Volume 1, Issue 7
October 2021
The Leading Causes of Recurrent Hospitalization of Neurologically Impaired and Disabled Pediatric Patients in King Abdulaziz Medical City- Jeddah from 2013 to 2017
Sahar Baloush, Hatoon Althobaiti, Raghad Alawfi, Sara Abed, Muhammed Khan
DOI: http://dx.doi.org/10.52533/JOHS.2021.1704
Keywords: children, neurological impairment, disability, global developmental delay, hydrocephalus, cerebral palsy, admission, causes
Background
Disabilities are a major issue, affecting 15% of the world’s population. They are mostly caused by NI such as GDD, CP, hydrocephalus, and HIE. Patients of such conditions, especially children, are more likely to require admission and healthcare. Therefore, it is necessary to investigate the causes that may lead these children to have multiple admissions
Methods
A cross-sectional study was conducted by reviewing medical records of patients who were admitted to the pediatric ward of King Khalid National Guard Hospital, Jeddah, Saudi Arabia from 2013-2017 with any underlying NI. These impairments included any previous diagnosis of GD, CP, HIE, encephalitis, hydrocephalus, or corpus callosum agenesis. A non-probability convenience sampling technique was used to recruit patients who were under 15 years of age with the mentioned diagnoses, and all of the identified 265 patients were included in this study.
Results
Analysis of a total of 635 admissions reports that the most common causes of admission in of patients with the mentioned included underlying conditions are other neurological conditions with (n=222, 35%) admissions, mainly due to seizures (n= 64, 10%), hydrocephalus (n=39, 6.1%), and delayed milestones (n=29, 4.6%). The second top category was respiratory conditions and infections (n=164, 25%). Aspiration pneumonia was documented (n=66, 10.4%), making it the top diagnosis in all admission, followed by seizures. The second top documented infection was pneumonia (n=40, 6.3%). The third top category was gastrointestinal infections and conditions. Leading that category is gastroenteritis (n=22, 3.4%) and GER (n=15, 2.4%). There was no There was a statistically significant relationship between NI and the gender of patients (p = 0.170). There was, however, a statistically significant relationship with the age group, feeding rout, home oxygen, documented disability, admission cause, and patient management (p < 0.001).
Conclusion
Specific NI are more associated with certain conditions that are more likely to lead to hospitalization. Recognition of these conditions can be of future help in early detection and prevention of serious complications and morbidity.
Introduction
Disabilities are life-long restrictions that are caused by any form of deviation from normal health, physical, mental, or social, leading to a loss of the normal function (1). Under this broad definition, comes multiple forms of disabilities other than physical and intellectual (1). Therefore, this wide range of disabilities come with significant morbidity, especially if patients suffer from more than one form. Nowadays, disabilities are a significant issue, affecting more than 15% of the entire world population (2). The Center of Disease Control and Prevention (CDC) states that among people living with some form of disability, 46% have movement disability, 39% have intellectual disability, 26% have hearing problems, 21% have sight problems and 43% have more than one form of disability (3). Locally, according to the national demographic survey that was conducted in 2016 by the General Authority for Statistics in Saudi Arabia, there are 667,280 citizens out of 20,064,970 reported with some form of disability at a prevalence rate of 3326 per 100,000, comprising 3.3% of the total population. Out of those, 154,594 were aged <15 years old, contributing to 23% of all disabled citizens of Saudi Arabia (4).
Out of all the possible causes, Neurologically Impairment (NI) stand out as a major cause of disability in children as the prevalence rate has increased by 15.6% between 2001-2001 to 2010-2011 (5). Furthermore, this increase was found to be the highest in children younger than six years with an increase by 62.1% (23.5 per 1,000 to 38.1 per 1,000 population). NI and disabilities can affect the lifestyle of adults and children alike. However, the effect of such conditions is especially apparent in the first years of life, majorly seen as restrictions in movement, speech, vision, hearing, and thinking of growing children, especially since most neurodevelopmental disabilities are acquired at a young age (6). Regarding children up to 15 years of age with disabilities, out of ten thousand children, 428 have minor impairment, while 376 have major impairment (7). In 2001, it was reported that out of 137 cases of disability, 59% had one disability, 22% had two, and 19% had three or more disabilities (8). With such high numbers of affected patients, the influences of disabilities on the overall health of children became more perceivable to the medical community, and the degree of increasing utilization of healthcare is now more noticeable than ever (9). For this reason, this study aims to investigate the main causes of hospitalization of children with neurological impairments and disabilities as well as to discuss possible etiologies behind this issue.
