Volume 2, Issue 10
October 2022
Knowledge, and Practice Related to Oral Leukoplakia Among Dental and Medical Professionals in Riyadh, Saudi Arabia
Hamad Albagieh, Atheer Almughaiseeb, Majid Asrar, Sara AlGhannam, Sara Alduraibi, Afnan Almughaiseeb
DOI: http://dx.doi.org/10.52533/JOHS.2022.21001
Keywords: leukoplakia, knowledge, practice, physician, dental
Background: Leukoplakia is a major oral potentially malignant disorder. Nonhomogeneous leukoplakia has a greater chance of developing into cancer. Leukoplakia must therefore be identified early via an oral (visual) examination by dentists and family doctors in order to maximize the chances of survival by prompt referral and early treatment. The purpose of this study was to comprehend the knowledge and practices of dentists and physicians about leukoplakia.
Methodology: This research was an observational analytic study using a cross-sectional design. The study included interns, general practitioners, residents, specialists, and consultants in the dental field, as well as family medicine physicians and otolaryngologists in Riyadh, Saudi Arabia, excluding oral medicine dentists and medical professionals. Data was collected via a questionnaire survey conducted using Google Forms. Recruitment was done by going to several private and governmental health institutes and distributing the survey link or filling it out through a data collector.
Results: A total of 260 dental and physicians participated in this survey. Of these, 147 (56.5%) were males and 113 (43.5%) were females. Knowledge scores were significantly higher in dental respondents than in physicians (p<0.001). The mean knowledge scores significantly differed across the levels, such as consultants, specialists, residents, general practitioners, and interns (P<0.001). Physicians (65.7%) were more likely to screen tobacco-using patients than dentists (31.6%). A greater percentage of dentists than physicians (77.1% vs 67.1%) respondents describe the risks associated with cigarette smoking.
Conclusion: From this study, it may be concluded that most of the dental professionals in Riyadh, Saudi Arabia have higher theoretical levels of knowledge about leukoplakia than family medicine physicians and otolaryngologists. The study also showed that there is a significant difference between the knowledge scores across various levels of dental and medical professionals regarding the knowledge scores. The current investigation finds that dentists are less experienced in dealing with leukoplakia cases but have good theoretical knowledge of them.
Introduction
Leukoplakia is a white patch or plaque that develops in the oral cavity (1). Oral leukoplakia (OL) is the most common potentially malignant disorder of the oral mucosa (2). It is usually asymptomatic and is more prevalent in males over the age of 40. However, the prevalence below the age of 30 is 1% and increases to reach 2% in males and 8% in females over the age of 70 (3). Leukoplakia is classified into early, homogenous, verruciform, and erythroleukoplakia. Each subdivision has a different malignant transformation potential. For instance, proliferative verrucous leukoplakia (PVL) carries the highest malignant transformation. It is found that 63.3% and 100% of PVL cases transform into Squamous Cell Carcinoma (SCC) (3). It is only when other white lesions such as oral lichen planus, white sponge nevus, nicotine stomatitis, and leukoedema are excluded that, the clinical diagnosis of OL can be made. Otherwise, the only confirmatory way of diagnosis is histologically (2).
The global prevalence of OL is between 0.2% and 3.6%, with different geographical variations. In India, it is between 0.2 and 4.9%, while in Sweden it is found to be around 3.6%, Germany 1.6%, and the Netherlands 1.4% (4). A recent study in Jedda, Saudi Arabia, found that OL was the second-most common possibly malignant lesion (2.3%) (5). A higher prevalence rate (3.17%) has been observed among tobacco smokers in Aljouf province in a 2017 study by Aljabb et al. with OL resulting as the most seen potentially malignant lesion (6).
Oral leukoplakia is associated with multiple risk factors. Smoking tobacco, regardless of its form was found to be the chief causative factor for OL (4). The number of smokers is increasing as the global population continues to grow, and Saudi Arabia has a well-established tobacco epidemic. (5). There’s a strong and well-reported correlation between smoking tobacco and malignancies of the oral cavity (7). Therefore, a lack of knowledge, attitude, and practice between dental and medical professionals will affect the prevention, diagnosis, and early intervention. The literature that measures the awareness and knowledge of OL is limited among health care professionals. Based on Eltelety et al. have reviewed the knowledge, attitude, and practice regarding oral cancer among dentists in Jeddah, Saudi Arabia. From the study, 27.5% identified both erythroplakia and leukoplakia as conditions that are most likely associated with oral cancer (8). On the other hand, Kujan et al. conducted a cross-sectional study on 550 Saudi dental undergraduates. The study has shown that 43% believed that it wasn’t part of their role to help patients to stop smoking or help in preventing smoking in the first place (9). Furthermore, a study in Jordan revealed an insufficient level of knowledge of oral cancer and that dentists significantly have more awareness of oral cancer than medical graduates (10). We aim to evaluate the knowledge, and practice of OL among dental and medical professionals in Riyadh, Saudi Arabia.
