Volume 5, Issue 1
January 2025
External Fixation of a Compound Comminuted Calcaneal Fracture in a Young Diabetic Adult Male: A Case Report
Elsiddig Ali Elsiddig Ahmed
DOI: http://dx.doi.org/10.52533/JOHS.2025.50112
Keywords: Calcaneal fracture, External fixation, Sanders type 4, Diabetes mellitus, Minimally invasive surgery
Background: Compound calcaneal fractures, especially Sanders Type 4, are complex injuries caused by high-impact trauma. Diabetes mellitus adds further complications, including impaired wound healing and higher infection risk. Restoring calcaneal alignment while preserving soft tissue is critical. Therefore, external fixation offers a minimally invasive method to stabilize fractures and reduce complications, making it a suitable choice for high-risk patients.
Case presentation: A 33-year-old male construction worker with type 2 diabetes mellitus fell from a height of seven meters. He presented with an open Gustilo Type II calcaneal fracture. Examination revealed swelling, ecchymosis, and a widened heel, with intact neurovascular status. Imaging confirmed a comminuted Sanders Type 4 fracture with posterior facet displacement. Emergency management included advanced trauma life support protocol, antibiotics, and wound care. Definitive treatment involved external fixation using ligamentotaxis and osteotaxis principles. Pins were placed under fluoroscopic guidance to restore height, alignment, and subtalar congruity. Postoperative care included strict wound monitoring and a structured rehabilitation plan. Follow-ups showed no infection, malalignment, or delayed healing.
Conclusion: External fixation is effective for managing complex calcaneal fractures in diabetic patients. It provides stable fracture alignment while minimizing soft tissue damage. This approach is a safe alternative to traditional methods in high-risk patients. Further research is needed to refine techniques and improve outcomes in similar cases.
Introduction
Calcaneal fractures, which affect the heel bone, present a complex orthopedic challenge due to the bone's intricate anatomy and its critical function in weight-bearing (1). They are rare complex injuries that account for 1–2% of all fractures and represent 60% of tarsal bone injuries (2). They are typically caused by high-energy trauma, such as falls from height, and often result in significant functional impairment. Other causes can be motor vehicle accidents, sport-related injuries, and crush injuries. There are certain risk factors that can lead to calcaneal fractures, such as osteoporosis, occupational hazards, age, gender and certain medical conditions (1).
Calcaneus fractures can be intraarticular, extraarticular, open vs closed fractures, or stress fractures (1). The Gustilo classification is a system used to categorize open fractures and is divided into 3 types based on the severity of soft tissue injury (3). Displaced intra-articular fractures occur when bone fragments in the joint space are misaligned. These fractures often affect the subtalar joint, which plays a key role in foot movement and weight distribution. The Sanders classification system is typically used to categorize these fractures based on the severity of joint involvement. It is based on Computed Tomography (CT) scans, and it has 4 types, with Type IV seen in our case (highly fragmented, poor outcomes may need fusion or external fixation) (4).
Diagnosis can be made with either an X-ray, CT scan or MRI. Non-contrast CT scan is the gold standard for traumatic calcaneus injuries. X-ray is usually the initial diagnostic tool, and MRI can be used to diagnose calcaneus fractures, it is typically done in specific cases where there are soft tissue injuries (5). Treatment for calcaneus fractures can be surgical or non-surgical, depending on various factors. Generally, fracture management involves reduction (realigning the bones) and fixation (stabilizing the bones). Non-displaced fractures can heal with rest and immobilization, usually with a cast. Some fractures are treated with closed reduction, repositioning the bone under anesthesia without surgery. If this fails or the fracture is severe, surgery may be required (1). Surgical options include closed reduction with internal fixation, open reduction with internal fixation (ORIF), or external fixation, depending on the severity and location of the injury.
The extensile lateral approach (ELA) remains widely used for surgical management. It provides excellent visualization for fracture reduction but is associated with significant soft tissue complications (6). Wound infection and necrosis are common, particularly in patients with comorbidities like diabetes mellitus. The adverse effects of diabetes can lead to nervous, vascular, and immune system issues that damage the musculoskeletal system, especially if the foot is involved. Diabetic foot is one of the frequent and severe issues encountered by orthopedic surgeons (7). These risks have led to increased interest in alternative techniques. Less invasive approaches, including percutaneous fixation and the sinus tarsi approach (STA), aim to reduce soft tissue damage while achieving adequate fracture stabilization (8). External fixation, used alongside ligamentotaxis principles, offers another effective option. It allows for stabilization and three-dimensional reconstruction of the calcaneus while limiting surgical trauma to surrounding tissues (9). This technique is particularly useful in high-risk patients with severe comminution or compromised wound healing (10).
