Volume 2, Issue 10
October 2022
Retinopathies: Types, Etiologies, and Outcome
Ahmed Alnahdi, Anwar Alghamdi, Khaled Alkandari, Abdulrhman Alsamir, Abdulrahman Alsomali, Taghreed Al Mani, Majed Albogami, Haitham AlOraini, Mohammed Alqahtani, Riham Altalab, Noura Alzubidi
DOI: http://dx.doi.org/10.52533/JOHS.2022.21003
Keywords: retinopathy, loss of vision, diabetic retinopathy, proliferative, non-proliferative, hypertensive retinopathy
Retinopathy is a broad term that involves damages occurring to the retina. The disease is a serious one, being a significant risk factor for blindness. It might also refer to abnormal blood flow-induced retinal damage or retinal vascular disease. Disturbances in the retinal blood flow can remarkably lead to ischemia and damage to the retina. Moreover, the accumulation of exudates (causing macular edema) and bleeding might cover the photoreceptors on the retina, leading to visual impairment. In the present literature review, we have provided updated evidence regarding the types and causes, and outcomes of retinopathy. Accordingly, a comprehensive search was conducted on the databases, including Web of Science, Google Scholar, PubMed, Embase, and Scopus, to identify all relevant articles. Estimates show that retinopathy is highly prevalent among individuals with systemic disorders like diabetes and hypertension. Diabetic and hypertensive retinopathies are the commonest causes of retinopathy. Retinopathy of prematurity is another cause affecting neonates. However, the condition is usually self-limited with no interventions, although highly prevalent in around 40% of newborns. There are two main types of retinopathies, including non-proliferative and proliferative types. Both types can occur as complications of diabetes mellitus, indicating the need to enhance the management of this population and improve the quality of care. Hypertension and poor glycemic control can remarkably determine the outcomes of the disease, implying the need to apply proper health interventions. Neonates with severe retinopathy of prematurity might suffer from severe outcomes, including loss of vision, glaucomas, and cataracts.
Introduction
Retinopathy is a broad term that involves damages occurring to the retina. The disease is a serious one, being a significant risk factor for blindness. It might also refer to abnormal blood flow-induced retinal damage or retinal vascular disease. Disturbances in the retinal blood flow can remarkably lead to ischemia and damage to the retina (1). Moreover, the accumulation of exudates, causing macular edema and bleeding might cover the photoreceptors on the retina which can lead to visual impairment. Different causes for retinopathy have been proposed in the literature, mostly including systemic diseases involving the pathologies mentioned above (2).
Some reports also consider age-related retinal macular degeneration a subtype of retinopathy (3). However, other authors consider it a different entity having other characteristics. There are two major types of retinal vascular disease or retinopathies, including non-proliferative and proliferative types. Evidence from different studies shows that retinopathy is not usually detected as a sole condition (2, 4). On the other hand, it is usually detected in individuals with chronic conditions, like hypertension and diabetes, as a consequence or a complication of these disorders (5). Epidemiological data from the United States in 2008 show that the commonest cause of retinopathy across the country is diabetes (6). Evidence of studies conducted among working-age individuals further shows that diabetic retinopathies are the commonest causes of blindness among them (6). Therefore, the World Health Organization stratifies the condition as a priority eye disease, being responsible for around 5% of blindness globally (6, 7).
In the present study, we will discuss the different types and etiologies of diabetic retinopathy based on evidence from different studies in the literature. We will also discuss the outcomes and prognosis of each type which might help healthcare authorities take more care of the most vulnerable groups.
Epidemiology
Retinopathy is highly prevalent worldwide, particularly among patients with chronic conditions like diabetes and hypertension (8). Moreover, according to previous investigations that are based on worldwide data, around 50,000 premature infants suffer from retinopathy of prematurity, and around 5 million individuals suffer from diabetic retinopathy (7, 9). Another large-scale investigation conducted in the United States and Canada shows that some degree of retinopathy of prematurity is prevalent in around 40% of premature infants (10). However, it has been shown that no treatment is usually required for these cases since the condition is self-limited. Another investigation also demonstrated that the prevalence of hypertensive retinopathy among non-diabetic adult’s ranges between 3-14% and constitutes the second most common cause of retinopathy (11, 12). Estimates furtherly indicate that among patients with hypertension, retinopathy is prevalent in around two-thirds of them. Different risk factors, including systolic blood pressure, age, and duration of hypertension, are all risk factors for developing the condition in this population.