Methodology
This is a cross-sectional survey study that was conducted between July 2019 and January 2020. The study included interns, general practitioners, residents, specialists, and consultants in the dental field, as well as family medicine physicians and otolaryngologists in Riyadh, Saudi Arabia, in both governmental and private sectors. We excluded oral medicine dentists and medica. Recruitment was done by going to several private and governmental health institutes and distributing the survey link or by filling it out through a data collector. A random sampling technique was applied. Furthermore, the survey was sent online through WhatsApp using Survey Monkey to healthcare practitioners. The questionnaire was divided into two sections to assess knowledge, and practice related to OL among dental and medical professionals in Riyadh, Saudi Arabia. This study was approved by the King Saud University College of Dentistry Institutional Ethical Review Board with approval Numbers: 18-3385.
statistical analysis
The survey was tested for validity and reliability using the Cronbach Alpha of > 0.70. Afterward, experts in the field were asked to assess any changes to the survey. The data was collected and analysed using IBM SPSS version 22. A chi-square test was applied to categorical questionnaire variables. Mean knowledge scores were compared using an independent sample t-test and ANOVA with post hoc analysis. A p-value of <0.05 was considered statistically significant.
Results
Of the 260 respondents, 147 (56.5%) were males and 113 (43.5%) were females. One hundred and ninety patients had a dental degree, and the remaining seventy respondents had a medical degree. Regarding the rank, the majority of the respondents were interns (39.2%), followed by residents (17.3%), consultants (15.8%), specialists (13.8%), and general practitioners (13.8%), respectively. The majority were working in the government sector (75%), 13.5% were working in the private sector, and 11.0% were working in both the private and government sector (11.5%) (Table 1).
|
Table 1: Baseline characteristics of the participants |
|
|
Characteristics |
No. (%) |
|
Gender |
|
|
Male |
147 (56.5%) |
|
Female |
113 (43.5%) |
|
Specialty |
|
|
Dentists |
190 (73.1%) |
|
Physicians |
70 (26.9%) |
|
Rank |
|
|
Consultant |
41(15.8%) |
|
Specialist |
36 (13.8%) |
|
Resident |
45 (17.3%) |
|
General practitioner |
36 (13.8%) |
|
Intern |
102 (39.2%) |
|
Sector |
|
|
Government |
195 (75.0%) |
|
Private |
35 (13.5%) |
|
Government and private |
30 (11.5%) |
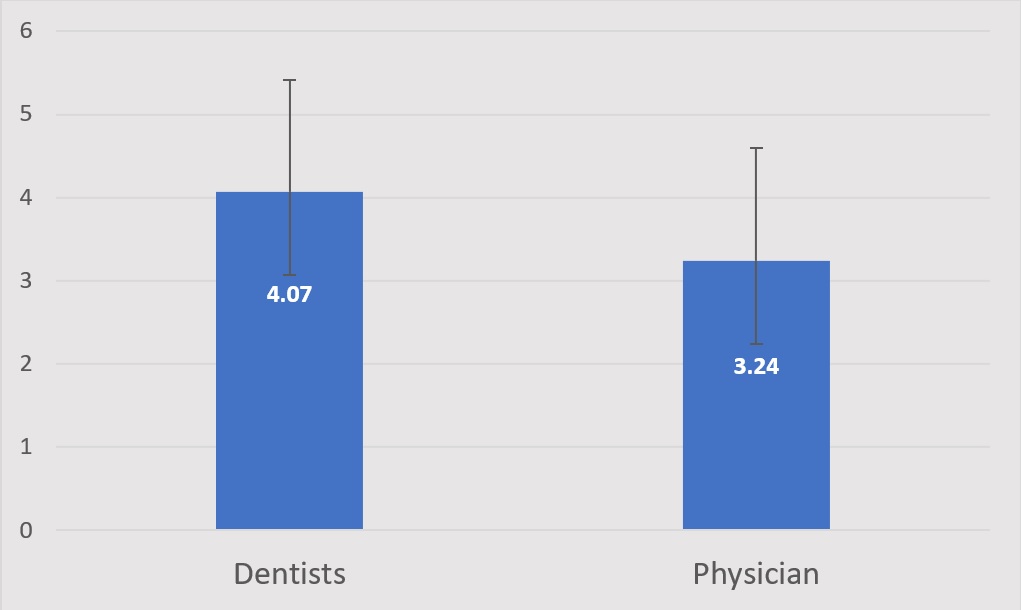
Table 2 shows the distribution of results regarding the knowledge questions on the questionnaire. The majority of dentists and physicians were familiar with the oral potentially malignant disorder, with 75.8% of dentists and 72.9 percent of physicians. The majority of the respondents were able to identify leukoplakia as the most common potentially malignant disorder in the oral cavity. Regarding the causative factor of PL, 70% of physicians correctly identified tobacco, while 62.1% of dentists identified tobacco and 11% identified alcohol as the causative factor. Dentists were more likely to identify the causative