Volume 5, Issue 8
August 2025
Ocular Manifestations of Inflammatory Bowel Disease in Saudi Arabia: A Systematic Review of the Past 13 Years
Reem Babakr, Ahmed Almanjoumi, Areej Guoziz
DOI: http://dx.doi.org/10.52533/JOHS.2025.50802
Keywords: Inflammatory bowel disease, Chron’s disease, Ulcerative colitis, ocular manifestation, Uveitis, Episcleritis, Scleritis
Ocular extraintestinal manifestations (O-EIMs) in inflammatory bowel disease (IBD) are significant but often underrecognized complications that can affect patient outcomes. In Saudi Arabia, limited data exist on the prevalence, clinical patterns, and management of O-EIMs in IBD patients. This systematic review evaluates existing research to provide a comprehensive analysis of O-EIM burden, highlighting prevalence clinical manifestations and treatment gaps. This review was conducted following PRISMA guidelines. A comprehensive search of PubMed, Scopus, Cochrane Library, Google Scholar, and Web of Science was performed for studies published between January 2012 and January 2024. Inclusion criteria were original studies—including cross-sectional, case-control, and cohort (prospective or retrospective) designs—that reported on the prevalence, clinical manifestations, or treatment of O-EIMs in IBD patients in Saudi Arabia. Exclusion criteria comprised non-English publications, non-original articles (e.g., reviews, editorials), studies lacking relevant clinical outcomes, and those with major methodological flaws. Seven articles were included that provided data on O-EIM prevalence, risk factors, and treatment approaches among Saudi IBD patients. The prevalence of O-EIMs ranged from 0.5% to 2.8%, except for one study reporting 76.9%, which relied on self-reported surveys. Episcleritis and uveitis were the most common conditions, with episcleritis significantly associated with IBD flares. Despite their clinical impact, only 9.7% of affected patients received ophthalmology referrals. Medical management across the reviewed studies focused on controlling disease activity. O-EIMs were addressed in limited studies, with treatment modalities including topical corticosteroids, lubricants, antibiotics, NSAIDs, and surgical interventions. Findings indicate that O-EIMs are underdiagnosed and undertreated in Saudi IBD patients. Improved screening protocols, interdisciplinary collaboration, and ophthalmologic referral pathways are needed to enhance early detection and optimize patient care.
Introduction
Inflammatory Bowel Disease (IBD) is a set of inflammatory disorders that include Crohn's Disease (CD) and Ulcerative Colitis (UC), which primarily affect the gastrointestinal (GI) tract and are associated with systemic consequences. While the core symptoms of IBD, such as abdominal discomfort and diarrhea, are GI-focused, extraintestinal manifestations have a considerable influence on other organ systems, including the skin, joints, hepatobiliary tract, and eyes (1, 2). Among these ocular manifestations referred to as ocular extraintestinal manifestations (O-EIM’s) are particularly concerning since they have the potential to cause discomfort, pain, and visual impairment, thereby compromising IBD patients’ quality of life (1). Some O-EIM’s may not result directly from the disease process, but rather as an adverse effect of chronic pharmacologic therapy of IBD, further highlighting the need for increased clinical awareness and research into their overall burden and implication (3).
The reported prevalence of O-EIMs varies widely across studies, influenced by population characteristics and methodological differences. Mintz et al., in a UK-based study, reported ocular complications occur in fewer than 10% of IBD patients (4). A meta-analysis by Li et al. showed that patients with CD have 1.6-fold higher odds of developing uveitis compared to those with UC, a difference more pronounced in European cohorts—underscoring regional heterogeneity and the importance of context-specific data (5). In a French cohort of 1,432 IBD patients, 3.7% were diagnosed with O-EIMs or treatment-related ocular complications. Inflammatory surface diseases were most common (33.2%), followed by uveitis (14.9%), episcleritis (5.7%), and scleritis (2.3%) (6).
EIMs can cause significant morbidity in IBD patients (7). Early identification and monitoring of O-EIMs in IBD is essential due to their potential severity. Patients with joint or skin involvement, or non-specific ocular complaints, should be promptly referred, as episcleritis may reflect bowel activity and uveitis can precede gastrointestinal symptoms (8, 9). Monitoring is especially important in high-risk subgroups, such as those receiving 6-MP therapy, where EIM prevalence is increased (10).