Methods
Study Design & Participants
This is a single-center cross-sectional study which was approved by King Abdullah International Medical Research Center (KAIMRC) Ethical Board Committee and was conducted between January 2013 and December 2017 at King Abdulaziz Medical City in Jeddah, Saudi Arabia. Amongst all patients that we admitted to the pediatric ward, children with diseases of the nervous system or possible disabilities were identified. We included patients diagnosed as Global Developmental Delay (GDD), CP, Hypoxic Ischemic Encephalopathy (HIE), encephalitis, hydrocephalus and corpus callosum agenesis. Other inclusion criteria included complete files and children below the age of 15. Meanwhile, we excluded children who were hospitalized in the intensive care unit, children older than 15 years, admissions of the included patients before diagnosing or documenting the underlying NI and incomplete files. Upon identifying all patients with the targeted underlying NI, all medical records for each admission of these patients were collected.
Variable Construction & Data Collection
The demographic data included age and gender. The included patients have been stratified into three groups according to the age ranges recommended by American Academy of Pediatrics (AAP) (10). These groups are infancy (from birth up to two years of age), childhood (2 - 12 years) and early adolescence (12 - 15 years old). Regarding NI and disability, each underlying NI that was used initially for patient inclusion was listed. In cases where two NI were documented for a single patient on first admission, the medical record notes for that admission was traced back to identify which NI was diagnosed first, or which NI was the initial presentation. In subsequent admissions, if the main diagnosed NI was changed after reevaluation, the new documented NI was used instead. In addition, through reviewing the medical record of the patients, disabilities that developed as a direct complication of the NI were identified and listed, if present, along with the patients’ main feeding route and the use of supplemental oxygen at home. The identified disabilities have been sub-grouped into six categories according to their types as classified by the Ministry of Health. Those classification are physical disability, visual impairments, hearing impairments, educational and intellectual impairment, mental disorders and social and communication disorders. A seventh group was added for patients with no documented disability or were under investigation to diagnose a disability.
The mentioned data was collected mostly from paper-based and electronic medical records. The documented diagnoses on admission were considered the cause of admission and were listed into nine major groups. The metabolic disorders and electrolyte imbalances, systemic infections, surgical, gastrointestinal, neurological, respiratory, musculoskeletal, genitourinary infections and conditions and unclassifiable causes. Additionally, the main provided management throughout the admission was also listed under either diagnostic or therapeutic managements.
Statistical Analysis
Data analysis was done using IBM Statistical Package for the Social Sciences (SPSS Inc., Chicago, IL, USA) version 20.0. Frequencies and percentages were computed for qualitative variables, while means and standard deviations were calculated for quantitative variables and reported in the form of tables. Chi-square test & fisher exact test ware used to compare qualitative variables, such as age groups, admission causes, and provided management with 95% significance level.
Results
Demographics
A total of 265 patients were included in the study with a collective total of 635 admissions. Those who were admitted to the pediatric ward within the specified period had been identified and included after applying the exclusion criteria. Out of the included 265 patients, 149 (56.2%) were males and 116 (43.8%) were females. The ratio of male to female was close to 1:1 throughout all the admissions. However, the number of male patients was slightly higher in the first five admissions as well as in all the admissions collectively. The mean age by years of the admitted was 4.77±3.7, collectively. The mean age remained relatively steady initially but slightly increased after subsequent admissions. A total of 427 (67.2%) of patients were in the childhood age range in all admissions, collectively. On the contrary, early adolescent patients were the smallest group throughout all admission, collectively and in each admission (Table 1). All 265 patients had a total of 635 admissions collectively with an average admission rate of 2.4 times per patient. Out of the 265 included patients, 109 (41.13%) were admitted once, 67 (25.28%) were admitted twice, 38 (14.34%) were admitted three times, and the remaining were admitted ? four times (Table 1).
Table 1: Descriptive data of patient by admission.

Feeding and Oxygen
A total of 488 (76.9%) were feeding orally from the reported admissions. Furthermore, 220 (83%) of patients were feeding orally in the first admission. However, this number decreased substantially with subsequent admission reaching to 20 (64.5%) in the fifth admission. There was 87 (13.7%) of patients who had been using a Nasogastric Tube (NGT) for feeding throughout the investigation period, while 57 (9%) were using a Gastric Tube (GT) with a similar pattern of decrease found in the use of home oxygen as a total of 263 (99.2%) of admissions did not report using it before the first admission, but that decreased to 7 (87.5%) reports out of 8 admitted patients in their eighth admission. However, when reporting the collective admissions, the portion of patients not on home oxygen was 626 (98.6%) (Table 1).
Underlying Neurological Impairment
Around half of the patients (51.7%) had been included in this study due to GDD. Also, half of the patient in the second and third admission had underlying GDD. This declined in subsequent admissions, as other conditions became more evident such as hydrocephalus followed by CP and HIE. Despite that, GDD was still the most common underlying neurological impairment in most subsequent admissions and all admissions, collectively (n=302, 47.6%). On the other hand, the lowest detected underlying impairment was encephalitis. Among the infants, 58 (53.2%) patients were diagnosed with hydrocephalus being the most common underlying cause of NI. In early adolescence, CP was the most common documented underlying NI (n=18, 41.9%), followed by hydrocephalus (n=12, 27.9%) and developmental delay (n=10, 23.3%).