factor than physicians (p < 0.001). The respondent’s knowledge concerning the diagnostic feature of oral cancer was assessed through the question with choices of whether the scrapable lesion (can be removed), the white non scrapable lesion (cannot be removed), and the white lesion disappear when scratched. Most of the dental (57.9%) and physician (70.1%) respondents answered that white non scrapable lesions are a major diagnostic feature. The majority of the physicians knew that buccal mucosa (85.7%) was the most common site of OL. According to most dentists, the tongue (56.8%) was the most common site of OL. Fifty-six dentists (29.5%) and twenty-two physicians (31.4%) correctly identified that proliferative verrucous leukoplakia has the highest malignant transformation. Figure 1 shows the distribution of knowledge scores among dentists and physicians. There was a statistically significant difference observed between the mean knowledge score among the dentists and physicians (p <0.001). The dentist was found to have higher knowledge scores compared with physicians (Table 2).

Figure 1: Mean score distribution of Dentists and Physicians
|
Table 2: Respondents’ answers to the survey concerning the knowledge of oral leukoplakia (n= 260) |
||||
|
Question |
Response |
Specialty |
p-value |
|
|
Dentists |
Physician |
|||
|
Familiarity with the potential malignant disorder (precancerous lesions) |
Yes |
144 (75.8) |
51 (72.9) |
0.628 |
|
No |
46 (24.2) |
19 (27.1) |
||
|
Most common potentially malignant disorder in the oral cavity |
Leukoplakia |
144 (75.8) |
49 (70) |
0.621 |
|
Candida |
6 (3.2) |
2 (2.9) |
||
|
Oral submucous fibrosis |
2 (1.1) |
2 (2.9) |
||
|
I don’t know |
38 (20) |
17 (24.3) |
||
|
The main causative factor of oral leukoplakia is? |
Tobacco |
118 (62.1) |
49 (70) |
<0.001* |
|
Genetic |
8 (4.2) |
0 |
||
|
Alcohol |
22 (11.6) |
0 |
||
|
I don’t know |
42 (15.8) |
21 (30) |
||
|
The most important diagnostic feature of oral leukoplakia is? |
White scrapable lesion (can be removed) |
14 (7.4) |
5 (7.1) |
0.013* |
|
White non-scrapable lesion (cannot be removed) |
110 (57.9) |
54 (77.1) |
||
|
The white lesion disappears when scratched |
20 (10.5) |
6 (8.6) |
||
|
I don’t know |
46 (24.2) |
5 (7.1) |
||
|
The most common site of oral leukoplakia is? |
Buccal mucosa |
44 (23.2) |
60 (85.7) |
<0.001* |
|
Palate |
10 (5.3) |
0 (0%) |
||
|
Tongue |
108 (56.8) |
6 (8.6) |
||
|
I don’t know |
28 (14.7) |
4 (5.7) |
||
|
What type of oral leukoplakia has the highest malignant transformation? |
Proliferative verrucous leukoplakia |
56 (29.5) |
22 (31.4) |
0.101 |
|
Erythroplakia |
40 (21.1) |
19 (27.1) |
||
|
Candida leukoplakia |
8 (4.2) |
7(10) |
||
|
I don’t know |
86 (45.3) |
22 (31.4) |
||
|
Knowledge Score |
4.07 ± 1.34 |
3.24 ± 1.36 |
<0.001* |
|
* P-value <0.05 is statistically significant
Our study found that physicians (65.7%) were more likely to screen tobacco-using patients than dentists (31.6%). The majority of the respondents among the dentist (77.9%) explains the risk factors for the use of tobacco which was higher than physicians (67.1%). However, physicians were more likely to screen patients affected by leukoplakia (Table 3).
