recommended to exclude any potential of a serious underlying disease and enhance patient outcomes (1, 5, 6).
Various laryngeal and extra laryngeal etiologies have been reported to induce dysphonia, posing serious challenges in the evaluation and management process of the condition. Laryngeal visualization and early identification of relevant signs and symptoms by the physician and patient are essential to achieving the best quality of care. However, diagnosis and evaluation of the condition are difficult due to challenges in laryngeal visualization and confusion caused by frequent laryngeal lesions (7, 8). Reduced awareness among patients and mis-diagnostic practices are the main reasons that might lead to delayed diagnosis and management (3). In the present literature review, we aim to provide enhanced evidence regarding the etiology of dysphonia based on data from relevant studies in the literature. We will also discuss the differential diagnosis and evaluation practices for healthcare physicians to enhance the quality of care proposed for these patients.
Methods
The current study design is a narrative comprehensive literature review aiming at identifying and discussing articles that investigated the etiology, evaluation, and differential diagnosis of dysphonia in their populations. Accordingly, a comprehensive search was conducted on the databases, including Web of Science, GoogleScholar, PubMed, Embase, and Scopus, to identify all relevant articles. We used MeSh terms to formulate the search strategy. Moreover, our inclusion criteria included articles that investigated the etiologies, evaluation, and differential diagnosis of dysphonia, including observational studies and recruiting human subjects. Accordingly, studies that were not original did not include human individuals and did not report any of our reported outcomes regarding dysphonia in their populations were excluded.
Discussion
Etiology and epidemiology
Evidence shows that various causes and conditions can contribute to developing dysphonia, indicating the need to establish a differential diagnosis of these causes to enhance the quality of care. Vocal fold oscillations-related irregularities are the main theme in developing dysphonia pathophysiology. Such events might be attributed to various factors, including vocal cord tumor or lesion, changes in the bulk of the vocal fold, inadequate glottis closure during phonation, and hypertonicity, leading to irregular muscle tone (3, 9). Moreover, according to previous relevant investigations, it has been shown that voice overuse or misuse is a leading cause in this context and can typically lead to developing vocal fold nodules, which are commonly reported in this condition (10). Previous epidemiological data showed that smoking is the commonest risk factor for developing laryngeal cancer and premalignant lesions (11).
It should be noted that dysphonia is usually reported as the initial manifestation among patients suffering from neoplasms of the thyroid, lungs, pharynx, larynx, and lymphomas. Related nerve injuries might also lead to dysphonia from various conditions, including metastasis from lung or breast cancers. Moreover, it has been shown that the most common related malignancy is squamous cell carcinoma, with an estimated rate of 85-95% of the different vocal cord cancers (12, 13). Epithelial lesions in laryngeal squamous cell carcinoma usually led to the development of defective vibrations, which are usually involved in the pathogenesis of the condition. As cancer progresses, dysphonia worsens secondary to the involvement of thyroarytenoid muscle and vocal ligament. The cricoarytenoid unit might also be involved later, which can be clinically detected when the vocal fold becomes fixated or immobile (12).
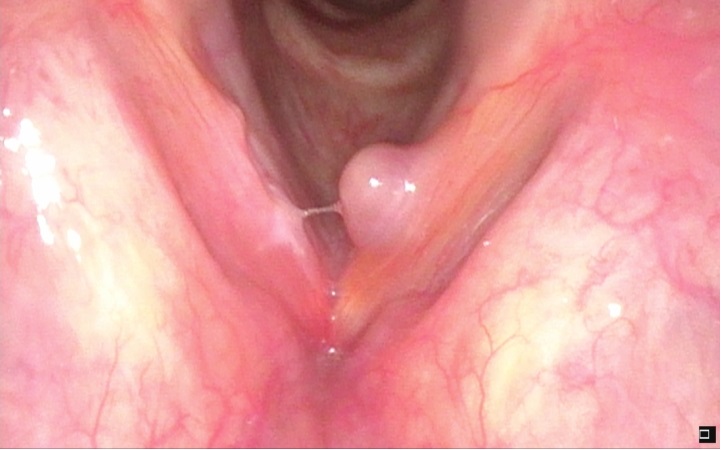
The most common cause of dysphonia has been reported to be infections, which might be acute or chronic, affecting the larynx. Voice abuse is also common among certain professions, like teachers, sports commentators, and singers (singer's nodules), leading to the development of lumps, polyps (Figure 1), papillomas, or cysts over the vocal cords that can interfere with their normal functions and speaking. Certain neurological conditions might also lead to dysphonia due to their impact on the nerves supporting the vocal cords. These conditions include Parkinson's disease, stroke, multiple sclerosis, and myasthenia gravis. Day-to-day stress was also previously reported as a psychological cause of developing dysphonia. Another cause might also be Reinke's edema impacting the larynx. Dysphonia has also been associated with certain endocrine disorders, like acromegaly and hypothyroidism. Permanent or temporary laryngeal nerve paralysis, a complication of thoracic and head and neck surgeries can also result in dysphonia. Gastroesophageal reflux disease is a common cause of developing dysphonia secondary to acid regurgitation into the larynx. Moreover, laryngeal scarring and, trauma, voice dysfunction might also result secondary to surgery on the vocal cords, major traumas affecting the thoracic and head and neck regions, laryngoscopy/bronchoscopy, and intubation. The long-term administration of corticosteroids might also lead to laryngeal irritation. Accordingly, a clinical evaluation should be thorough in these events to establish a proper diagnosis and enhance management outcomes (14, 15).
