Volume 5, Issue 8
August 2025
Polymer-Based Dental Composites: A Critical Analysis of Mechanical and Aesthetic Properties
Anwar Hassan Alzahrani, Muath Muhammad Benten, Faisal Salem Alkully, Khalid Mustafa Ballol, Abrar Yousef Johari
DOI: http://dx.doi.org/10.52533/JOHS.2025.50806
Keywords: resin composite, polymerization shrinkage, mechanical properties, aesthetic properties, filler size and load
Restorative dentistry focuses on preventing, diagnosing, and treating dental diseases affecting tooth function and aesthetics. It encompasses procedures like fillings, crowns, and bridges, traditionally requiring tooth structure removal, which can compromise tooth integrity and lead to further decay. Resin composite restorations offer better aesthetics and allow for more conservative tooth preservation, bonding effectively to dental tissues. However, they have drawbacks like polymerization shrinkage and moisture sensitivity during placement. Resin composites consist of an organic matrix, fillers, and coupling agents. Fillers enhance mechanical properties and make up 30% to 70% of the volume, improving radio-opacity and hardness while reducing shrinkage. Restorations are affected by masticatory forces, leading to deformation over time. These forces include shear, compressive, tensile, and bending forces. The strength of resin composites is primarily influenced by filler load, which improves hardness and wear resistance until a threshold is reached where matrix adhesion weakens. Polymerization shrinkage, occurring during light-curing, can lead to postoperative sensitivity and marginal gaps. Strategies to minimize this shrinkage include altering viscosity and using alternative monomers. Layering techniques during application can reduce polymerization shrinkage but are time-consuming, prompting the use of bulk-fill composites, which save time and exhibit lower shrinkage. Additionally, resin composites must match the optical properties of natural teeth, with factors like refractive index affecting opalescence and fluorescence, critical for aesthetic restoration, stability, and enhanced polishability. Resin composites have become the most used material for direct restorations in dentistry. However, despite significant advancements, there are still several challenges that need to be addressed. Ongoing research and innovation are crucial for resin composites to reach their full potential as the ideal material for direct restorative applications. This review article analyzes the mechanical and aesthetic properties of polymer-based dental composite restorations and their relevance in clinical applications.
Introduction
Restorative dentistry is a branch of dentistry that specializes in preventing, diagnosing, and treating dental diseases that affect the function and aesthetics of the tooth (1). Restorative dentistry includes fillings, crowns, and bridges. Traditionally, it was based on removing tooth decay or defects in addition to other tooth structures to accommodate a restoration. For instance, preparing for crowns and bridges recommends tooth reduction and total enamel removal, which compromises the tooth integrity, rendering it susceptible to fracture and further decay (2, 3). Dental restorations are either direct or indirect restorations.
Direct restorations are less time-consuming, less expensive and require less removal of tooth structure (4). One of the most used direct restoration materials is amalgam. Amalgams are of low cost, have a high survival rate, high compressive strength, high tolerance to masticatory forces, high wear resistance, are less technique-sensitive, and are less sensitive to moisture contamination. However, amalgam restorations are not esthetic, do not preserve tooth structure, tend to cause marginal leakage with time, and are unable to adhere to dental tissues (4). In response to the limitations of traditional restorative materials, a variety of alternative options have been developed for dental restorations, such as resin composite restorations.
Composite restorations offer several advantages: they exhibit superior aesthetic qualities, allow for a more conservative approach to tooth preservation, and possess the ability to bond effectively to the natural tooth structure. Additionally, these materials typically require less extensive tooth preparation compared to other options (4).
However, composite restorations have drawbacks, including polymerization shrinkage, which can result in the formation of gaps between the restoration and the tooth. Furthermore, these materials are susceptible to moisture contamination during the placement process, demanding a high level of technique sensitivity. They may demonstrate increased occlusal wear in areas subjected to significant stress. Over time, inadequate bonding can lead to marginal percolation, further compromising the longevity and efficacy of the restoration (4).