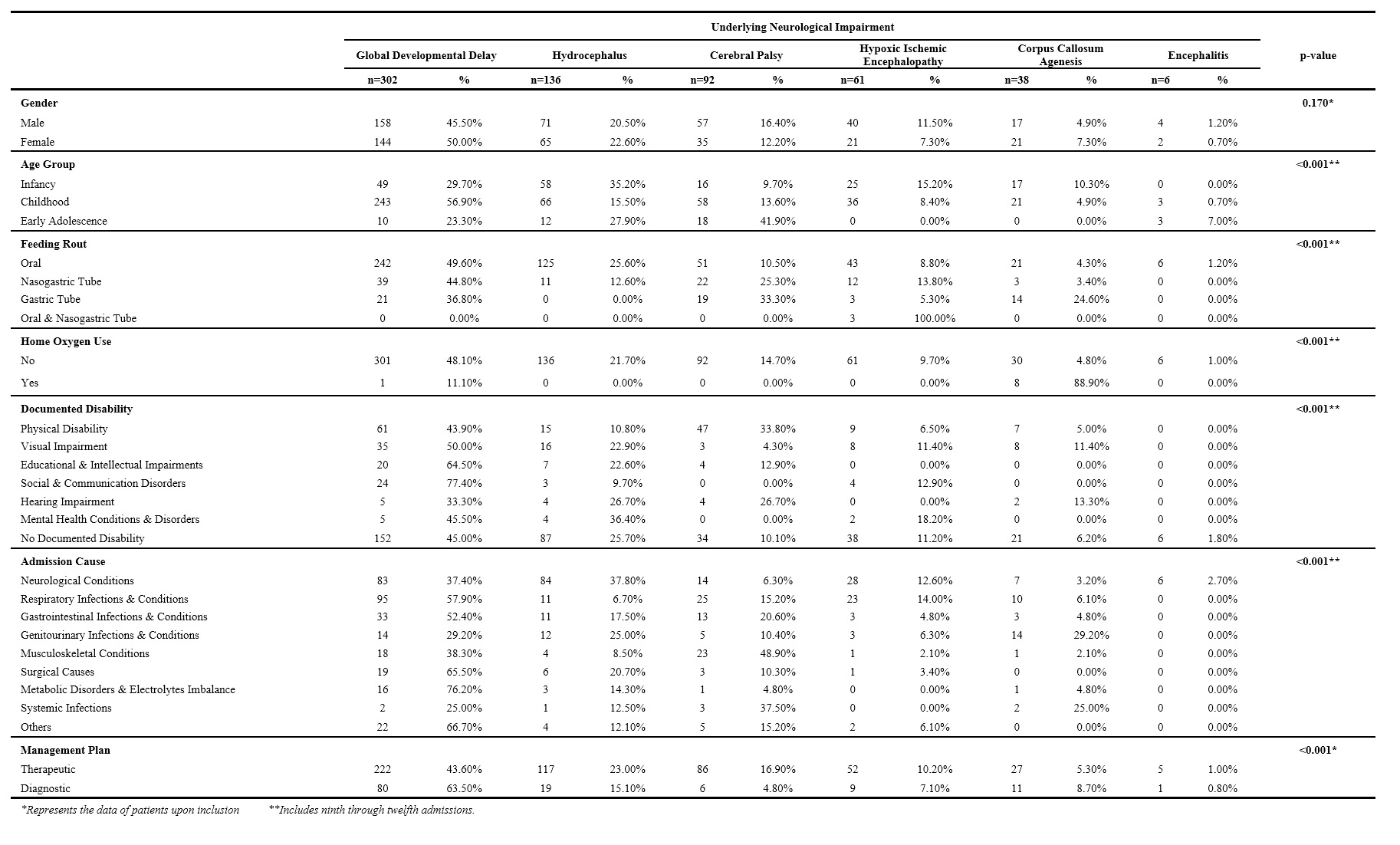
On exploring the relationship between variables, there was no statistically significant relationship between the type of NI and the gender of patients (p=0.170). However, there was a statistically significant relationship with the age group, feeding route, home oxygen, documented disability, admission cause, and patient management (p<0.001). Despite the fact that non-oral feeding routes are most commonly used with GDD, there was still a significant number of patients who were not feeding orally that were admitted with other underlying NI. For instance, 22 (25.3%) patients that were using NGT, and 19 (33.3%) patients that were using GT feeding tube presented with underlying CP (Table 2).