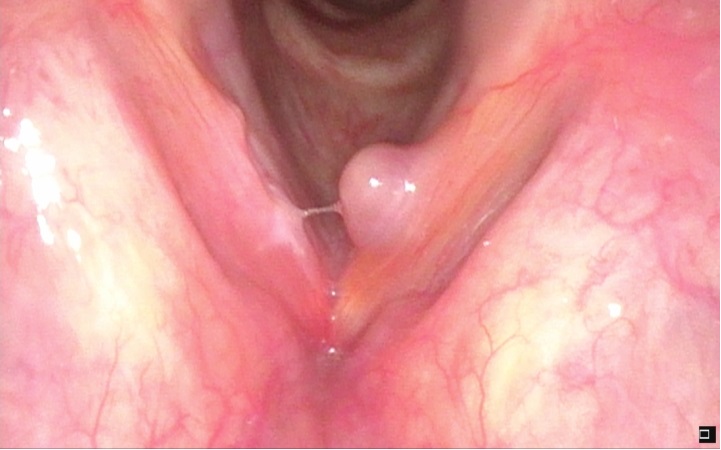
Figure 1: A vocal fold polyp in a patient with dysphonia
The development of dysphonia can occur in different gender and age population groups. Estimates indicate that the prevalence of the condition is up to 30% in the general population. However, it has been shown that certain populations might be at increased risk, including individuals with voice abuse/overuse, as previously mentioned (3, 9). Moreover, an estimated incidence of 7 in 100,000 of the general population has been reported for developing vocal fold malignancy (12).
Evaluation and differential diagnosis
As previously elaborated, different etiologies for developing dysphonia were reported in the literature. Figure 2 presents a summary of the differential diagnosis of dysphonia together with the commonest causes that should be considered by healthcare physicians when evaluating a presenting case (3, 16, 17). The first step in evaluating a patient presenting with dysphonia is by obtaining a thorough history from the patient and conducting needed examinations. Obtaining the history should include voice-related problems, including phonatory effort, loudness, pitch range, fatigability, voice quality, impaired singing voice, and conversational dyspnea. Moreover, physicians should also ask about similar previous conditions, received treatment modalities, previous related surgeries, voice habits, environmental factors, current medications, and the medical history of the patient (18). Identifying the most annoying factor is also recommended. Evidence among relevant studies in the literature indicates the validity of various questionnaires aiming at assessing voice problems, initial patient evaluation, and prognosis after conducting relevant treatment modalities. For instance, it has been demonstrated that glottic insufficiency can be significantly determined by the Glottal Function index (GFI), Voice-Related Quality of Life (VRQoL), and Voice Handicap Index (VHI) (18, 19). Moreover, assessing the emotional and functional parameters of voice-related problems can be significantly conducted by the Voice Handicap Index (VHI-10), which has been used in various surveys (20).
Laryngoscopy-based evaluation is also recommended for presenting patients to assess laryngeal functions and structure. The commonest instruments widely reported in this context include rigid endoscopes, flexible fiber optic laryngoscopes, and mirrors. Evaluation and recording of patient voice examination can be successfully conducted by rigid and flexible endoscopy during vocalization. Visualizing the vocal folds can be directly conducted using these instruments providing valuable assessment information that can help establish the diagnosis and draft the best management practice. Besides, evidence shows that these instruments can significantly view mucosal abnormalities, which can be difficult to obtain via magnetic resonance imaging or computed tomography (4). In this context, it has been recommended that routine evaluation should not include radiographic imaging, particularly prior to endoscopic assessment. Visualizing the vocal fold's mucosal oscillation in slow motion can be done by pulsed light of the video laryngoscope, which is synchronized with the vocal frequency of the patient. This can remarkably provide assistive knowledge regarding mucosal pliability. Therefore, it is considered the most diagnostic instrument in evaluating dysphonia.