This case report describes the management of a 33-year-old diabetic male who sustained a compound comminuted calcaneal fracture after a fall from height. The report focuses on surgical management, including external fixation and postoperative care. It illustrates the application of modern techniques in managing high-risk patients, such as diabetics to optimize outcomes and minimize complications.
Case presentation
On December 12, 2024, a 33-year-old male construction worker with type 2 diabetes mellitus, was brought to the Emergency Department (ED) of Prince Mutaib Bin Abdul Aziz Hospital following an accidental fall from approximately seven meters height, landing directly on his right foot. The patient sustained this high-impact trauma during his work, resulting in acute right foot pain, swelling, and inability to bear weight on it. His medical history was significant only for diabetes mellitus, with no hypertension or smoking history.
Initial assessment revealed a conscious, oriented patient with Glasgow Coma Scale of 15/15, blood pressure 117/69 mmHg, and pulse rate 82 beats per minute. Systemic examination indicated no abnormal findings. Local examination of the right foot demonstrated a Gustilo type II compound fracture with a 3-cm puncture wound on the medial calcaneal aspect. Clinical findings included significant foot swelling, ecchymosis, and a characteristically shortened and widened heel. Testing range of motion revealed limited plantarflexion, eversion, and inversion. Neurovascular examination confirmed palpable femoral, popliteal, posterior tibial, and dorsalis pedis pulses, with preserved motor and sensory function. Compartment assessment revealed soft compartments without any signs of vascular compromise.
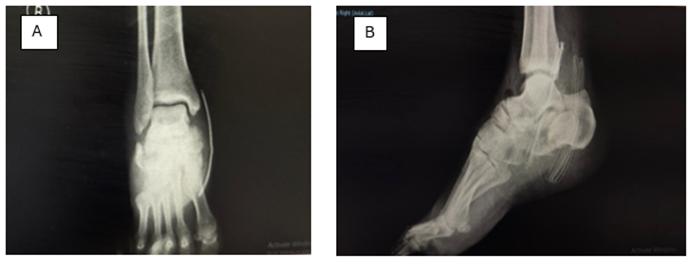
Radiographic evaluation by X-ray showed multiple pathological findings including a double-density sign, subtalar incongruity, partial separation of the facet from the sustentaculum, and calcaneal shortening with varus tuberosity deformity. Additional findings included a decreased Böhler's angle, posterior facet collapse, and increased angle of Gissane (Figure 1). Computed tomography (CT) with 2-3 mm cuts revealed a Sanders Type 4 classification with posterior and middle facet displacement, characterized by three or more primary fracture lines and articular displacement exceeding 2 mm, indicating severe comminution (Figure 2).
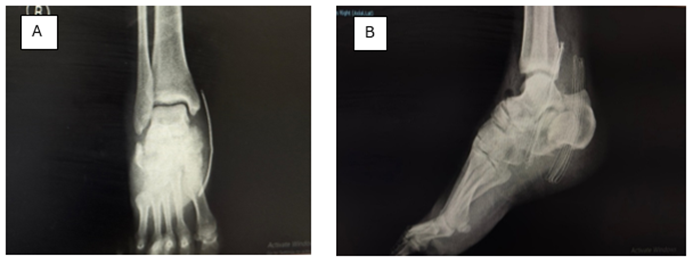
Figure 1: X-rays of the patient’s right foot, anteroposterior (A) and lateral (B) views.
Findings: double-density sign, subtalar incongruity, partial separation of facet from sustentaculum, calcaneal shortening, varus tuberosity deformity, decreased Böhler's angle, collapse of the posterior facet and increased Gissane angle.
Findings: A severely comminuted calcaneal fracture with posterior and middle facet displacement, tuberosity fragment malalignment, and significant articular incongruity. Sanders type 4 classification is confirmed by three or more primary fracture lines with >2mm articular displacement.
Initial management in the ED followed advanced trauma life support protocol and included administration of analgesics, intravenous fluid resuscitation, prophylactic antibiotics, tetanus prophylaxis, and sterile dressing application to the puncture wound. Following admission, the treatment plan involved continued antibiotic therapy, pain management, thromboprophylaxis with enoxaparin, foot elevation, and surgical planning for debridement and external fixation.
On December 13, 2024, the patient underwent planned surgical intervention, under general anesthesia and strict sterile conditions. It started with thorough debridement of the compound fracture site. All necrotic tissue, devitalized soft tissue, scabs, and loose hematomas were evacuated. The wound was thoroughly irrigated, with preservation of bone fragments. Then the external fixation procedure was conducted using ligamentotaxis and osteotaxis principles for fracture reduction.