Table 2: Data of patients by underlying neurological impairment.
Disabilities
A total of 338 (53.2%) admissions did not have a documented disability. Physical disability was the highest documented form of disability in all admissions collectively. Relatively, about a quarter to one fifth of patients had documented physical disability in almost each admission. Almost all other forms of disability started with low percentages, but slightly increased with subsequent admissions. The least documented form was mental disability with only 11 (1.7%) (Table 1).
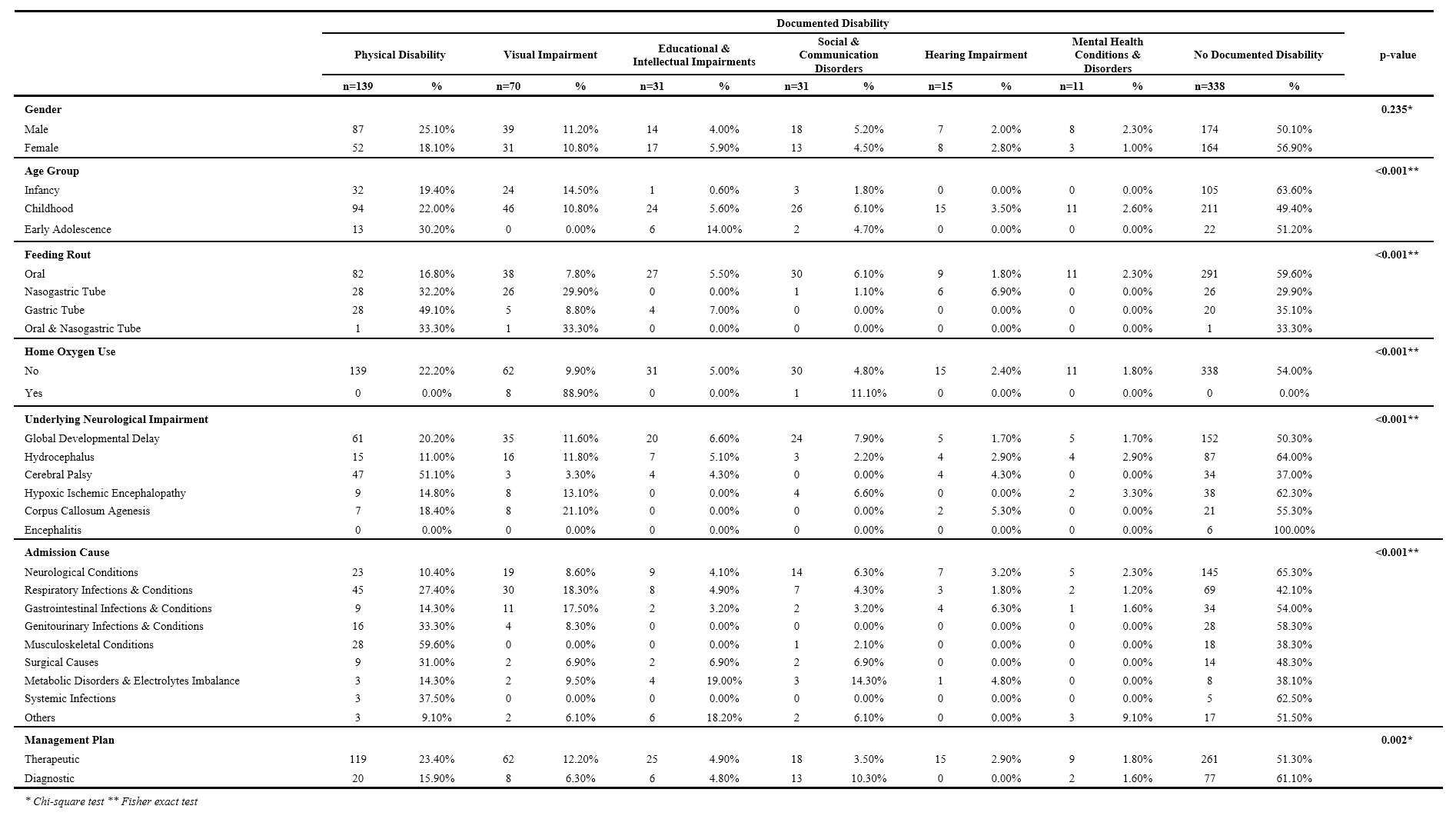
The relationship between the type of documented disability and patients’ gender was not statistically significant (p=0.235). On the contrary, the relationships with the age group, feeding route, supplemental home oxygen use and the cause of admission were statistically significant (p<0.001). Similarly, the relationship between the documented disability and the management plan of patients was statistically significant as well (p=0.002). Excluding the majority of patients that did not have any documented disability, it was noted that physical disability was the most common form of disability documented in association with most of the other variable of this study. Even so, more than half of patients with CP had documented physical disability (n=47, 51.1%), which is more than the cases of CP that did not have a documented disability (n=34, 37%) (Table 3).