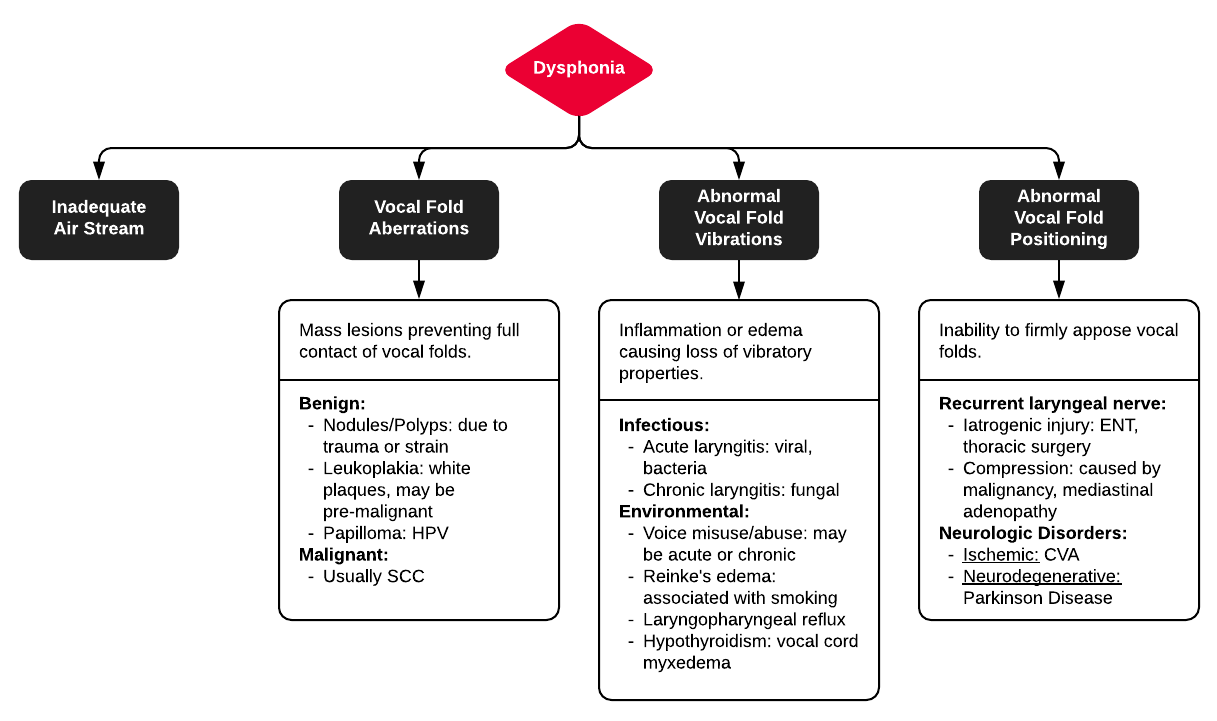
Figure 2: Differential diagnosis of dysphonia
Laryngoscopy-based evaluation is also recommended for presenting patients to assess laryngeal functions and structure. The commonest instruments widely reported in this context include rigid endoscopes, flexible fiber optic laryngoscopes, and mirrors. Evaluation and recording of patient voice examination can be successfully conducted by rigid and flexible endoscopy during vocalization. Visualizing the vocal folds can be directly conducted using these instruments providing valuable assessment information that can help establish the diagnosis and draft the best management practice. Besides, evidence shows that these instruments can significantly view mucosal abnormalities, which can be difficult to obtain via magnetic resonance imaging or computed tomography (4). In this context, it has been recommended that routine evaluation should not include radiographic imaging, particularly prior to endoscopic assessment. Visualizing the vocal fold's mucosal oscillation in slow motion can be done by pulsed light of the video laryngoscope, which is synchronized with the vocal frequency of the patient. This can remarkably provide assistive knowledge regarding mucosal pliability. Therefore, it is considered the most diagnostic instrument in evaluating dysphonia.