Types and etiologies
The pathophysiology of retinopathy can be broadly divided into two main types, including proliferative and non-proliferative types. The pathophysiology of developing retinopathy by these types includes a variety of pathways and mechanisms, which mainly impairs the retinal blood flow. The central retinal artery is the main branch supporting the retina by small vessels. Abnormal growth of the retinal blood vessels leads to the development of the proliferative type. It should be noted that the formation of new blood vessels, referred to as angiogenesis, naturally occurs as a part of tissue formation and growth (4, 13, 14). However, neovascularization is the term used to describe an abnormal rate of angiogenesis since abnormal blood vessels grow within the tissues. On the other hand, the pathophysiology of the non-proliferative type is mainly due to compromised or damaged blood vessels secondary to various reasons that will be discussed later.
Proliferative retinopathy
The neovascularization process in the neuroproliferative group leads to developing weak, fragile, and non-competent blood vessels that cannot adequately deliver blood to the retinal tissues. Besides, these vessels, being vulnerable and fragile, cause protein, fluid, and other debris to leak into the surrounding tissues. Moreover, it has been shown that there is an increased risk of bleeding secondary to reduced strength of the newly formed vessels (Figure 1). Blindness and vision loss might result secondary to these events since hemorrhage might interpret the normal retinal functions, making proliferative retinopathy a high-risk disease. Other causes of proliferative retinopathy are also involved in the non-proliferative type. It has been shown that the non-proliferative type might significantly result as a later consequence of neovascularization and angiogenesis. Furthermore, direct retinal damage and tissue ischemia might develop secondary to various causes of non-proliferative retinopathy. In the ischemic/damaged tissues, increasing the blood flow is usually observed as the body tries to compensate for these events (15-18).
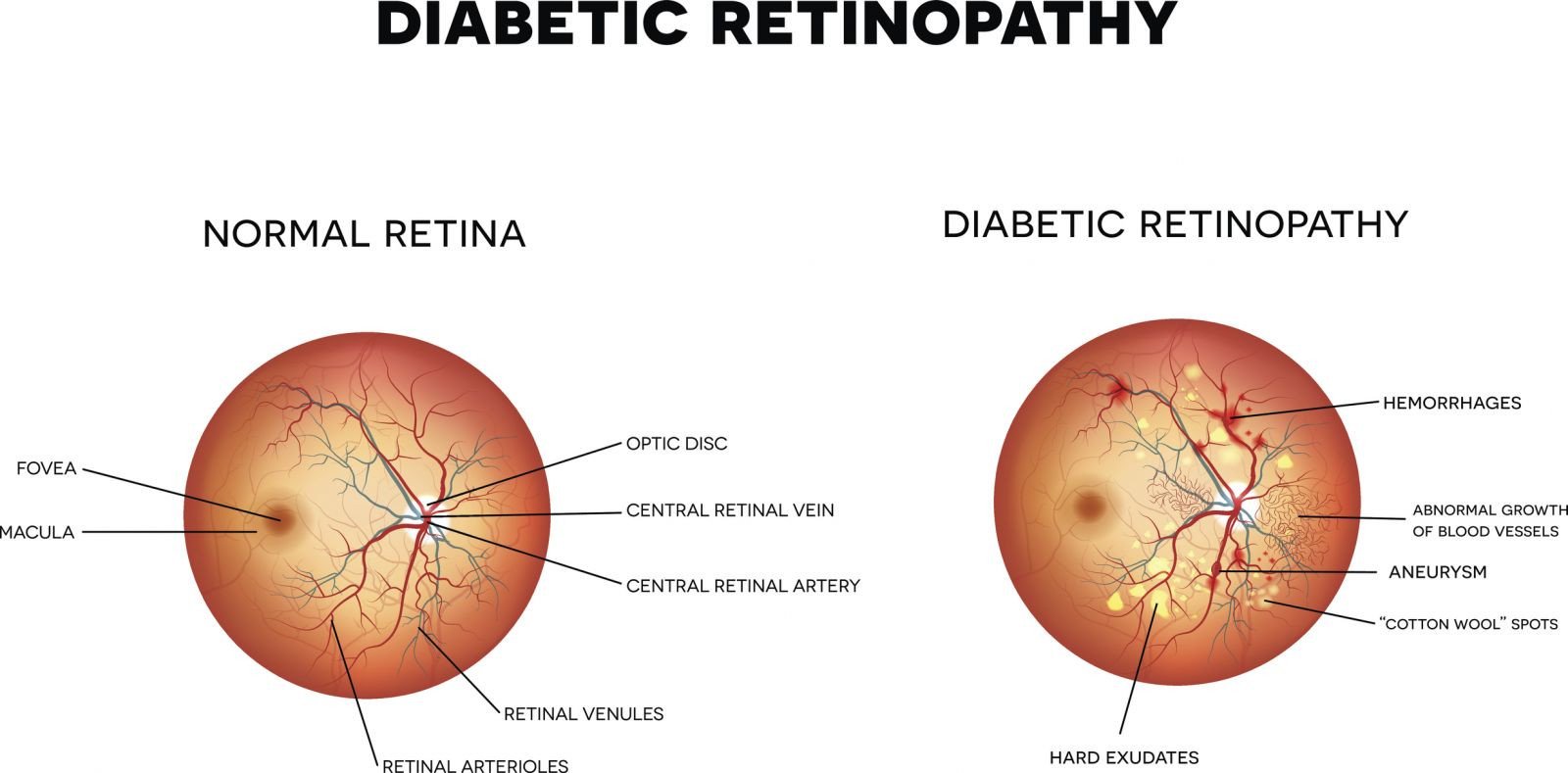
Figure 1: A comparison of a normal retina and another with diabetic retinopathy (proliferative type).
Non-proliferative retinopathy
It has been demonstrated that various causes can remarkably lead to developing non-proliferative retinopathy. Some factors include anemia (like anemia due to vitamin B12 deficiency), sickle cell disease, radiation, and hypertension (19). Other causes might also include diabetic retinopathy, solar retinopathy, and retinopathy of prematurity. There are different mechanisms by which these etiologies result in developing non-proliferative retinopathy. These include blood vessel occlusion, direct retinal damage, and damage or remodeling of the retinal blood vessels. Retinal blood vessel occlusion might result from a significant narrowing of these blood