Table 3: Data of patients by documented disability.
Leading Causes of Admission
Throughout all admission, neurological conditions as a category was the top cause for admissions (n=222, 35%). Under that category, the highest causative condition was seizures (n=64, 10%), followed by hydrocephalus (n=39, 6.1%) and delayed milestones (n=29, 4.6%). The second top category was respiratory conditions and infections (n=164, 25%) with low respiratory tract infections reported in 112 (17.6%) of all admissions. Out of them, the most common reported respiratory condition was aspiration pneumonia in 66 (10.4%) admission followed by pneumonia in 40 (6.3%). Gastrointestinal infections and conditions was reported in 63, 9.9% admissions with gastroenteritis being the most common (n=22, 3.4%) followed by gastroesophageal reflux disease (n=15, 2.4%) (Table 1).
There was no significant relationship between the causes of admissions and the gender of the patients (p=0.721) and the use of supplemental home oxygen (p=0.826). Conversely, there was a statistically significant relationship with the age group of patients, their main feeding route, underlying NI, documented disability and management during their admission (p<0.001). The neurological conditions mentioned earlier, amongst many others, were the most common documented cause of admission in all age groups. Additionally, it was found that the use of non-oral feeding routes were more likely to lead to respiratory infections and conditions, most prominent of which is lower respiratory tract infections, primarily aspiration pneumonia. When compared with the underlying NI used for inclusion, neurological conditions were the most common cause of admission in patients with underlying hydrocephalus (n=84, 61.8%), HIE (n=28, 45.9%) and encephalitis (n=6, 100%). Similarly, respiratory conditions and infections were the most common cause of admission in patient who had GDD (n=95, 31.5%) and CP (n=25, 27.2%). The second most common cause for admission in patients with CP was admission due to musculoskeletal conditions (n=23, 25%) (Table 4).
Table 4: Data of patients by cause of admission.

Management During Hospitalization
A total of 126 (19.8%) admissions had received diagnostic workup and 509 (80.2%) required therapeutic management. Medical intervention remained the top approach to patients in every admission, mostly via the use of antibiotics, antiepileptics and other types of medications as each case requires (n=304, 47.9%) followed by surgical interventions (n=133, 10.9%). Moreover, Ventriculoperitoneal (VP) shunt insertions and revisions were the most conducted surgery amongst all surgeries (n=34, 5.3%). In the first admission, a total of 126 (25.3%) patients had diagnostic evaluations as their main care plan during the admission. The need for diagnostic work up slowly decreased to reach about 13.7 % in the fourth admission. The top diagnostic tool that was used throughout the first and all the admissions collectively was non-invasive imaging (n=64, 10%) with Magnetic Resonance Imaging (MRI) of the brain (n=52, 8.2%) being the most performed modality. Consequently, electroencephalogram EEG was used in 22 (3.5%) of patients (Table 1).
Discussion
Sample Distribution & Demographics
The percentage of each age group fluctuated in each subsequent admission but remained comparable. It was also found that the mean ages of patients in each admission are relatively comparable to those of patients in all admission collectively. There was an uneven distribution of patients among each individual age group in each admission. However, that is likely due to the uneven age ranges that defined each age group. Nonetheless, those specific age ranges were used per the recommendations of the American Academy of Pediatrics (AAP) as they are more appropriate in describing specific subsets of patients according to common risks, exposures, diseases, and other factors that each age group shares (11).
A trend that was noted when analyzing the demographics of the patients is that most admission occurred in the childhood age range with the biggest contributing factor for this is GDD. By definition, GDD is a significant delay in two or more domains in children less than five years of age (12). Table 2 shows that more than half of all admissions collectively were marked as GDD as an underlying NI. This is due to the fact that GDD may require further investigations for the detection of a possible pathological etiology in case of inconclusive clinical evaluation (13). One of the highest yielding modalities, neuroimaging or brain MRI to be exact, requires admission for pediatric patients. For this reason, it was noticed that many of the first admission with underlying GDD were due to neurological causes, which included delayed milestones, and the documented course of management of these cases was brain MRI. Nonetheless, all other NI can be directly caused by GDD (13). This leads to the overlapping of presentation of other NI to the presentation of GDD. Therefore, even other NI can present with the same expected mean age of presentation in GDD.
