Volume 2, Issue 1
January 2022
Hereditary Hemorrhagic Telangiectasia: A Case Report with Hematuria as Primary Presentation
Ali S. Albrahim, Tarek A. Swellam
DOI: http://dx.doi.org/10.52533/JOHS.2021.2102
Keywords: case report, hereditary hemorrhagic telangiectasia (HHT), Rendu-Osler-Weber Disease, Curaçao’s diagnostic criteria, urinary tract telangiectasia, hematuria
Hematuria is a concerning sign that warrants evaluation because it may signal the presence of a genitourinary malignancy. Full urologic evaluation for hematuria must be done after excluding pseudohematuria, history of nephrological pathology, trauma, or recent urologic manipulation. One of the rare causes of gross hematuria: hereditary hemorrhagic telangiectasia (HHT) that must be considered in the differential diagnosis of haematuria of unknown cause. In this case we describe a rare primary presentation of hereditary hemorrhagic telangiectasia with painless gross haematuria and urethral bleeding. We present a case of a 21-year-old Saudi male with a history of painless gross haematuria and urethral bleeding. Urinary tract infection (UTI), nephropathy and bleeding diathesis had been investigated and were excluded. Computed tomography (CT) scan showed no pathological lesions. The patient underwent urethro-cystoscopy and multiple telangiectatic lesions were observed in the penile urethra and in the trigone of the bladder. We also found another telangiectasias lesion in the oral mucosa. With these findings, this patient was diagnosed with probable HHT based on Curaçao’s diagnostic criteria. However, other differential diagnoses other than solitary telangiectasia of the bladder were excluded. HHT, despite a rare cause, must be considered in the differential diagnosis of haematuria of unknown cause. Conservative management with close follow up to prevent complications can be a potential line of management in these cases with stable condition before proceeding to medical or surgical treatment.
Introduction
Hematuria is a concerning sign that warrants evaluation because it may signal the presence of a Genitourinary malignancy in up to 25% of patients with this complaint. Hematuria can present with gross or microscopic variations. Gross hematuria is often alarming to the patient making him present to the medical care for evaluation. Risk factors that come with hematuria and increase suspension to genitourinary malignancy are age of patient, presence of irritative voiding symptoms, smoking, industrial chemical exposure, analgesic abuse or chronic foreign objects in the urinary tract (1).
Gross hematuria must be differentiated from pseudohematuria, whereby the urine may appear red because of dehydration, certain medications, or food. Pseudohematuria initially excluded by absence of red blood cells in microscopic urine examination. After excluding pseudohematuria, history of renal disease, trauma, or recent urologic manipulation. The physician should give the patient a full urologic evaluation for hematuria according to the American Urological Association (AUA) guidelines (2).
HHT or Rendu-Osler-Weber Disease is one of the scarce causes of gross hematuria. It is a rare fibro-vascular dysplasia that makes vascular walls susceptible to injury with minor trauma leading to skin and mucosal bleeding. The genetic pattern of the disease is an autosomal-dominant inheritance. However, in about 20% of the cases it can be present with no family history and can be idiopathic (3). It is characterized by telangiectasis lesions on the face, hands and or mucosal membrane. In addition, arterio-venous malformations can be found in several organs as well as a positive family history. With advance of age, the telangiectasis increase in number and in prominence, and episodes of bleeding become more frequent (4). Bleeding telangiectasis in the genitourinary tract may be controlled by local or systemic measures. Conservative management with close follow up to prevent complications can be a potential line of management in these cases with stable condition before proceeding to medical or surgical treatment.
Case Report:
A 21-year-old Saudi male came to the emergency department for sudden onset of urethral bleeding and painless gross haematuria. On presentation, there was no active bleeding nor gross hematuria. He was evaluated and discharged from the emergency department after excluding any active emergency issues and referred to a urology clinic. During follow up with urology, the patient gave a history of painless gross haematuria and urethral bleeding that occurred on two occasions three days apart. Urethral bleeding lasted for a few seconds and was followed by one episode of gross hematuria on each occasion. There was no history of gastrointestinal or respiratory bleeding and there were no other urinary tract symptoms such as dysuria, urgency nor urinary incontinence. Patient didn't have any history of spontaneous epistaxis. He is single and he denied any sexual contact nor history of trauma and no history of similar events. No family history of similar presentation and a negative history of gastrointestinal, respiratory or genitourinary bleeding. There are no known congenital or genetic disorders in the family. However, genetic testing was not done as it is not available in our facility. He is medically free, not on any medication and no past surgical procedures. Lastly, the patient does not smoke and has no history of drug abuse or chemical exposure.