Various risk factors have been proposed to influence the development of O-EIM’s in IBD patients. Active intestinal disease has been consistently associated with ocular symptoms such as episcleritis, especially in Crohn’s disease patients (10). Female gender has been found to be associated with the development of ocular EIMs, alongside other systemic factors such as arthritis and colonic disease location, which have shown significant correlation with ocular involvement suggesting shared immunopathogenic mechanisms (4, 5, 10, 11). Additionally, smoking has been linked to increased risk of ocular manifestations in patients with ulcerative colitis, highlighting modifiable environmental risk factors (12). An association has been observed between O-EIMs and the chronic use of some pharmacological agents including corticosteroids and 5-aminosalicylic acid (5-ASA) (3, 13). These findings underscore the multifactorial etiology of ocular EIMs in IBD.
Episcleritis may correlate with intestinal disease activity and resolves with IBD control, while scleritis and uveitis may occur independently and demand more aggressive management, including topical or systemic corticosteroids and immunosuppressants (14). Prognosis is generally favorable with prompt treatment; however, recurrent or untreated uveitis can lead to vision loss and complications such as glaucoma or cataracts (15).
Despite growing identification of O-EIMs, their etiology is not fully understood. Existing research points to the relevance of systemic inflammation, genetic susceptibility, and microbial dysbiosis in the development of these symptoms (1, 16). Several studies outlined a structured approach in managing ocular manifestations of IBD, with consensus emerging around the role of anti-inflammatory and immunosuppressive therapies. Mild cases of episcleritis are often self-limiting and require only supportive care or topical agents, whereas anterior uveitis and scleritis may necessitate topical corticosteroids and cycloplegics, escalating to systemic corticosteroids in refractory cases. Notably, biologic agents have demonstrated efficacy in managing persistent or severe O-EIMs, particularly when associated with active intestinal disease (2-4).
This systematic review sought to evaluate the O-EIMs of IBD in Saudi Arabia over the previous 13 years. This systematic review aims to assess the prevalence, characteristics, risk factors, and clinical management of O-EIMs in IBD patients in Saudi Arabia.
Methods
Search Strategy
This systematic review was conducted in accordance with the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guideline. A comprehensive literature search was performed using five electronic databases: PubMed, Scopus, Cochrane Library, Google Scholar, and Web of Science, covering studies published between January 2012 and January 2024. The search strategy employed Medical Subject Headings (MeSH) and keyword combinations including: “Inflammatory Bowel Disease” (IBD), “Ocular Manifestations”, “Eye Diseases”, “Saudi Arabia”, “Crohn Disease”, “Ulcerative Colitis”, “Eye Complications”, “Uveitis”, “Scleritis”, “Episcleritis”, “Conjunctivitis”. Boolean operators such as AND/OR were used to refine results, and filters were applied to restrict studies to humans and English language publications.
Inclusion and Exclusion Criteria
Studies were included if they were published in English between January 2012 and January 2024, conducted within Saudi Arabia, and investigated ocular manifestations in patients with IBD. Eligible study designs included cross-sectional, case-control, retrospective, and prospective cohort studies. Included studies had to report on the prevalence, clinical presentation, associated risk factors, or management of O-EIMs in IBD patients.
Studies were excluded if they were not original research (e.g., reviews, editorials, commentaries, case reports), were published in languages other than English, or lacked clinically relevant outcomes. Studies with serious methodological limitations, such as poor data collection, unclear outcome definitions, or lack of peer review, were also excluded.
Review Outcomes
The primary outcome of this review was the prevalence of ocular extraintestinal manifestations in IBD patients. Secondary outcomes included characteristics, risk factors, and clinical management strategies employed in Saudi Arabia.