Infant younger than two years of age are the second most documented to be admitted with the included underlying NI. The most common underlying NI in this age group was hydrocephalus which can be attributed to the fact that 55% of hydrocephalus cases are classified as congenital (13). Such cases can be detected on ultrasonographic assessment during intrauterine life. After delivery, the infant can present with symptoms and sign. such as progressive macrocephaly, widened fontanelles, and splaying of cranial sutures (14, 15). Similarly, Wammanda et al. reported in their retrospective study that CP was the most common reported neurological disorder (55.3%) in their population (16). On the other hand, Mohamed et al. studied a total of 6019 patients with NI and found that epilepsy was the most common form of NI (52.8%) followed by CP (19.1%) (17). After establishing a clinical suspicion of hydrocephalus, the infant or child may be admitted for further diagnostics, usually neuroimaging, and later for definitive management by insertion of a VP shunt. All of these reasons may explain the high number of admissions on infants with hydrocephalus. Causes of later admissions of children with hydrocephalus may include VP shunt infection or failure. The latter have been documented in up to 40% of patients within two years of shunt insertion (18).
When compared to infants and children, early adolescents had considerably lower admissions. We hypothesize that this is mostly due to having an already established clinical history and management plans. Simply put, the older the patient gets, the less likely that they will present to a hospital because of having been already treated for their underlying NI. They are, however, more likely to present with later complication of their NI than to present with the disease itself. Within this smaller group of patients, 18 of them had been admitted with underlying CP. It is a well-established fact the CP patients are prone for aspiration and aspiration pneumonia. A study reported that 25% of patients with CP develop aspiration (19). In support, it was noted that the top cause for admission of patients with CP is respiratory conditions & infections. Another possible explanation behind the later admission ages of children with CP is the elective admission for corrective surgeries for CP-relater musculoskeletal deformities. It was noted that out of the 92 documented CP-related admissions, 47 (51.1%) of admissions had some form of physical disability while 23 (25%) had musculoskeletal conditions such as deformities, contractures, and spastic joints. Such conditions can be managed by elective surgeries to correct deformities or release tendons. One study on 30 patients with spastic diplegia reported that the mean age for performing muscle-tendon recessions or releases was 8.7 years (4-20 years) (20). Although the mean falls in the range of the childhood age group, the range is quite wide, and it includes early adolescents.
Feeding Route
If the first admission, 83% of the included patients were taking orally. This number continued to decline till it reached 64.5% in the fifth admission as more patient had been converted to NGT or GT feeding. Of all cases documented to be on NGT or GT feeding, most had underlying GDD or CP, 44.8% and 36.8% respectively. This finding can imply the presence of a relationship between GDD and CP and the development of feeding problems. In fact, the presence of feeding problems has been associated with developmental disabilities in up to 80% of cases (20,21). Many neurologically impaired or disabled children require the insertion of an NGT or GT at some point of their lives for many reasons. Some of which include the need for nutritional status correction, impaired cognition, and most importantly, feeding problems. Depending on the cause of the NI or disability, the mechanisms behind feeding problems may differ. For example, mentally retarded children may display selective eating as a feeding problem, while patients with CP have detectable oromotor and neuromotor dysfunction leading to the development of dysphagia, GER, and chocking spells (22). When looking at these two examples of feeding problems, it is possible to infer that the spectrum of management of feeding problems may range from simple behavioral approaches to more invasive managements, such as the use of NGT or the insertion of a GT for feeding. That depends, of course, on the magnitude of the underlying problem. One study has longitudinally followed up 57 children who were severe CP patients after the insertion of a GT, most of whom had significant debilitating neuromotor impairment (23). The study reported significant weight gain and improvement in overall health during and after the follow up period of 1 year. Taking CP as an example, CP causes significant neuromotor dysfunction that, as explained earlier, can lead to feeding problems such as inadequate intake, oral dysphagia, oropharyngeal dysphagia, GER. These serious problems, in addition to being a burden on their own, can lead to the development of serious complications. Some of which include poor weight gain, growth failure and aspiration pneumonia. In order to avoid such conditions, the insertion of a GT has become a necessary choice.
Another finding of this study was the significant relationship between the feeding routs and disabilities. More than half of the included patients who were on NGT or GT have some form of disability. The top two forms were physical and visual disability. This finding replicates the findings of Strauss and co-investigators who have found that the use of feeding tubes was associated with almost every form of disability they investigated in a study than included 4921 children with severe disabilities and mental retardation (24). Despite the necessary use of tube feeding, the risk of developing feeding problems-related complications still remains real, and the insertion of a GT still carries significant risk and is more likely to be associated with worse outcomes if the degree of the disability is not high enough to warrant the insertion (24).