Resin composites are composed of three main phases: organic matrix, fillers, and coupling agents. Other components of resin composites are photo initiators, accelerators, and stains (5). Fillers are responsible for enhancing the mechanical and physical properties of the resin composites, whereas coupling agents are responsible for strengthening the adhesion between the fillers and the matrix (5). Photo initiators are particles that react to the external source of energy to initiate the polymerization of resin composites. The organic matrix contains inhibitors to inhibit the premature polymerization of the resin composite if exposed to light (5). The monomers in the organic matrix are often urethane dimethacrylate (UDMA), bisphenol A diglycidyl dimethacrylate (Bis-GMA), TEGDMA, and bisphenol A diglycidyl dimethacrylate (Bis-GMA), or bisphenol A ethoxylate dimethacrylate (Bis-EMA) (5). Inorganic fillers represent 30% to 70% of the volume of composite resins. Fillers include borosilicate, aluminum silicate, quartz, barium, zirconium, ytterbium fluoride, strontium, lithium aluminum silicate, and zinc glasses (5). They increase the radio-opacity of the resin composites, increase hardness, and reduce polymerization shrinkage (5).
This review article seeks to provide a critical analysis of the mechanical and aesthetic properties associated with polymer-based dental composite restorations. The analysis will encompass the fundamental characteristics that contribute to the performance and visual appeal of these materials in clinical applications.
Methodology
This narrative review is based on a comprehensive literature search conducted on July 27, 2025, using ScienceDirect, PubMed, Wiley Library, Dynamed, MDPI, Oxford Academic, BMC, and Cochrane databases. The research utilized Medical Subject Headings (MeSH) terms and relevant keywords, such as polymer-based dental composite and its mechanical and aesthetic properties, to identify studies that examined resin composites and analyzed their different mechanical and aesthetic properties. A manual search was also conducted using Google Scholar, and the reference lists of identified papers were reviewed to locate additional relevant studies. No restrictions were applied regarding publication date, language, participant age, or type of publication, ensuring a broad and inclusive exploration of the available literature.
Discussion
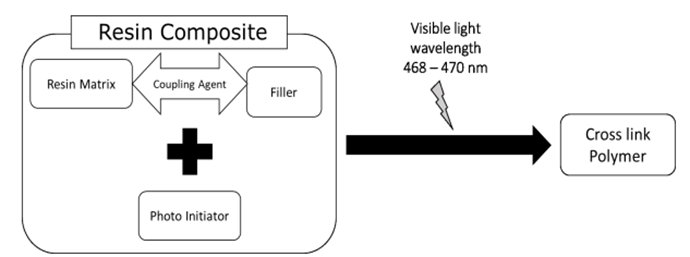
Composites are the most advanced restorative material in current times. They are three-dimensional compounds consisting mainly of organic matrix, inorganic fillers, and coupling agents (Figure 1). The organic matrix binds all the components of the resin composite (6). Resin composite matrix can either contain bis-GMA, UDMA, HEMA, or TEGDMA. Each monomer has an advantage in terms of strength, curing characteristics, or plasticity. Therefore, a composite oligomer matrix was developed, which includes bis-GMA, HEMA, TEGDMA, and UDMA to further increase its mechanical and physical properties (7).
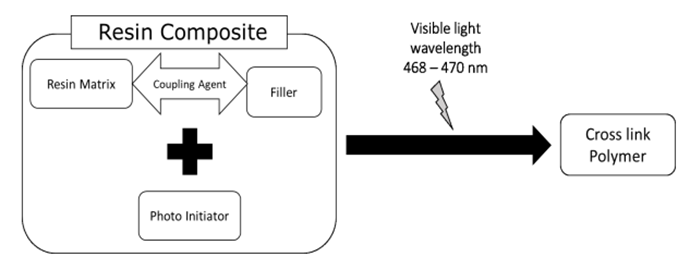
Figure 1: Composition of resin composite (8).
While the organic matrix plays a significant role in the formulation of resin composites, it is the inorganic fillers that emerge as critical components in determining the mechanical properties, aesthetic qualities, wear resistance, and minimizing polymerization shrinkage. These fillers are essential not only for enhancing the strength of the composite but also for influencing its overall performance in clinical applications. Moreover, resin composites are classified based on the size of the filler particles into macrofilled, microfilled, nanofilled, and hybrids (9). Conventional resin composites are macrofilled, with the filler size ranging between 10 and 50 μm. This type of composite showed increased strength; however, it was unable to retain the colour and was difficult to polish. To overcome such aesthetic drawbacks, microfilled resin composites were developed, in which filler size ranged between 40 and 50 nm. Microfilled composites exhibit excellent aesthetic characteristics. However, they demonstrate a marked susceptibility to fractures and exhibit diminished wear resistance, which ultimately leads to a loss of anatomical shape (9). Such disadvantages lead to the development of hybrid resin composites, which contain a few micrometers of glass filler particles and small amounts of colloidal silica particles (10–50 μm and 10–50 nm). This combination of different sizes of filler particles renders hybrid composites aesthetic and has reduced polymerization shrinkage, which makes it the ideal restoration for posterior cavities (9, 10). However, hybrid resin composites are not aesthetically ideal for anterior teeth; hence, nanofilled resin composites were developed. Nanofilled composites contain filler particles whose sizes range between 10–100 nm, resulting in a significant increase in translucency and aesthetics (11). Additionally, the increased filler load in nanofilled resin composites resulted in a significant increase in strength and reduced polymerization shrinkage (12).