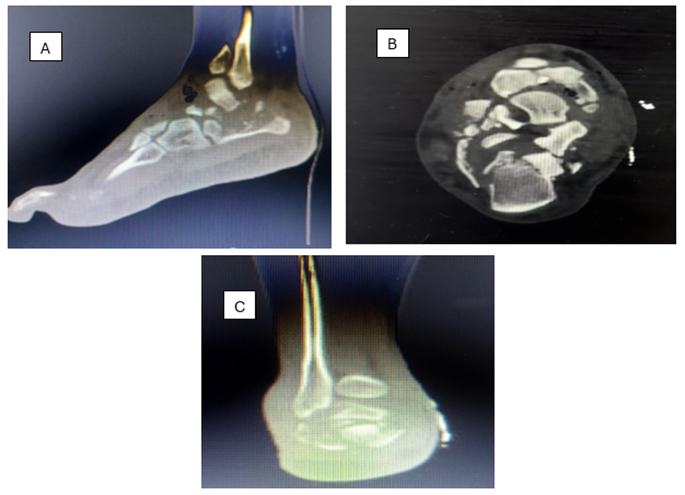
Figure 2: CT images of the patient’s right foot, sagittal (A), axial (B), and coronal (C) views.
External fixation began with the placement of two parallel 4-mm diameter pins into the calcaneal tuberosity. These pins were strategically positioned in the most posterior, non-fractured area of the tuberosity, behind the depressed thalamic fragment, as guided by preoperative CT imaging. The pins were inserted from inside-out, perpendicular to the calcaneal longitudinal axis, with careful attention to avoid damaging the inferior calcaneal nerve. The insertion plane was selected based on the separation line between the calcaneal tuberosity and thalamic fragment, ensuring complete visualization of the subtalar joint on lateral fluoroscopic imaging.
The construct was expanded by inserting two additional 4-mm pins into the anteromedial aspect of the tibia, aligned with the bone longitudinal axis. This was followed by placing two 3-mm pins in the distal metaphyseal region of the fifth metatarsal, oriented along its major axis in an anteromedial position. These components were then connected to create a triangular construct on the lateral aspect of the foot (Figure 3). The pin-jaw unit allowed manipulation to correct rear foot varus and restore calcaneal height and length. All adjustments were verified through real-time fluoroscopic imaging, taking care to avoid over-correction into valgus.

Figure 3: The triangular construct of the external fixator on the lateral aspect of the patient’s right foot.
Post-operative management consisted of scheduled wound assessments and dressing changes on days 1, 2, 3, 5, and 7, accompanied by thromboprophylaxis with enoxaparin. The rehabilitation protocol prescribed non-weight bearing for 6-8 weeks, with ankle range-of-motion exercises initiated 2 weeks after the operation. The patient was discharged on December 19, 2024, with a structured follow-up schedule involving weekly visits for the initial 6 weeks, followed by biweekly appointments for the subsequent 6 weeks, and monthly follow-up planned for 6 months. External fixator removal is expected between 8-12 weeks post-operatively, depending on clinical and radiological progress. At initial follow-ups, the patient showed good recovery, with no signs of infection or malalignment (Figure 4). There were no complications on subsequent follow-ups.

Figure 4: Post-operative X-ray of the patient’s foot (lateral view) showing no signs of malalignment.
Discussion
Calcaneal fractures caused by high-energy trauma, such as falls from height, present significant management challenges. Axial forces compress the calcaneus against the talus, leading to severe comminution and disruption of the subtalar joint (9). In this case, the Sanders type 4 fracture represents the most complex category, characterized by multiple fracture lines and extensive posterior facet involvement. The direct axial load altered the Bohler’s and Gissane angles, which are critical for evaluating fracture severity and guiding reduction. The open nature of the fracture further increased the risk of infection and healing complications.
Diabetes mellitus complicates fracture management by decreasing microvascular perfusion, delaying wound healing, and increasing infection risk. These challenges are pronounced in open fractures and require strict glycemic control and careful wound management (8, 10). In this case, integration of diabetic foot care principles into the treatment plan minimized infection risks and promoted wound healing. This approach, coupled with regular monitoring, ensured that diabetes did not exacerbate the complications typically associated with complex calcaneal fractures.