vessels or directly blocking them, making them unable to deliver sufficient blood and nutrients to the target tissues, resulting in tissue ischemia and damage (20). A compelling example of this is sickle cell disease, which induces the blood flowing through the retinal arteries to thicken or sludge, reducing its flow rate (21). Blood sludging events are also observed in other hyperviscosity syndromes, leading to compromised blood flow to the retina. Retinal cell ischemia might also result from central artery clots or thrombosis. Altering the blood supply by retinal vessels is also reported as a common mechanism for inducing non-proliferative retinopathy. This is mainly apparent in cases of hypertension since increased blood pressure significantly results in the thickening of the walls of the blood vessels, which reduces the amount of delivered blood to the retina (1, 13). This is also significant in cases of atherosclerosis, which induces significant narrowing and hardening of the blood vessels, cumulatively leading to ischemia and tissue damage. Free-radical induced direct retinal damage is another common mechanism that results from oxidative stress, apparent in retinopathy of prematurity, solar, and radiation retinopathies (22).
Diabetic retinopathy
Evidence from various investigations in the literature shows that the commonest cause of proliferative retinopathy is Diabetes Mellitus (DM), causing diabetic retinopathy. Moreover, estimates show that the commonest cause of blindness and loss of vision among adults is diabetic retinopathy. DM-related hypertension and poor glycemic control are the most contributing factors to developing diabetic retinopathy. It can occur in two types: proliferative (secondary to neovascularization), which occurs at an advanced stage of DM, and non-proliferative (secondary to microaneurysms formation). Impairment of vision might result from the non-proliferative type secondary to macular edema resulting from blood and fluid leakage into the retina. On the other hand, impaired vision might result from the light block from the retinal photoreceptors secondary to vitreous hemorrhage (23).
Hypertensive retinopathy
This type is also considered one of the most important conditions since its role in the pathogenesis and development of subsequent conditions, including vision impairment. Epidemiological data estimate that around 33% of the United States suffer from chronic hypertension (24). Moreover, the disease is a significant risk factor for developing severe cardiovascular and cerebral disorders. Evidence shows that hypertensive retinopathy might remarkably result from chronic and acute episodes of increased blood pressure. Chronic hypertension can significantly increase the vascular tone (leading to constricted retinal vasculature), which can subsequently induce significant damage to the underlying vascular endothelium. Accordingly, sclerotic hypertensive retinopathy can result from these events.