Resin composites are classified based on their clinical use into packable composite, bulk-fill composite, and flowable composite (13, 14). Packable resin composites are the most common composites used. They are easy to handle and shape and provide proper proximal contact (14). Flowable resin composites are microfilled with the filler load decreased from 50–70% of the volume of the composite to 37–53%, which increased their flowability and decreased their viscosity. However, strength and wear resistance drastically decreased in flowable composites, and polymerization shrinkage significantly increased. Therefore, flowable composites are recommended to be used to fill low-stress-bearing areas (15). To combine the advantages of both flowable composites and packable composites, bulk-fill composites were developed. Bulk-fill composites allow incremental fill up to 4mm, which occurs during restoration placement. Additionally, it provides better marginal and cervical seals in class II cavities and class V cavities (16-18).
Restorations are susceptible to masticatory forces, which result in deformation of the restoration over time. When masticatory forces are applied to the restoration, internal stresses are generated. These forces are complex and include shear forces, compressive forces, tensile forces, and bending forces (19). Shear forces are the forces applied parallel to the restoration, such as the chewing movements (20), whereas compressive forces are applied vertically to the restoration, reducing its volume, such as the biting force (21). Tensile forces cause the expansion of composites and increase their length (22), whereas bending forces are a combination of compressive and tensile forces (21).
Filler load is the most important factor that affects the strength of the resin composites. It is directly proportional to the mechanical properties; however, when it reaches a certain threshold, the mechanical properties of the restoration start to deteriorate. This is attributed to the reduction of the matrix adhesion strength (23). Additionally, increasing filler load specifically increases the hardness, compressive strength, and flexural modulus. Increasing filler load and decreasing filler particles result in a significant increase in the wear resistance of resin composites. The shape of the filler particles affects the mechanical properties of the restoration as well. For instance, spherical filler particles result in less polymerization shrinkage than irregularly shaped filler particles, hence decreasing the internal stresses produced and increasing the overall strength of the restoration (24).
Resin composites, when exposed to the light-curing process, the monomers start a polymerization process, in which the double bonds between the monomers change into single bonds between polymers, resulting in polymerization shrinkage. This shrinkage ranges between 2% to 14% of the restoration volume (25, 26). Polymerization shrinkage produces internal stresses and transfers them to the cavity walls, which results in postoperative sensitivity, marginal gaps, leakage, and recurrent caries (25). Polymerization shrinkage can be minimized by strategically manipulating factors such as viscosity, polymerization rate, network structure, and conversion rate. For instance, the use of macromonomers tends to lead to lower shrinkage compared to traditional small monomers; however, they often exhibit significantly higher viscosity (26). This increased viscosity can pose challenges in handling the resin composite. In order to decrease polymerization shrinkage in resin composites, Cuevas-Suárez et al. (27) suggested replacing TEGDMA with allyl carbonate monomer (BPhADAC), which can decrease polymerization shrinkage from 5.37% to 4.48%.
Alternative curing methods can contribute to decreasing the percentage of polymerization shrinkage (Figure 2). Soft-start method, in which a low intensity curing starts for seconds, followed by a gradual increase in intensity, can significantly reduce polymerization shrinkage (26).
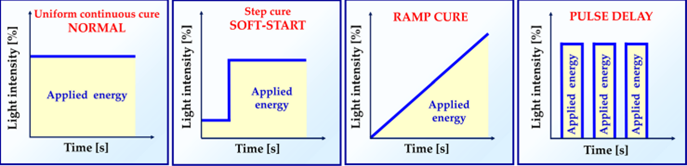
Figure 2: Different curing methods (26).