Various treatment modalities exist for calcaneal fractures. The ELA approach offers excellent visualization for reduction and fixation but carries high complication rates, particularly in high-risk patients. Wound dehiscence and infections can occur in up to 24% of cases, making ELA unsuitable for diabetic patients with open fractures (11). STA minimizes soft tissue disruption and reduces wound complications. However, it is less effective in treating severe comminution occurring in Sanders Type 4 fractures (12). Percutaneous fixation is a minimally invasive option but ineffective in complex fractures requiring precise anatomical reconstruction (13). External fixation, used in this case, effectively balances fracture stability and soft tissue preservation. By applying ligamentotaxis principles, the fixator restored calcaneal height and alignment, confirmed through fluoroscopic imaging. This method avoided the large incisions associated with ELA and provided sufficient flexibility to adjust alignment gradually, reducing the risk of malunion.
The case series reported by Farrell et al. demonstrated the efficacy of temporizing external fixation followed by staged ORIF through STA, improving Bohler’s angle with no infections (14). This strategy highlights the value of external fixation for early stabilization, although our approach differed by exclusively using external fixation, avoiding ORIF entirely. This was particularly advantageous for our diabetic patient, where additional surgical trauma was avoided.
Heinig et al. presented a case of Sanders type 4 fracture managed with a circular external fixator and a calcaneal osteotomy, reporting full ambulation within five months. Their use of a bioactive glass to fill bone loss and prevent infection could be potential adjunctive measures for managing bone defects (15), though these were not required in our case. The similarity lies in the reliance on external fixation for stabilization while preserving soft tissue integrity.
Hou et al. explored circular external fixators combined with locking plates in managing severe intra-articular fractures. Their results demonstrated significant improvement in Bohler’s and Gissane’s angles, with relatively low complications (9). This aligns with the outcomes observed in our case, where external fixation effectively restored alignment without additional internal fixation. Unlike the combination approach used by Hou et al., our exclusive use of external fixation avoided the risks associated with ELA, further reducing the likelihood of soft tissue complications.
Hammond et al. evaluated percutaneous fixation in high-risk populations, including diabetics and smokers. Their study reported no wound complications but observed difficulty in achieving anatomical reduction in Sanders Type 4 fractures (10). Similarly, Syros et al. investigated STA in high-risk patients, observing a wound complication rate of 2.1% in patients surgically treated within 1 week, and they also noticed 15.2% in patients surgically treated after delaying the surgery for 2 weeks, despite it being a minimally invasive technique (16). In contrast, this case achieved successful reduction and alignment using external fixation, with no infection or soft tissue complications, indicating its suitability for complex fractures in high-risk patients.
The timing of surgical intervention is critical in reducing complications and improving outcomes, especially in high-risk patients. In the Hammond series, percutaneous fixation, conducted within an average of 6.7 days from injury, was associated with favorable outcomes (10). Similarly, Syros et al. pointed to the importance of early STA intervention to minimize infection risks (16). In the current case, surgical intervention was performed on the day following admission, ensuring timely debridement and stabilization. This prompt approach likely contributed to the successful management of the fracture and soft tissue injury.
Functional outcomes vary by fracture type and treatment modality. Percutaneous fixation studies report American Orthopaedic Foot and Ankle Society scores ranging from 73 to 96 (out of 100), with better results in less comminuted fractures (10). STA achieves comparable functional outcomes to ELA with fewer wound complications, but long-term risks of subtalar arthritis persist if reduction is inadequate (16). In this case, external fixation successfully restored calcaneal height and alignment, with early results indicating a favorable trajectory for functional recovery.
Further studies should evaluate hybrid fixation methods that integrate external and internal techniques to improve outcomes in complex calcaneal fractures. Long-term research focusing on diabetic patients is essential to refine surgical strategies and postoperative care. Advances in external fixation approach may improve precision and streamline use, offering better solutions for high-risk patients.
This case demonstrates the effectiveness of external fixation in treating complex calcaneal fractures in diabetic patients. It achieves a balance between maintaining fracture stability and minimizing soft tissue damage, addressing the unique challenges caused by high-impact injuries.
Conclusion
This case highlights the effectiveness of external fixation in treating complex, open Sanders type 4 calcaneal fractures, particularly in high-risk patients such as diabetics. By applying ligamentotaxis and osteotaxis principles, the approach restored calcaneal alignment and subtalar congruity while preserving soft tissue integrity. This method minimized the risks associated with large incisions and internal fixation, which are particularly problematic in diabetic patients prone to wound complications and infections. Early surgical intervention and precise pin placement under fluoroscopic guidance were critical in achieving a stable construct and avoiding malunion.
Disclosures
Author contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
An informed consent was provided by the patient to include the data anonymously. Furthermore, the local ethical committee of Prince Mutaib Bin Abdul Aziz Hospital approved the publication of the case.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The author declares no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.