Study Selection Process
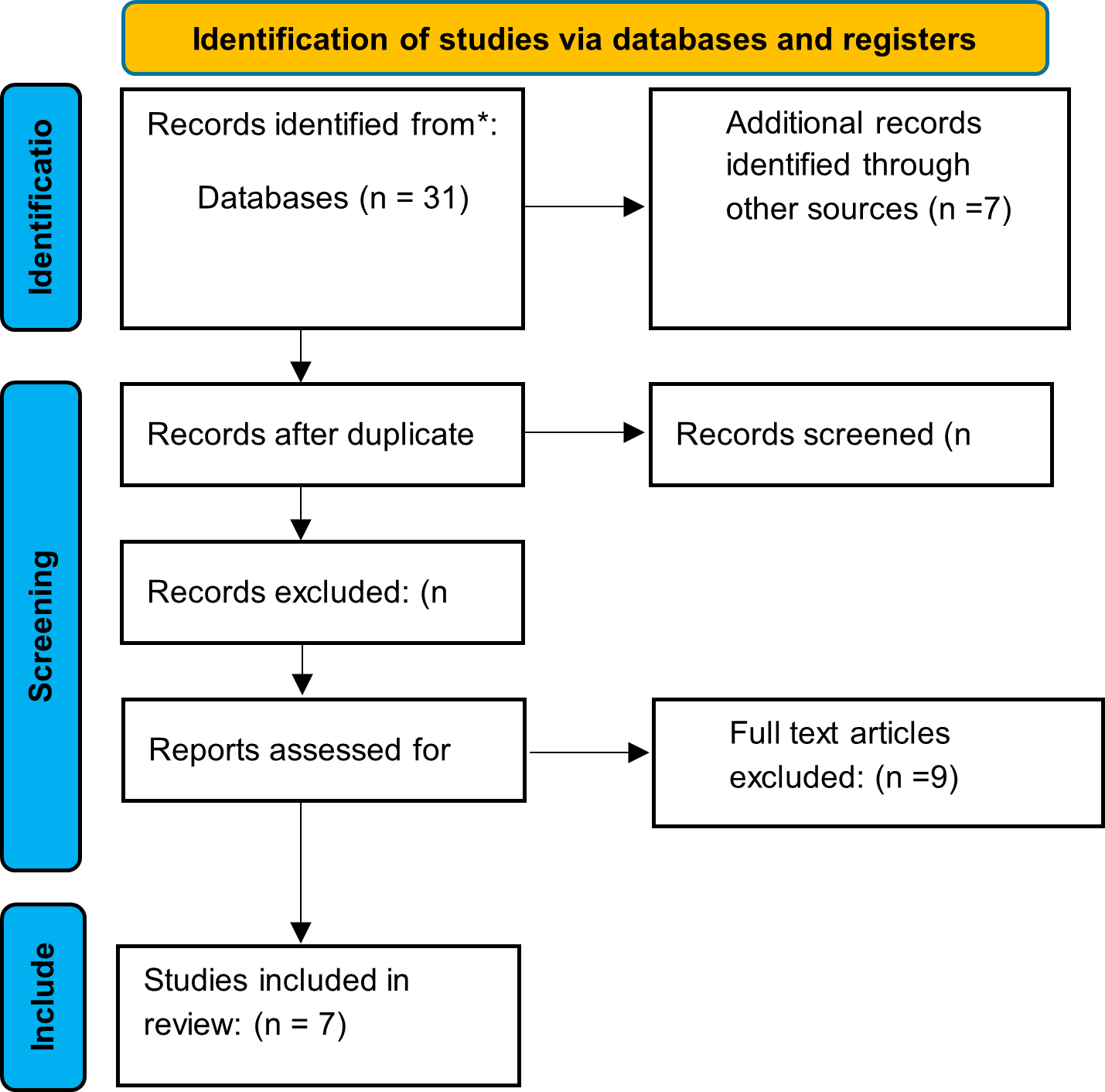
Two independent reviewers screened titles and abstracts for eligibility based on the predefined criteria. Full-text articles were retrieved for potentially eligible studies and evaluated in detail. Discrepancies were resolved through discussion and consensus. The study selection process is outlined in the PRISMA flow diagram.
Data Extraction and Synthesis
A standardized data extraction form was developed to capture relevant information from each included study. Key variables extracted included: author name, year of publication, study design, sample size, participant demographics (age, gender), type of IBD, prevalence and types of O-EIMs, associated risk factors, management approaches, and key conclusions. Data extraction was performed independently by two reviewers, and discrepancies were resolved through discussion to ensure consistency and minimize errors. Due to heterogeneity in study designs and outcome definitions, results were synthesized narratively without conducting a meta-analysis.
Quality Assessment and Risk of Bias
The methodological quality of included studies was independently assessed by two reviewers using the Joanna Briggs Institute (JBI) Critical Appraisal Checklist for Analytical Cross-Sectional Studies. This tool evaluates eight domains: clarity of inclusion criteria, description of setting and participants, validity and reliability of exposure and outcome measures, identification and management of confounding factors, and appropriateness of statistical analysis. Each study was rated as “Yes,” “No,” or “Unclear” for each domain. All included studies clearly stated the inclusion criteria, and clearly defined objectives and settings, standard diagnostic criteria were applied across studies. But several studies failed to identify or address potential confounding factors. Self-reported data and absence of standardized ophthalmologic assessment contributed to detection bias in some studies.
Results
Search Results
A total of 38 records were identified through database searching (n = 31) and other sources (n = 7). After removing duplicates, 26 records remained for screening. Of these, 10 were excluded based on title and abstract. The full texts of 16 articles were assessed for eligibility, resulting in the exclusion of 9 studies that did not meet the inclusion criteria. Ultimately, 7 studies were included in the final systematic review. The study selection process is summarized in the PRISMA flow diagram (Figure 1).