The application of layering techniques in the use of resin composites is critical and can significantly influence the rates of polymerization shrinkage during the curing process. Specifically, when resin composites are placed in oblique or horizontal increments, this method effectively reduces cuspal deflection, which in turn contributes to a decrease in the overall polymerization shrinkage observed (28). However, it is essential to note that while this layering technique offers advantages regarding restoration stability, it is inherently time-consuming. The meticulous nature of layering demands additional clinical time, which may not be feasible in all dental practice settings (28). Consequently, to address these concerns, the utilization of bulk-fill composites, whether of high or low viscosity, has emerged as a more favorable alternative. Bulk-fill composites significantly reduce the procedural time required for placement. Additionally, they exhibit lower percentages of polymerization shrinkage compared to packable resin composites (28).
Resin composites have several optical properties, such as fluorescence and opalescence. Opalescence is the difference in chroma between the reflected and transmitted colors, while fluorescence is the emission of light by natural teeth that have absorbed light (29, 30). Natural teeth have fluorescence, opalescence, and translucency. Resin composite restoration should match the optical properties of natural teeth. The opalescence of resin materials is determined by the difference in the refractive index of the resin matrix and fillers, whereas the fluorescence of resin materials is determined by the presence of certain fluorescent pigments in their structure (31). Dentin exhibits a yellowish hue and possesses greater opacity compared to enamel. In contrast, enamel is characterized by its translucency, which influences the perceived color of the tooth by scattering light wavelengths predominantly in the blue spectrum. Consequently, the coloration of dentin plays a critical role in determining the overall shade of the tooth. Furthermore, the incisal, middle, and cervical regions of a tooth display varying shades due to differences in the enamel-to-dentin thickness ratio (32). This variation has significant implications for the optical properties of resin composite restoration materials, which are designed with differing levels of opacity to match the natural shade of teeth (32).
The aesthetic qualities of resin composite restorations play a crucial role in dental practice, particularly in the anterior teeth. The importance of gloss and polishability in these restorations extends beyond mere visual appeal; they are fundamental in mitigating the risk of inflammation in the gingival and periodontal tissues (33). Achieving a high degree of gloss and polish not only enhances the immediate appearance of the restoration but also contributes significantly to the long-term survival and functionality of the restoration itself (33). Smooth, polished surfaces are less likely to harbor plaque and bacteria, which are directly linked to periodontal disease. A restoration that retains its smooth surface over time is more resistant to wear and degradation, ultimately leading to better performance and a longer lifespan (33). The size of filler particles is a critical factor influencing both color stability and the maintenance of a smooth, polished surface in restorative materials. Smaller filler particles contribute significantly to the longevity of the restoration, ensuring sustained color stability and enhanced polishability (33).
The aesthetic quality of composite restorations is significantly influenced by the presence of an inhibited oxygen layer during the polymerization process. In composite resins, the monomers located in the superficial layer are unable to undergo complete conversion into polymers when exposed to atmospheric oxygen. This inhibition leads to diminished aesthetic outcomes and contributes to an increased susceptibility of composite materials to staining. Over time, these restorations can absorb chromogenic compounds from various food and beverage sources, thereby compromising their visual integrity (34).
To address this limitation, an oxygen-inhibiting gel has been formulated and is recommended for application on the final unpolymerized layer of the composite. This gel works by creating a barrier that mitigates the effects of oxygen, thereby enhancing the degree of monomer conversion. The result is an improvement not only in the aesthetic appearance of the restoration but also in its color stability and overall longevity. However, despite these advancements, it remains crucial to recognize that superficial staining applied to the composite restorations can still lead to the deterioration of composite restorations, necessitating eventual replacement (34).
Moreover, the oral hygiene practices of patients play an instrumental role in the maintenance of composite restorations. Poor oral hygiene can lead to the accumulation of dental plaque and its associated by-products, which can degrade the organic matrix found in resin composite materials. This degradation exacerbates the absorption of extrinsic stains, ultimately resulting in the discoloration of the restoration. It is essential for both dental professionals and patients to acknowledge these factors in order to enhance the durability and aesthetic performance of composite restorations over time. Proper oral hygiene and routine dental care are indispensable components in prolonging the life and aesthetic quality of these dental materials (34).
Conclusion
Resin composites represent a significant advancement in restorative dentistry and have emerged as the material of choice for direct restorations. Over the past few decades, these materials have undergone extensive development aimed at addressing several inherent limitations. The mechanical and aesthetic properties of modern resin composites have evolved to surpass those of traditional direct restorative materials. Despite these advancements, challenges such as polymerization shrinkage remain, necessitating continued research and innovation. Future improvements are essential for resin composites to fully realize their potential as the optimal material for direct restorative applications.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical considerations
This study is a review of previously published literature and does not involve any original data collection involving human or animal subjects. Therefore, ethical approval was not required.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.