On examination, we noticed a telangiectasis lesion in the oral mucosa located in the soft palate that blanch with applying pressure, no other telangiectatic lesions were found. UTI, nephropathy, bleeding diathesis had been investigated and were excluded. Regarding his laboratory investigation, his White Blood Cell (WBC) was 8.6 K/uL, hemoglobin 13.7 g/dl, platelet 272 109/L, creatinine 0.93, blood urea nitrogen (BUN) 25. Meanwhile his bleeding profile showed a Prothrombin Time (PT) of 15.2, Partial Prothrombin Time (PTT) of 35.9 and International Randomized Ratio (INR) of 1.12. In addition, urine analysis showed red blood cell casts with the rest of the results unremarkable.
Computed Tomography (CT) scan of the abdomen and pelvis was normal and showed no pathological lesions. He was scheduled for urethro-cystoscopy a week after, during which he hadn’t any episode of bleeding. During the procedure, urethral meatus was narrow and was dilated using a 26 French foley catheter. With advancement of the cystoscope, we observed multiple telangiectasis lesions in penile urethra distal to the sphincter and in the trigone of the bladder near the right ureteric orifice that bleed with bladder distension (Figure 1). Wash cytology was done and proved negative for high grade urothelial carcinoma; no biopsy was taken.
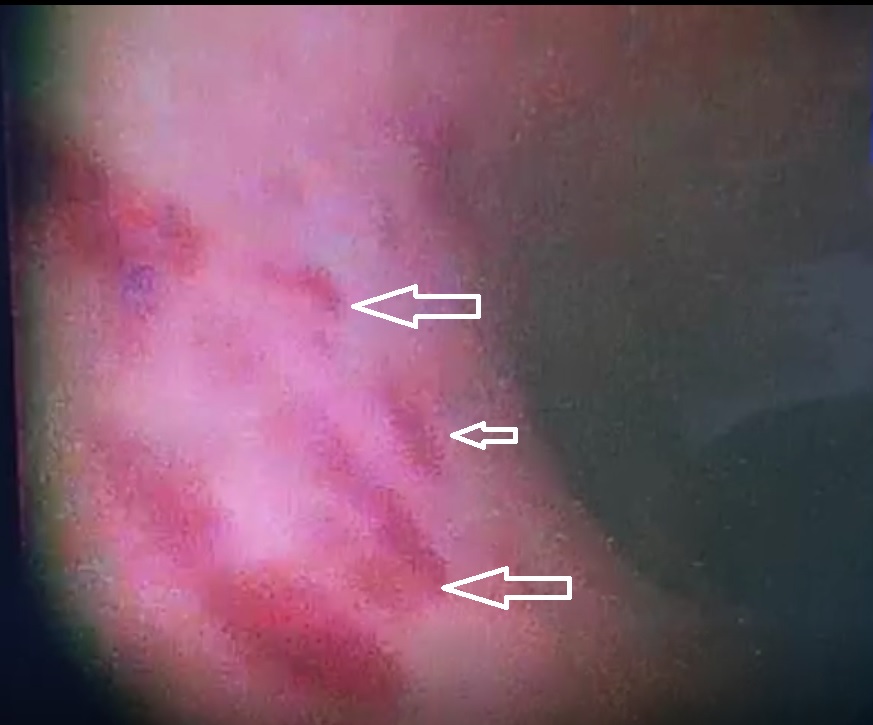
Figure 1. Telangiectasis lesions in the penile urethra (white arrows)
Furthermore, we noticed that the telangiectatic lesions of the bladder were more prone to bleed with bladder distention during cystoscopy. So, we advised the patient to frequently empty the bladder with the early sensation of fullness. After four months, another follow up in the clinic was done and the patient had no single episode of urethral bleeding nor gross hematuria. The patient is on the priority follow up list and will be evaluated on a regular basis.
Discussion:
HHT or Rendu-Osler-Weber Disease is a rare fibro-vascular dysplasia that makes vascular walls susceptible to injury with minor trauma leading to skin and mucosal bleeding. It’s an autosomal-dominant inheritance, although there is no family history in about 20% of the cases (3). Patients with HHT initially present with recurrent spontaneous epistaxis. Haematuria is an unusual presentation with few reported cases presented initially with haematuria. It’s unusual for telangiectasia to involve lower urinary tract in patients with HHT although the telangiectatic lesions of this condition are often widespread, urinary tract involvement occurs in nearly 3% of these cases (5).
As with any rare disorder, patients with HHT suffer from the considerable long delay of being diagnosed if they have been done. A questionnaire-based retrospective study concluded that many patients go with this disorder without being diagnosed and this is because the disease is unnoticed without any attention-grabbing symptoms as the variable penetrance of its clinical manifestations, inadequate disease awareness among patients and their family and/or there is poor awareness among healthcare professionals as this disorder is characterized by high variability of clinical features with many other common diseases (6).