Retinopathy of prematurity
Estimates from worldwide data also indicate that this type of retinopathy is a leading cause of vision impairment and loss. The affected population includes extremely low and low-birthweight and premature infants. Moreover, the condition has also been reported among full-term infants. However, such events are rare (25). Oxidative stress is the main pathology involved in developing retinopathy of prematurity in neonates. The disease is a significant indicator of receiving supplemental oxygen therapy (26, 27). Hypoxia in neonates significantly flares the release of vascular endothelial growth factors, which have a significant role in developing angiogenesis-related retinopathies. Accordingly, oxygen supplementation for these infants can significantly reduce the frequency of circulating vascular endothelial growth factors and induce a state of hyperoxia. However, it has been shown that it might also lead to endothelial cell death and abnormal vasculature growth (28). Neovascularization will subsequently result from these events secondary to increased growth factors and vasculature closure (26).
Macular damage might occur secondary to various events leading to central vision loss among patients suffering from age-related macular degeneration. The condition might be atrophic (dry) or exudative (wet), while the first one accounts for most of the cases (80-90%). On the other hand, most cases with severe vision loss (90%) are attributed to the exudative type, although its prevalence is very low compared to the dry type (29). Lipofuscin, oxidized lipid pigments, correlates with age-related macular degeneration by accumulating intracellularly within the retinal pigment epithelium (30). The pathogenesis of age-related macular degeneration is controversial and being investigated. However, it has been suggested that lipofuscin accumulation might have a significant role in this context. Another risk factor that might be involved in developing age-related macular degeneration is the extracellular accumulation of drusen between Bruch’s membrane and retinal pigment epithelium (31). The current area of research lacks cohesion, and further studies are still warranted in the future to provide better evidence.
Outcomes and prognosis
The prognosis of retinopathy remarkably depends on the cause of the condition, its prognosis, and how much it is involved in the pathogenesis of retinopathy. For instance, some reports indicate that retinopathy of prematurity usually enhances over time as the condition is self-limited. The pathology that was originally observed (formation and development of abnormal vessels) begin to disappear, which is also aided by providing appropriate treatment circumstances. However, it should be noted that the condition can be severe in some cases, leading to blindness if not properly managed. Furthermore, these children reported some complications, including near-sightedness, lazy eyes, crossed eyes, glaucomas, cataracts, and retinal detachment (32-34). Furthermore, the prognosis in cases with serious central retinopathy is usually favourable since it has been evidenced that most cases return to normal within 3-4 months. Besides, it has been shown that full visual acuity can be fully reserved within six months from the disease onset. On the other hand, some patients might suffer from permanent symptoms, like difficulty with night vision, reduced contrast sensitivity, and distortion. In cases when the disease is severe or resistant, photodynamic or laser therapy can be effectively used to enhance treatment outcomes. Photodynamic therapy increases the sensitivity of certain cells to light by exposing them to certain chemicals and light. However, it should be furtherly noted that some estimates reported that around half of patients with central serous retinopathies develop recurrent disease.
Regarding diabetic retinopathy, evidence shows that the prognosis significantly depends on various factors regarding the disease. For instance, it has been reported that the prognosis depends on the degree of glycemic and blood pressure control, close monitoring of the condition, and controlling the disease with no evidence of complications. Compliance with adequate treatment regimens might enhance the condition and reduce the risk and severity of retinopathy. On the other hand, poor disease control might worsen the condition, leading to blindness in severe cases. Regarding hypertensive retinopathy, it has been evidenced that adequate control of the patient’s blood pressure can remarkably enhance the condition and reduce the severity of the disease. However, some damage-related manifestations might be permanent even with adequate treatment (6, 35-37).
Conclusion
Estimates show that retinopathy is highly prevalent among individuals with systemic disorders like diabetes and hypertension. Diabetic and hypertensive retinopathies are the commonest causes of retinopathy. Retinopathy of prematurity is another cause affecting neonates. However, the condition is usually self-limited with no interventions, although highly prevalent in around 40% of newborns. Hypertension and poor glycemic control can remarkably determine the outcomes of the disease, implying the need to apply proper health interventions. Neonates with severe retinopathy of prematurity might suffer from severe outcomes, including loss of vision, glaucomas, and cataracts.
Disclosure
Statement
The authors declare no conflict of interest.
Funding
No funding.
Ethical consideration
Non-applicable.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Authors’ contribution
All authors contributed equally to the drafting, writing, sourcing, article screening and final proofreading of the manuscript.