Furthermore, using stroboscopy can be significantly used to obtain and visualize various components of the glottic cycle, including the patterns of partial versus complete and incomplete closures and the symmetry of vocal folds in both the vertical and lateral folds, mucosal waveform, regularity of glottic cycle (uniformity). This approach can be remarkably useful in the evaluation process since some details cannot be obtained by rigid or flexible endoscopic approaches. Stroboscopy-based surveillance might also be useful in evaluating patients suffering from related malignancies (21, 22).
On physical examination, the only abnormal finding might be hoarseness of voice. An informal and formal evaluation of the patient's voice should be approached while the patient is conversing with the physician. This can significantly enable the physician to assess different voice aspects, including articulation, prosody, loudness, nasality, pitch, and quality. Physicians should also observe whether wet voice, diplophonia (two spontaneous simultaneously-perceived pitches), glottic fry, tremors, and aphonia are present. Some signs and symptoms might be associated with dysphonia and indicate the presence of laryngeal carcinoma, including dysphagia, aspiration, and weight loss. Otalgia and dyspnea might also be other manifestations in advanced stages of laryngeal cancer. Physicians should also ask about other signs of malignancy, including hemoptysis and cough. Obtaining a history of gastroesophageal reflux disease, like heartburn and discomfort, should also be sought. Asking about history should also include a family history of neck and head cancer, neck radiation, alcohol use, and smoking (12, 23). Besides, physicians should be aware that some symptoms, like cognitive delays, gait abnormalities, extremity and hand tremors, tongue deviation or tremor, and dysphagia, are suggestive of a neurological etiology of dysphonia (24, 25).
Furthermore, different auditory-perceptual assessment tools have been proposed in the literature to evaluate the patient's voice. Among the different scales, the CAPE-V and the GRBAS are the two most commonly used scales. The gold standard for assessment of voice perception is the GRBAS scale. Moreover, it can remarkably evaluate different components, like strain (excessive effort), asthenia (weakness), breathiness (air escape), roughness (irregularity), and degree (grade of voice dysfunction). The severity of the condition can be stratified by this tool according to a 4-point scale, as 3 indicates a severe disease while 0 indicates a normal condition (18). Physicians should also conduct a thorough head and neck examination, together with the auditory-perceptual assessment. They should observe the breathing habits of the patient and whether there are any breath-holding patterns (18).
Various treatment and evaluation-associated complications might be developed and should also be considered by healthcare physicians. For instance, some complications like edema, postoperative hematoma, bleeding, and hemorrhage might develop and complicate the ability to visualize the vocal folds, making the assessment process more difficult. Moreover, vocal fold injections during evaluation and assessment are less common and are usually observed in < 5% of this population (26). These complications might include aspiration and airway compromise. Other surgery-related complications might also include infections, need for re-surgery, failure to obtain proper medialization, implant extrusion or migration, and the increased risk of tracheostomy (27). It is important to stratify the prognosis of dysphonia and evaluate the efficacy of the proposed management modalities. It should be noted that the prognosis of these patients is remarkably variable and significantly depends on the underlying etiology and whether other comorbidities are associated. Accordingly, the prognosis can range from excellent to poor among the affected patients. For instance, the prognosis is usually good for patients with dysphonia secondary to acute laryngitis, as these patients usually recover within 1-3 weeks after proper symptomatic treatment. On the other hand, extensive management modalities, like excessive speech therapy and rest sessions, are usually needed among patients who developed dysphonia secondary to vocal fold polyps/nodules, muscle tension-induced dysphonia, and following functional dysphonia. The prognosis and survival rates of patients with laryngeal cancer are significantly variable and depend on the severity and stage of the disease. For instance, reports estimated a 5-year survival rate of 30-63% for patients suffering from late stages. On the other hand, the estimated 5-year survival rate is significantly higher among patients presenting with early-stage disease. Metastasis is the most commonly reported cause of death among these patients. Therefore, these rates indicate the importance of early identification and management of laryngeal cancer, which can be early identified by dysphonia, the earliest disease symptom, as previously mentioned (12, 13, 23).
Conclusion
Different etiologies can attribute to this condition, including laryngeal and extra laryngeal disorders. Dysphonia does not usually persist for more than four weeks. However, when it persists beyond this, physicians should promptly evaluate the patient looking for a serious underlying disorder, most likely malignancy. Laryngeal visualization and obtaining a thorough history from the patient are the most recommended steps in evaluating a patient presenting with dysphonia. However, adequate care should also be paid to the development of evaluation-related complications that might further worsen the condition. Increasing awareness among patients is also recommended to identify the problem and present it for evaluation as early as possible.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.