Quality Assessment Results
The overall methodological quality of the included studies was moderate. Most studies showed clear inclusion criteria, reliable outcome measure, and an appropriate statistical analysis. However, a key limitation across studies was the lack of identification and control of confounding factors. Although standardized criteria were used to define exposures and outcomes, none of the studies employed strategies such as stratification or multivariate analysis to address confounding. Despite these limitations, the studies provided relevant data to address the review objectives (Table 1).
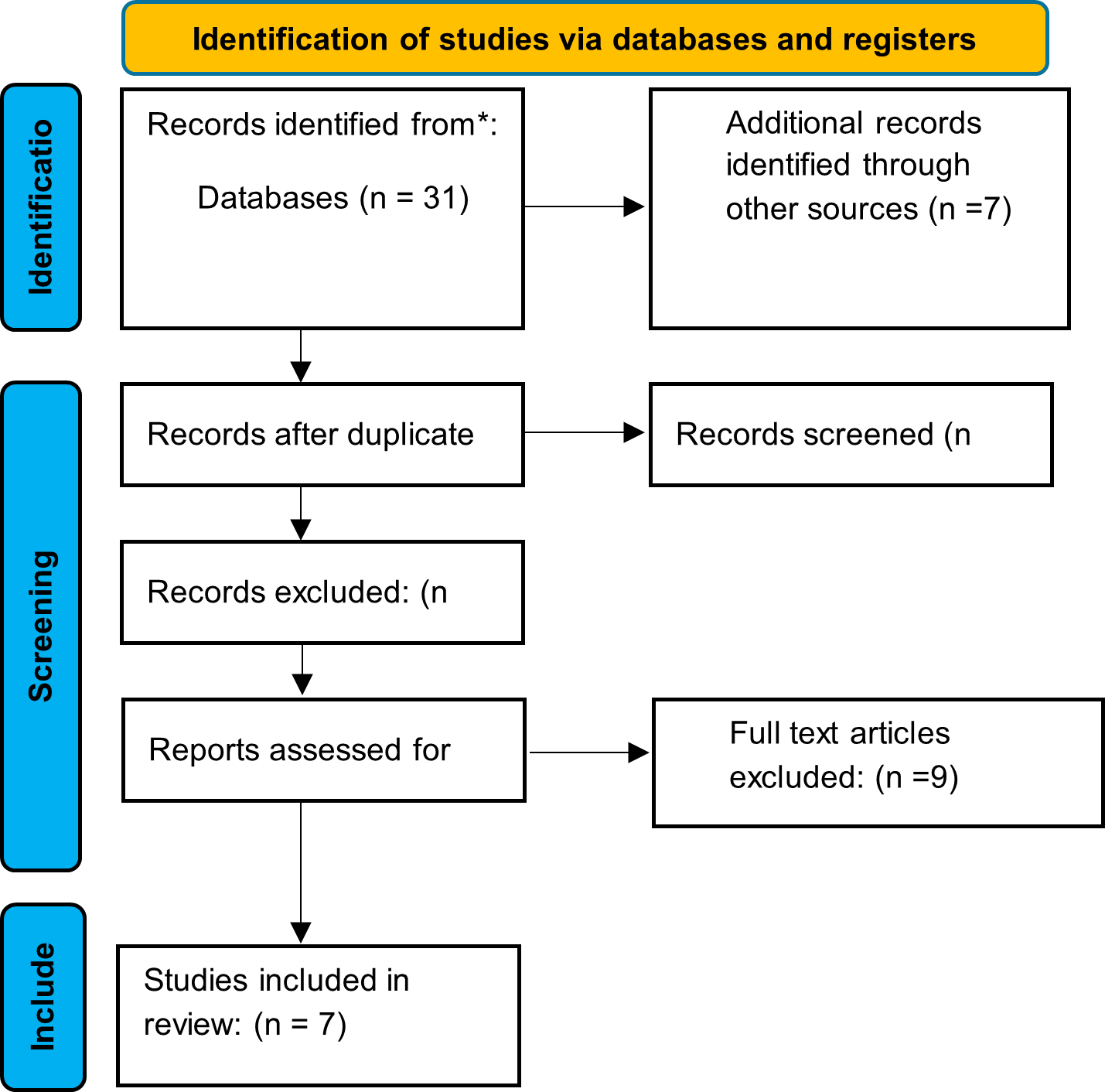
Figure 1: PRISMA Flow Diagram of Study Selection Process
|
Table 1: Risk of Bias Assessment |
|||||||||
|
Reference |
Were the criteria for inclusion in the sample clearly defined? |
Were the study subjects and the setting described in detail? |
Was the exposure measured in a valid and reliable way? |
Were objective, standard criteria used for measurement of the condition? |
We’re confounding factors identified? |
Were strategies to deal with confounding factors stated? |
Were the outcomes measured in a valid and reliable way? |
Was appropriate statistical analysis used? |
|
|
Alotaibi et al. (10) |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
Yes |
|
|
Alreheili et al. (11) |
Yes |
Yes |
Yes |
Yes |
No |
No |
Yes |
No |
|
|
Fadda et al. (17) |
Yes |
yes |
Yes |
Yes |
Yes |
No |
Yes |
Yes |
|
|
Alharbi et al. (18) |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
Yes |
|
|
Alghamdi et al. (19) |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
Yes |
|
|
Aljohani et al. (20) |
Yes |
Yes |
Yes |
Yes |
No |
No |
No |
Yes |
|
|
Al-Fawzan et al. (21) |
Yes |
Yes |
Yes |
Yes |
Yes |
No |
Yes |
Yes |
|
Characteristics of Included Studies
This systematic review aimed to assess the prevalence, characteristics, risk factors, and clinical management of ocular extraintestinal manifestations in IBD patients in Saudi Arabia. The review includes seven studies published between 2012 and 2024 (10, 11, 17-21), encompassing a total of 2,258 IBD patients. Among the included studies, all were retrospective in design except for one cross-sectional study (19). One study focused on a pediatric population under 14 years of age, where gender distribution was not specified (11), while the remaining studies included patients of various age groups, with a mean age ranging from 25.5 to 33.6 years. Across the studies, gender distribution was relatively balanced, though there was a slight male predominance in most cases (Table 2).
|
Table 2: Demographic Data of IBD Studies |
||||
|
Sample Size |
Mean Age (Years) |
Male (%) |
Female (%) |
Reference |
|
578 |
32±11 |
54% |
46% |
10 |
|
66 |
<14 |
N/M |
N/M |
11 |
|
312 |
25.5±10.6 |
48.7% |
51.3% |
17 |
|
394 |
30.2±0.6 |
51% |
49% |
18 |
|
216 |
N/M |
49.5% |
50.5% |
19 |
|
435 |
38.3±16.2 |
55.6% |
44.4% |