|
Table 3: Respondents’ practice-related items (n=260) |
||||
|
Items related to the practice |
Response |
Specialty |
p-value |
|
|
Dentists |
Physician |
|||
|
Do you adequately screen a patient who is using tobacco? |
Yes |
60 (31.6) |
46 (65.7) |
<0.001* |
|
No |
130 (68.4) |
24 (34.3) |
||
|
Do you explain the risk factors of tobacco use to the patient? |
Yes |
148 (77.9) |
47 (67.1) |
0.076 |
|
No |
42 (22.1) |
23 (32.9) |
||
|
Have you ever screened patients affected with leukoplakia? |
Yes |
27 (14.2) |
26 (37.1) |
<0.001* |
|
No |
163 (85.8) |
44 (62.9) |
||
|
To which specialty you will refer the patient who is affected with leukoplakia? |
Maxillofacial department |
68 (35.8) |
4 (5.7) |
<0.001* |
|
Oral medicine department |
80 (42.1) |
66 (94.3) |
||
|
Oral radiology department |
2 (1.1) |
0 (0%) |
||
|
I don’t know |
40 (21.1) |
0 (0%) |
||
|
Do you inform the patient to report any abnormal change in the oral cavity? |
Yes |
116 (61.1) |
57 (81.4) |
0.002* |
|
No |
74 (38.9) |
13 (18.6) |
||
* P-value <0.05 is statistically significant
Table 4 demonstrates the mean scores among different levels of respondents. The mean knowledge scores significantly differed across the levels, such as consultants, specialists, residents, general practitioners, and interns (P<0.001) (Figure 2). Consultants and specialists were found to have significantly higher knowledge than others. It has been observed that interns have significantly lower knowledge than others. There was no statistical difference between residents and general practitioners, as well as between consultants and specialists.
|
Table 4: Distribution of knowledge scores among respondents at various levels |
||
|
Mean ± SD |
p-value |
|
|
Consultant |
4.24 ± 1.30 |
<0.001* |
|
Specialist |
4.22 ± 0.92 |
|
|
Resident |
3.27 ± 1.25 |
|
|
General practitioner |
3.5 ± 1.63 |
|
|
Intern |
2.56 ± 1.30 |
|
* P-value <0.05 is statistically significant

Figure 2: Mean score distribution of respondents at the various expertise levels
Discussion
Among the potentially malignant disorders of the mouth the majority is leukoplakia. Understanding the main contributing causes of OL and its accompanying problems is essential for both early detection and prevention of the condition because, once it appears, it will affect patients’ quality of life and their survival rates (11). Oral cancer researchers concur that early detection considerably improves the likelihood of cure and the survival rate with the least amount of disability and deformity (12).
The present study is original research conducted in Jeddah, Saudi Arabia, and is a leading investigation for assessing and comparing dental and medical physicians’ knowledge and practice levels regarding OL. According to the results, an almost similar percentage of dentists and physicians are already familiar with oral potentially malignant disorders, even though dental professionals showed a slightly higher percentage than physicians. Knowledge about this disorder is important for all healthcare workers who are involved in the diagnostic and management aspects. The success rate of early detection of these malignant illnesses, which in the past have gotten less attention than lesions of other cancer kinds, will be impacted by one's understanding of oral potentially malignant disorders, particularly leukoplakia (13). One should be aware of and understand that, depending on their degree of experience, different healthcare professionals have different levels of knowledge concerning oral leukoplakia (14). Leukoplakia is the most frequently found oral potentially malignant disorder as compared with others. Most dental practitioners recognize that leukoplakia lesions are a more common malignant disorder in the oral cavity. As many as 30% of the respondents from physicians don’t know the contributing factors to leukoplakia, and 70% of them accept that tobacco is the causative factor. According to Scully (15), the etiology and predisposing factors for oral potentially malignant disorders are smoking, alcohol, betel quid or areca nut chewing, immune system disorders, sun radiation, genetic factors, and others. This was in line with the knowledge level of causative factors among dental professionals, 62.15% correctly identified tobacco, 11.6% identified alcohol, and 4.2% identified genetic factors as the causative factors. This finding suggested that dental professionals would be able to give patients who had undergone the examination and diagnosis greater educational information. Dentists should be knowledgeable of the reasons for biopsying any oral lesion, not just leukoplakia. Probably in most parts of the world, dentists are not typically educated to conduct a biopsy; they instead refer to a specialist for such a procedure (14). According to the question assessing knowledge of the clinical characteristics of leukoplakia lesions, the majority of doctors were knowledgeable about them and responded that the diagnostic feature was a white, non-scrapable lesion that could not be removed (77.1%), whereas the dental profession was unaware of it in 24.2% of participants. Both professionals also identified proliferative verrucous leukoplakia as the OL with the highest malignant transformation and erythroplakia as the second.