Global Developmental Delay
The prognosis of GDD can be quite variable, and a portion of children with GDD may not require extensive medical care after receiving proper initial evaluation. Shevell et al. detected a surprising finding when it comes to the developmental prognosis of children with GDD. The initial severity of GDD predicts the future functional level of a child, not their future developmental course (21). Another study by Riou et al. found that the initial diagnosis of GDD may not be associated with objectively measured cognitive skills (22). These findings can imply that the diagnosis of GDD is not necessarily associated with further deterioration in neurological development (21). Furthermore, GDD’s diagnosis is made by documenting a delay in two domains of development, rather than in all domains, and because of that, the initial diagnosis of GDD may not necessarily reflect the actual severity of the NI status of the child (2). The initial diagnosis of GDD, however common it might be, may not actually persist as a cause for increasing need for hospitalizations.
Documented Disabilities
In the beginning of admissions, it was noted that 61.1% of the patients did not have a documented disability. However, an increasing number of patients have had their disabilities documented in later admission, and as a result, the number of patients without a documented disability has decreased to reach the lowest point of 32.3% by the fifth admission. Still, the overall number of admissions without a documented disability in all admission was relatively high (n=338, 53.2%). The diagnosis of GDD itself is considered a disability, and almost half of all admissions have had underlying GDD. Therefore, the other included conditions are most likely associated with many other forms of disabilities (23-26). As a result, it is fair to state that there is a major under-reporting of disabilities in children with underlying NI, which may lead to many consequences. Generally, people with disabilities are more likely to experience more health-affecting issues across multiple aspects of healthcare such as difficulty in acquisition of healthcare, having higher overall risk factors for many diseases, and being incapable of selfcare or being unable to afford the needed aid, along many other problems (27). When examining cases with documented disabilities, it was found that physical disability was the commonest amongst all forms of disabilities which were similarly reported in other studies (22, 24, 26, 28). In addition, it was noted that the number of patients with visual impairment was high and close to that of patients with physical disability in cases of hydrocephalus and HIE. In hydrocephalus, a possible cause for visual impairment is atrophy of the optic nerve (14, 15). On the other hand, the mechanism behind visual impairment in HIE is primarily asphyxia-related insult to the visual pathway and visual cortex, resulting in cortical visual impairment (29, 30).
Neurological Causes of Admission
The common causes for admission of children with underlying disabling NI are mostly neurological with seizures at the top, followed by hydrocephalus-related causes, and milestones delays (31). In our study, neurological causes that lead to admission were prevalent in almost all underlying NI, most noticeably with underlying hydrocephalus and HIE. The most common neurological condition that led to admission of patients with underlying NI was seizures. In patient with underlying congenital hydrocephalus developing seizures is a common complication, reaching up to approximately 50% (32, 33). The underlying mechanism of how hydrocephalus can cause seizure is controversial. Many authors reported a strong association between shunt insertion and seizure while others found no such correlation (34). The high occurrence of seizures in hydrocephalus is an undeniable fact. Seizure can also be associated with HIE, especially in the neonatal period, reaching approximately 50% (35, 36). Irrespective of the cause, children with seizures are often brought to a healthcare facility for workup or treatment where they are often hospitalized (37). The second highest neurological cause for admission after seizures was hydrocephalus-related complications. 84 out of 138 of the patients with underlying hydrocephalus have been admitted due to neurological causes, and 34 of those patients had VP shunt insertions or revisions, mostly due to complications and failure. VP shunts’ failure is not an uncommon occurrence (18) with an overall complication rate of VP shunt insertion was 35.76% (37). Some of the mentioned complications include shunt blockage (45.94%), shunt infection (16.21%), and shut migration (10.81%). One study has mentioned that 33 hydrocephalus patients had a total of 201 shut revisions (44). These findings can explain the high admissions count in patients with hydrocephalus, let alone the fact that hydrocephalus can also present with seizures.
Respiratory Causes of Admission
The second commonest group of causes that lead admission of children with underlying NI is conditions affecting the respiratory system (n=164, 25%). Leading that category are infections of the lower respiratory tract infections (n=112, 17.6%), mostly aspiration pneumonia. Aspiration pneumonia, as a single diagnosis, was more common than seizures. It was found that respiratory conditions were common in patients with underlying GDD, CP and HIE amongst other NI. Considering that HIE and CP are possible causes of GDD, it is reasonable to see the same array of medical problems in all three conditions. It is known that GDD is a major cause of respiratory problems in children (38). The care required for such patients in order to prevent respiratory complications is extensive (39). Therefore, the chances of contracting a lower respiratory infection in patients diagnosed with GDD or any of its causative pathologies are not slim. An example is the clear pathophysiology of aspiration pneumonia in CP. Reflux and aspiration, combined with poor cough and airway clearance, in addition to respiratory muscle weakness and possible chest wall deformities can lead to recurrent chest infections (40). The diagnosis of aspiration pneumonia carried higher morbidity and is more associated with worse medical complications and outcomes and extended hospital stays (41). Additionally, there was a significant relationship between having a respiratory cause for admission and the main rout of feeding. It was found that a higher fraction of patients on NGT and GT feeding were more likely to acquire a respiratory infection. This was more evident in patients using NGT than in patients on GT feeding. This finding was proven by previous studies that favored the use of GT over NGT in reducing the risk of pneumonia (42). This all proves the hypothesis that children with underlying NI are more likely to develop pneumonia, requiring hospitalization.