20 |
|
257 |
33.6 |
52.2% |
47.8% |
21 |
N/M =not mentioned
Risk of Bias Within Studies
Risk of bias across the included studies was mainly attributed to the lack of strategies for dealing with confounding variables and, in some cases, inadequate statistical analysis. While outcome measurements were generally valid and reliable, and participant selection was clearly described, the omission of confounding adjustment raises concerns about internal validity in 10 and 11, for instance, did not identify or address confounding factors and apply appropriate statistical methods, contributing to a higher risk of bias. In contrast, studies 18 and 21 demonstrated relatively stronger methodological consistency, though still lacked confounding control. Overall, the studies showed moderate risk of bias, primarily due to analytic and confounding limitations.
Synthesis of Results
The prevalence of O-EIMs was rare in most reviewed literature ranging from 0.5% to 2.8 % except in one study that specifically assessed the ocular manifestations of inflammatory bowel disease in Taif region of Saudi Arabia during the COVID-19 pandemic the previlance was 76.9% based on self-reported survey (10, 11, 17-21). A total of 187 O-EIMs cases were reported, and while most studies did not detail specific ocular conditions, those that did primarily reported Uveitis and Episcleritis (10, 11, 20). Conjunctivitis was assessed in one patient with ulcerative colitis (20) (Table 3).
|
Table 3: Ocular Extraintestinal Manifestations in IBD Studies |
|||||
|
Study |
O-EIMs %CD |
O-EIMs %UC |
Total O-EIMs N (%) |
EIM in N (%) |
Ocular Manifestation Type |
|
10 |
NS |
NS |
1 (1.5%) |
65 (11.2%) |
Uveitis |
|
11 |
1(2.5%) |
0 |
1 (1.5%) |
21 (31.8%) |
Uveitis/Episcleritis |
|
17 |
4 (2%) |
2 (1.7%) |
6 (NM) |
110 (NM) |
NS |
|
18 |
NS |
NS |
5 (1.5%) |
NM |
NS |
|
19 |
NS |
NS |
166 (76.9%) |
NM |
Various ocular symptoms (Impaired vision, photophobia, redness, pain, discharge) |
|
20 |
1 (0.3) |
1 (0.3) |
2 (0.5) |
133(31%) |
Episcleritis, Conjunctivitis. |
|
21 |
3 (2.3%) |
3 (2.3%) |
6 (2.3%) |
45 (17.5%) |
NS |
CD= Crohn’s Diseases UC= Ulcerative Colitis, O-EIMS= Ocular Extraintestinal Manifestations
EIM=Extraintestinal Manifestations, NR= Not specified, NM= Not mentioned
In a study conducted in Taif, where ocular symptoms were reported by patients using a self-reported survey, 16 participants (9.7%) reported that ocular symptoms occurred prior to gastrointestinal symptoms. The study explored a wide range of OEIMs of IBD. The most commonly reported symptom was impaired vision, affecting 39.4% of participants. This was followed by acute eye redness in 26.9%, photophobia in 23.1%, and severe eye pain accompanied by headaches or nausea in 22.7% of cases. Additionally, 20.4% of respondents experienced seeing halos around lights, indicating a significant prevalence of ocular discomfort among IBD patients in this cohort (19) (Table 4).