When the hypothesis test was conducted, the p-value obtained was <0.001 which implies that there was a significant difference between the knowledge scores among the dental and physician respondents included. The results of the current investigation showed that knowledge scores are significantly higher in the dental field as well as in family medicine physicians and otolaryngologists in Riyadh, Saudi Arabia. A study conducted by Dewi et al., stated that all levels of dental students had adequate knowledge of leukoplakia is an oral potentially malignant disorder (16). Similarly, in our study, the dental respondents had higher theoretical knowledge about leukoplakia
When observing the results of respondent practice related to leukoplakia, physicians were more likely to screen tobacco-using patients than dentists. Further support is also gained from other international researchers, Macpherson et al., (17) stated that medical practitioners examined patients’ mouths, usually in response to a complaint of soreness or as a result of the practitioner’s knowledge of a pre-existing oral condition. Among the dental respondents, they carried out an examination for oral cancer during the course of routine examination, which is lower than medical practitioners. Many of the respondents, the dentists (77.9%), explain the risk factors for the use of tobacco better than physicians (67.1%). However, physicians were more likely to screen patients affected by leukoplakia. There was a general feeling that the dentist was the key primary care professional to undertake opportunistic oral cancer screening. However, physicians were more likely to examine patients than dentists. This implies that physicians encountered leukoplakia patients more than dentists and have adequate experience with the patients. The results of this study indicated that, theoretically, most of the dental professional respondents understand the predisposing factors, diagnostic features, and other characteristics of leukoplakia disorder, and they were more likely to explain the risk factors for the use of tobacco to the patients than physicians. This implies that dentists are less experienced in dealing with leukoplakia cases but have good theoretical knowledge of OL.
According to physician responses in our study, patients with leukoplakia were either referred to the maxillofacial department or the oral medicine department, while 21% of dentistry respondents were unsure about the referral department. It's possible that this is because there isn't much experience with OL instances. In contrast to our study, Macpherson et al. (17) found that dental respondents tended to adhere to the reference criteria more than their medical colleagues. Lack of knowledge about the referral department and criteria has effect on how treatments turn out, as a timely referral and early therapy increase survival prospects. Depending on their level of experience, different healthcare professionals have different levels of knowledge regarding OL (18). In our study, also consultants and specialists were found to have significantly higher knowledge than others.
To the best of our knowledge, no other study has examined the knowledge and practices of the dental profession and physicians regarding OL. This study does have possible strengths and limitations. The strengths of this investigation were that it was conducted with a group of health care professionals seeking employment in both private and government sectors. The conclusions may therefore be representative of all dental and family care physicians. Even though our study findings need to be interpreted with the following limitations. Initially, the study did not classify the knowledge scores into different levels among the respondents.
Conclusion
From this study, it may be concluded that most of the dental professionals in Riyadh, Saudi Arabia have higher theoretical levels of knowledge about leukoplakia than family medicine physicians and otolaryngologists. The study also showed that there is a significant difference between the knowledge scores across various levels of dental and medical professionals regarding the knowledge scores. The current investigation finds that dentists are less experienced in dealing with leukoplakia cases but have good theoretical knowledge of them. Additional training is needed for both dentists and physicians to improve their understanding of leukoplakia as a malignant transformation and its associated risk factors, as well as to improve primary care practitioners' capacity to identify possibly carcinogenic intra-oral lesions.
Disclosure
Conflict of interest:
There is no conflict of interest
Funding:
No funding
Ethical consideration:
The study was approved by institutional review board (IRB) of King Saud University in Riyadh with approval number: IR-0302, project number E-18-3385.
Data availability:
Data that support the findings of this study are embedded within the manuscript.
Author contribution:
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.