Gastrointestinal Causes of Admission
Gastrointestinal causes of admission in children with NI were the third most common. It was noted that gastroenteritis (n=22, 3.4%) was the most common presenting gastrointestinal disease, followed by gastroesophageal reflux disease (n=15, 2.4%). High admission rates due to gastroenteritis are likely due to the common nature of the disease rather than NI being an actual risk factor. Hospitalization of children due to gastroenteritis can reach up to 10% of all emergency admissions (43, 44). Moreover. there was no studies found that can relate NI to an increased risk for acute gastroenteritis. When it comes to gastroesophageal reflux disease, one study found a strong relationship between having developmental disability and developing feeding problems (1). The study focused mainly on children with CP, autism and Down syndrome. It reported that 48% of developmentally disabled children had gastroesophageal reflux disease. It also proposed that the reason behind the development of gastroesophageal reflux disease in CP patients was the presence of moderate-to-severe widespread neuromotor dysfunction as hypothesized. As part of the management of gastroesophageal reflux disease and its complications, patients may undergo upper gastrointestinal endoscopy and fundoplication which requires hospital admission. In more severe cases, patients would be electively admitted for gastric tube insertion to avoid malnutrition and aspiration (45). Another study reported that there is no significant relationship between urgent admissions and any reflux parameter even with positive investigations in children that aspirate and children suffering from NI (34%), 15% of which having developmental delay (46). Meaning, neurologically impaired children do not have urgent admissions due to reflux alone, even if they aspirate. The cause for urgent hospitalization in such cases would be aspiration-related pneumonia, rather than aspiration itself. Despite that, this study shows a relationship between non-urgent admission with reflux and aspiration. This finding supports the hypothesis that children with NI have higher admission rates due to GER-related issues other than aspiration.
Our study limitation, before the implementation of an electronic medical record system and the use of the International Classification of Diseases coding system, the specific documentation of conditions was lacking and most cases of complications of a disease would not be explicitly documented. Furthermore, since the sample of this study is a non-probability convenience sample, it can be subject to selection bias. An example of which is the fact that all VP shunt complications would be documented as “hydrocephalus”. This has led to the ambiguity in data collection and interpretation. Therefore, rather than using the ICD-AM-10 codes, a grouping system for causes of admission was implemented for data analysis. Regarding the causative condition, there was an overlap with the underlying NI on the inclusion criteria as they were different in that they are an immediate cause for the admission in question, not an underlying condition but was written as so in the files. Moreover, having many later admissions with low patient number will lead to sample skewness as the data of patients who have more than a few admissions will persist while the majority’s data regresses, as they do not have as many admissions. An example of such skewness is the age of patients. In Table 1, there is a noticeable increase of the mean age of patients in the eighth and later admission. This means that the same patients are being admitted repeatedly at later ages. For these reasons, this discussion will focus primarily on the first 5-6 admissions for better representation of the targeted population.
Conclusion
In conclusion, we found that the leading causes of recurrent admission in children with NI were neurological, respiratory and gastrointestinal. The single most documented cause for admission was aspiration pneumonia, followed by seizures. There was a statistically significant relationship between the type of NI and the cause of admission. For a future direction, a multi-centered prospective cohort study with a larger sample is needed to identify other possible causes of admission. We recommend increasing the awareness amongst healthcare workers and caregivers of neurologically impaired and disabled children regarding these conditions in order to implement preventive measurements that may allow for a better quality of life for these children. That can be achieved by increasing vigilance towards children with NI and disabilities, using accurate documentation and better clinical description to allow better representation, and by driving more efforts towards modifying and individualizing health plans for each patient.
Acknowledgment
We would like to acknowledge the efforts of Dr. Maan Althobaiti in assisting with data collection, as well as the relentless efforts of the administrative staff of the medical records department of King Abdulaziz Medical City for their cooperation and assistance. We would like to also acknowledge the valuable insight.
Disclosure
Statement:
The authors declare no conflict of interest.
Funding:
None.
Ethical Consideration:
The study was approved by King Abdullah International Medical Research Center (KAIMRC) Ethical Board Committee with registration number: H-01-R-005. All methods were performed in accordance with the relevant guidelines and regulations of Declaration of Helsinki 1975.
Data Availability:
All data are presented within the paper.
Author Contribution:
SB, HA, RA and SA contributed to conceptualizing, drafting, data collecting and analysis of the data. RA, SA and MK took part in drafting, proofreading and English editing.