|
Table 4: Specific Ocular Manifestation |
||
|
Ocular Manifestation |
Number of Patients |
Percentage (%) |
|
Impaired vision |
85 |
39.4% |
|
Acute eye redness |
58 |
26.9% |
|
Photophobia |
50 |
23.1% |
|
Severe eye pain with headache/nausea |
49 |
22.7% |
|
Seeing halos around lights |
44 |
20.4% |
|
Red, swollen, itchy eyelids |
37 |
17.1% |
|
Severe irritation or burning |
33 |
15.3% |
|
Pain or tenderness on palpation |
28 |
12.9% |
|
Watery or purulent discharge |
18 |
8.3% |
|
Fading or yellowing of colors |
17 |
7.9% |
There is limited data that focused on O-EIM of IBD, and few studies have explored their association with specific risk factors in Saudi Arabia. This gap in research makes it challenging to assess potential correlations with other risk factors. Additionally, it was observed that EIMs were generally more prevalent among CD than in UC (11, 17, 21), when UC had slightly higher prevalence of EIMs it was mostly related to musculoskeletal manifestations (10, 20). No significant correlation was found between extrintestinal symptoms and factors such as gender, age, smoking (19, 20). However, positive Family history of IBD was marked as significant risk factor in one study that focused on assessing ocular manifestations among IBD patients, in the same study it was noted that ocular symptoms and active IBD flares were reported where 43.4% of patients reporting worsening eye symptoms during disease exacerbations. Despite this relatively high prevalence, most affected patients were not referred to an ophthalmologist, and only 9.7% received an ophthalmology consultation. Notably, 8–12% of respondents reported a positive family history of IBD, highlighting a potential genetic predisposition (19).
Across seven reviewed studies, medical management generally followed international step-up or top-down approaches and focused mainly on controlling disease activity and maintenance therapy including 5-aminosalicylic acid (5-ASA), in both adult and pediatric patients with UC and CD (11, 17, 18). Corticosteroids were commonly used for inducing remission with steroid dependency noted. Thiopurines such as azathioprine and 6-mercaptopurine were prescribed, often for maintenance or steroid-sparing purposes. Biologic therapy including anti-TNF agents was increasingly used more commonly in CD patients (11, 17, 18, 20, 21). Ocular manifestations management was only mentioned in one study and treatment strategies included topical steroids, cycloplegics, systemic corticosteroids, immunosuppressants, and biologics (19) (Table 5).
|
Table 5: Treatment Modalities in O-EIMs in IBD Patients |
||||
|
Treatment Modality |
Number of Patients Treated |
Percentage (%) |
Number of Documents Citing |
Referenced Documents |
|
Topical corticosteroids |
47 |
21.8 |
2 |
15, 16 |
|
Cool compresses |
47 |
21.8 |
1 |
15 |
|
Topical lubricants (Artificial tears) |
40 |
18.5 |
2 |
15, 17 |
|
Antibiotics |
18 |
8.3 |
3 |
15, 16, 17 |
|
NSAIDs |
22 |
10.2 |
3 |
15, 16, 17 |
|
Surgical intervention |
3 |
1.4 |
1 |
15 |
|
No treatment given |
10 |
4.6 |
2 |
15, 17 |
Outcome Measures
The primary outcome measure across the included studies was the prevalence of ocular extraintestinal manifestations among patients with IBD. This was reported either as a percentage of affected patients within the study population or as the number of ocular events identified. Secondary outcome measures included the type and frequency of specific ocular conditions, such as uveitis, episcleritis, and, in rare cases, conjunctivitis. Several studies also evaluated ocular symptom profiles, including impaired vision, eye redness, photophobia, and eye pain, particularly during IBD flares. Also, in one study, temporal relationship between ocular and gastrointestinal symptoms was evaluated, noting that ocular complaints preceded GI symptoms in (9.7%) of patients. Additional outcome measures included the association of ocular symptoms with disease activity, where (43.4%) of patients reported worsening eye symptoms during IBD exacerbations, and the rate of ophthalmologic referral, which was notably low at (9.7%) (19). Treatment-related outcomes were also described, such as the use of systemic therapies (e.g., 5-ASA, corticosteroids, anti-TNF agents, immunosuppressants) and topical or supportive interventions (e.g., corticosteroid drops, cool compresses, lubricants). In a minority of cases, surgical intervention was reported.