It is recommended to do a thorough work-up to individuals with haematuria, including CT urogram, urethro-cystoscopy, urine culture, cytology and bleeding profile. Even if telangiectasis in the lower urinary tract were seen, other more common causes of haematuria must be considered and ruled out. Despite normal clotting parameters, patients suffer several haemorrhagic episodes from these telangiectasis. To the best of our knowledge, there are a total of five case reports where telangiectasia has been observed by cystoscopy in the lower urinary tract (5, 7-10). Only one of these five cases in which histologic confirmation of lower tract telangiectasia was made (4).
Although genetic testing is now being used to diagnose HHT, diagnostic clinical manifestations of this disorder still are being used for this purpose. HHT manifests age-related penetrance with the average age of onset for epistaxis is 12 years and about 100% affected by the age of 40. Most patients had telangiectasis of the face, hands and or mouth that manifested 5-30 years after the onset of epistaxis. The clinical manifestations of this disorder show variability among the patients even within the same family members. Diagnostic clinical criteria known as the Curaçao Criteria were developed (table 1) (11). The diagnosis of HHT is considered ‘definite’ if three or more criteria are present, ‘possible’ if two criteria are present, and ‘unlikely’ if one or no criterion is present. Sensitivity and specificity of the Curaçao Criteria is unknown, but the experts agreed that the Curaçao Criteria are especially helpful in discriminating the affected from non-affected older adults and to keep HHT within the differential diagnosis in younger adults and children. It's commonly seen for the affected children and young adults to present with arteriovenous malformations especially in those who are not manifested with epistaxis, telangiectasia or symptoms of solid organ pathology. The risk of missing diagnoses among these age groups is worrisome and should be carefully sought. For that reason, genetic testing should be the most useful among these (12-13).
Table 1 Curaçao Criteria for clinical diagnosis of hereditary hemorrhagic telangiectasia (HHT) (11).
|
Criteria |
Description |
|
Epistaxis |
Spontaneous and recurrent |
|
Telangiectasia |
Of skin, face and mucosal membranes |
|
Visceral lesions |
Gastrointestinal telangiectasia, pulmonary, hepatic, urinary, cerebral or spinal arteriovenous malformations |
|
Family history |
A first-degree relative with HHT according to these criteria |
In this patient, we found telangiectasis lesions in the urinary tract with few lesions in the oral mucosa. Patient denied any history of recurrent epistaxis, but according to age-related penetrance, 100% of patients are affected by age 40 years. Meanwhile, the patient’s family history was non-significant, and his parents were still within the young adult age group. Meanwhile, a study has related the blood group O to be genetically responsible for the HHT and that is thought to be coupled to the gene responsible for this disorder (5). Similarly, our patient blood group was O but genetic testing was not available in our facility.
According to Curaçao Criteria, this patient is possibly having HHT that genetic testing required for confirmation of diagnosis. However, the other differential diagnoses other than solitary telangiectasia of the bladder were excluded. Bleeding telangiectasis can be controlled by local or systemic measures. Local compression and cauterization have frequently relieved bleeding skin and mucous membrane telangiectasis. One option of controlling bleeding is by ligation of the vessel which is not effective in these cases because the defect is within the vessel wall.
It has been noticed that there is a consistent raise of plasminogen activator in the dilated telangiectatic vessels. Assuming that Epsilon Aminocaproic Acid (EACA) should antagonize the fibrinolysis triggered when angiomas bleed, epistaxis was successfully controlled with topical EACA in 1 patient (14). Harrison DFN reported that a successful management of 20 patients with HHT were treated with daily doses of 0.25-1 mg of Ethinyl Estradiol. However, none of these patients had hematuria (15). Since Harrison’s original work, Cooney has noticed an exacerbation of bleeding in females with this disorder who have taken estrogen for contraception (16). Rowley PT concluded that the obvious paradox between these can be resolved by retrieving that minor rise in systemic estrogen levels, as in pregnancy and chronic liver disease, which can promote vascular proliferation which is reflected in the telangiectasia as an increase in fragility leading to traumatized vessels. Conversely, higher estrogen levels induce epithelial metaplasia which will toughen the skin or mucosa overlying the telangiectasia (17).
In our case, we noticed that telangiectatic lesions of the bladder are prone to bleed with bladder distention during cystoscopy. So, we advised the patient to frequently empty the bladder with the early sensation of fullness. Follow up four months later and with restricting to the conservative management, the patient had no single episode of urethral bleeding nor gross hematuria. The patient is on the priority follow up list and will be evaluated on a regular basis.
Conclusion
Conservative management for patients known to have HHT presenting with gross hematuria and urethral bleeding is a valid option in stable patients before proceeding to medical or surgical treatment.
Disclosure
Statement:
The authors declare no conflict of interest.
Funding:
The case did not have any funding.
Ethical Consideration:
Consent was taken from the patient to publish the case. We thank the patient and the institution of Dammam Medical Complex for accepting to publish the case.
Data Availability:
All data is found within the article.