Discussion
This systematic review aims to assess the prevalence, characteristics, risk factors and clinical management of ocular extraintestinal manifestations in IBD patients in Saudi Arabia. The review includes seven studies published between 2012 and 2024. Across most of the reviewed literature, O-EIMs were found to be relatively rare, with a prevalence ranging from 0.5% to 2.8%, which aligns with global data. A meta-analysis conducted by Kilic et al. in the United Kingdom reported a pooled incidence of O-EIMs of 0.02 (95% CL, 0.01-0.03) in UC and 0.03 (95% CL, 0.02-0.06) in CD, further confirming the low but significant occurrence of O-EIMs in IBD patients. Similarly, a systemic review by Li et al found that O-EIMs, particularly uveitis and episcleritis, were more prevalent in CD than in UC, with pooled odds ratios indicating a significantly increased risk in CD patients. These findings underscore the importance of early recognition and management of O-EIMs to prevent potential sight-threatening complications (5, 22).
An exception in our review was a study conducted by Alghamdi et al. in Saudi Arabia, which reported an exceptionally high prevalence of O-EIMs at 76.9% (19). This outlier percentage raises important considerations, since it stands in contrast to the lower prevalence rates reported in other studies from Saudi Arabia. One possible explanation is that O-EIMs have been underreported in the region, possibly due to limited screening or lack of standardized diagnostic approaches. Supporting this theory, a study by Lee et al. found that 72.1% of IBD patients exhibited ophthalmologic manifestations, with dry eye syndrome being the most common at 57.4% (23).
The disparities in prevalence across studies reviewed in this article highlight the variability in reported rates and underscore the urgent need for standardized diagnostic criteria and consistent ophthalmologic evaluation in IBD care to more accurately determine the true burden of O-EIMs.
This review identified several factors potentially associated with an increased risk of developing ocular manifestation in patients with IBD. The most prominent risk factors observed was active disease, with 43.4% of participants reporting that ocular symptoms worsened during IBD flares. Episcleritis appeared to be a flare-related risk factor in adult patients. This finding is consistent with global evidence (19). Two studies, by Mintz et al. and Thomas et al., identified disease flares as a strong predictor of episcleritis and scleritis in patients with IBD, supporting disease activity as a key risk factor for ocular involvement (4, 24).
Although international literature has reported Crohn’s disease as a potential risk factor for developing O-EIMs. A meta-analysis by Li et al. found that uveitis and episcleritis were significantly more prevalent among Crohn’s disease patients, local literature did not confirm statistical association between IBD subtypes and specific ocular manifestation (5). This may be attributed to the methodological limitations in bias assessment, where confounding factors related to ocular involvements were really identified and controlled among IBD patients.
Another relevant risk factor discussed in the literature is disease extent. One of the included studies done in Saudi Arabia by Alotaibi et al. reported a higher frequency of EIMs among patients with extensive colitis (10). This aligns with findings from Troncoso et al. who showed that patients with pancolitis had a significantly higher risk of developing EIMs including ocular forms than those with limited disease (25).
Despite the recognition of these risk factors, ophthalmologic referral remains low in local studies. Only 9.7% of symptomatic patients in our review were referred for specialist evaluation according to Alghamdi et al. Published in 2021, in Taif (19), highlighting a missed opportunity for early intervention. This aligns with trends reported in global studies. For instance, Cuny et al. found that less than 5% of IBD patients had ocular manifestations, primarily dry eye and uveitis but suggested this figure may reflect underdiagnosis due to low screening rates (6). This supports the idea that the low prevalence reported in most Saudi studies (0.5–2.8%) may not represent the true burden of O-EIMs, particularly when combined with low referral patterns. These findings collectively underscore the importance of early identification of high-risk patients and the incorporation of routine ophthalmologic evaluation in IBD management. A multidisciplinary approach, ensuring collaboration between gastroenterologists and ophthalmologists, remains crucial for timely diagnosis and prevention of irreversible ocular damage.
The most commonly reported ocular extraintestinal manifestations in IBD patients across reviewed studies were episcleritis and uveitis (10, 11, 20), aligning with global observations. Episcleritis typically presents during active disease flares, while uveitis can occur independently of IBD activity according to Li et al. (5).
Interestingly, although the methodology and healthcare settings differ substantially between Alghamdi et al. and Cuny et al., the prevalence of key ocular symptoms is remarkably aligned. In the Taif-based survey, Impaired vision (39.4%), acute eye redness (26.9%), photophobia (23.1%), and severe eye pain with headaches or nausea (22.7%), with (20.4%) experiencing halos around lights (19). While these rates slightly exceed those typically reported internationally, the symptom patterns are consistent and closely paralleling findings from the French cohort where 25% reported redness, 23.2% acute visual loss, and 17.2% ocular pain. This convergence suggests that patient-reported symptom surveys, when well-structured can offer valuable insight into the burden of ocular manifestations in IBD, even outside formal clinical diagnoses. However, the key divergence lies in the clinical confirmation rate: while only 3.7% of patients in the Cuny study received a formal ocular EIM diagnosis including dry eye in (17.2%), uveitis (14.9%), episcleritis (5.7%), and scleritis (2.3%) (6). Alghamdi’s study reflects broader symptomatology that may or may not correspond to underlying pathology. Together, these findings reinforce the importance of integrating both subjective and objective data in IBD care.
These findings underscore the necessity for clinical evaluations to differentiate true O-EIMs from other ocular conditions and highlight the importance of standardized diagnostic criteria in assessing ocular symptoms in IBD patients.
Across the seven reviewed studies the evaluation of O-EIMs was inconsistent, with limited emphasis on standardized diagnostic approaches. One study mentioned diagnoses based on self-reported symptoms rather than formal clinical assessment, and only one study explicitly mentioned referral to an ophthalmologist (19). None of the included studies utilized structured ophthalmologic tools such as slit-lamp examination or grading systems, and no diagnostic protocols were described to differentiate O-EIMs from non-specific ocular complaints. This lack of standardized assessment likely contributed to variability in reported prevalence and limits the accuracy of symptom attribution.
In terms of management, treatment strategies varied depending on the severity of symptoms and the specific ocular condition most of treatment strategies mentioned focused on controlling disease activity (11, 17, 18). One study by Alghamdi et al. reported that among patients who were referred to the hospital for ocular symptoms 56.6% of patients with O-EIMs received cool compress and topical treatment only, while 18.7% received oral or injection medications, and 3.6% underwent surgery (19). Across the reviewed studies, corticosteroids and immunosuppressants such as azathioprine were frequently used, and biologic agents such as infliximab to manage IBD flares (10, 11, 17, 20, 21). However, none of the studies evaluated the use or effectiveness of biologics for ocular manifestations. This stands in contrast to international findings, particularly anti-TNF agents like infliximab and adalimumab have demonstrated high efficacy. These biologics are now widely recommended for both intestinal and extraintestinal disease control, emerging agents, including vedolizumab and ustekinumab, show promise for difficult-to-treat cases, although more data are needed to clarify their role (26).
To improve outcomes, standardized ophthalmologic screening should be integrated into routine IBD care in Saudi Arabia, especially during flares. Prospective, multicenter studies using structured diagnostic criteria and objective assessments are needed. Additionally, closer collaboration between gastroenterology and ophthalmology teams is essential to enhance referral practices and provide timely, evidence-based care for patients with ocular complications.
Limitations
This review has several limitations. The number of included studies was relatively small, and their geographic distribution was limited, which may affect the generalizability of the findings to the broader Saudi IBD population. Most studies were retrospective and observational in design, limiting the ability to draw causal relationships. Across the included literature, there was a lack of standardized diagnostic protocols and formal ophthalmologic evaluations, making it difficult to distinguish true ocular extraintestinal manifestations from unrelated ocular complaints. These gaps highlight the need for prospective, multicenter studies using standardized diagnostic criteria and objective ophthalmologic assessments.
Conclusion
This systematic review assesses the prevalence, characteristics, risk factors and clinical management of ocular extraintestinal manifestations in IBD, significant variability in prevalence estimates the need for standardized diagnostic criteria. Despite ocular symptoms affecting up to 43.4% of patients during IBD flares, ophthalmologic referrals remain critically low (9.7%), emphasizing the need for interdisciplinary collaboration. Ophthalmologic screening should be integrated into IBD management, improved referral pathways between gastroenterologists and ophthalmologists are necessary. By implementing standardized screening and management protocols, clinicians can improve early detection, reduce complications, and enhance patient quality of life.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical considerations
This study is a systematic review of previously published literature and does not involve any original data collection involving human or animal subjects. Therefore, ethical approval was not required.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis and final writing of the manuscript.