Volume 5, Issue 1
January 2025
Evaluating the Efficacy of SGLT2 Inhibitors in Preventing Diabetic Kidney Disease
Samar Abed Alharbi, Abdullah Mushabab Alqahtani, Shahad Nasser Alnasser, Ghadeer Lafi Alfuhaydi, Raghad Adel Alrowithi, Fawzia Ayedh Asiri, Ahmed Ammar Almutairi
DOI: http://dx.doi.org/10.52533/JOHS.2025.50111
Keywords: SGLT2 inhibitors, Diabetic kidney disease, Renal outcomes, Diabetes management
Diabetic kidney disease (DKD) remains one of the leading causes of morbidity and mortality in diabetic patients, and there are very few therapeutic options that can halt its progression. SGLT2 inhibitors were developed to lower glucose, but they have also demonstrated highly significant renal and cardiovascular benefits independent of their glucose-lowering effects. This article summarizes, based on evidence from clinical trials and meta-analysis, the efficacy of SGLT2 inhibitors in preventing diabetic kidney disease. EMPA-REG OUTCOME, CANVAS, and DAPA-CKD trials have suggested that SGLT2 inhibitors drugs have renal benefit effects. This review also discusses safety profiles, emphasizing that a proper balance exists between efficacy and adverse effects, with a low but manageable risk for genitourinary infections. The current guidelines advocate the supplementation of SGLT2 inhibitors to usual care in patients with DKD, especially those who are at high risk for cardiovascular or renal outcomes. In summary, SGLT2 inhibitors represent a paradigm shift in the management of DKD, supported by robust evidence from trials that have clearly demonstrated their benefits for renal outcomes. The advantages may be related to several processes, such as decreased intraglomerular pressure, enhanced hemodynamic stability, and decreased renal inflammation. Crucially, renal advantages are also present in both diabetic and nondiabetic patients, underlining their wide range of applications in nephroprotection. Future studies should be directed at long-term and large-scale clinical trials assessing the efficacy and mechanisms of SGLT2 inhibitors for preventing DKD. Per the current guidelines, patients with DKD at high risk for renal consequences should be administered SGLT2 inhibitors in addition to their regular therapy.
Introduction
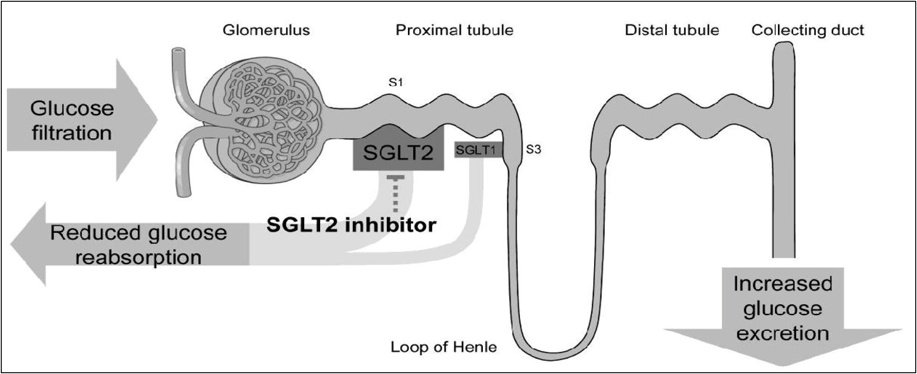
Diabetic kidney disease (DKD) is one of the most serious and common complications of diabetes and greatly increases morbidity and mortality. It is characterized by progressive renal dysfunction and often leads to end-stage renal disease (ESRD), which requires renal replacement therapy. DKD is expected to rise due to an increased prevalence of diabetes worldwide, highlighting the urgent need for efficient preventive and treatment measures that are quite necessary. Early intervention is important since DKD can be managed to slow or even halt its progression (1). Sodium-glucose cotransporter-2 (SGLT2) inhibitors, originally developed to treat type II diabetes, have become a subject of great interest because of their possible benefits associated with renal protection, especially in the setting of DKD. This drug acts by inhibiting SGLT2 proteins in the proximal renal tubules, reducing glucose reabsorption and increasing glucose excretion through the urine (2).
Besides its role in managing hyperglycemia, this mechanism further reduces intraglomerular pressure, increases natriuresis, and decreases renal inflammation, collectively contributing to renal protection. Several large-scale clinical trials in recent years, including the CREDENCE, CANVAS, and EMPA-REG OUTCOME trials, have demonstrated that SGLT2 inhibitors significantly reduce the risk of kidney disease progression, albuminuria, and other markers of renal dysfunction in individuals with diabetes (3, 4). These findings raise the possibility that SGLT2 inhibitors, such as empagliflozin, dapagliflozin, canagliflozin, ertugliflozin, and bexaglifloxin represent a new approach to preventing DKD and could exert benefits beyond reduction of blood glucose. In addition to that, SGLT2 inhibitors have shown potential for reducing the adverse renal outcomes typically associated with diabetes (5).
This review aims to provide an unbiased analysis of the efficacy of SGLT2 inhibitors in halting the progression of diabetic kidney damage. It focuses on long-term outcomes, clinical trials involving the drug class, mechanisms of action underlying its effects, and potential benefits for patients across various stages of DKD. Understanding the impact of SGLT2 inhibitors on kidney health in diabetic patients is crucial for optimizing treatment plans and improving patient outcomes, particularly in clinical practice (3).
Methodology
This review applied a broad peer-reviewed article search from the Cochrane Library, PubMed, and Scopus databases in an effort to find key studies and clinical and meta-analyses trials that discuss the evaluation of SGLT2 inhibitors in the prevention of DKD. The following keywords were used: SGLT2 inhibitors, diabetic kidney disease, and the efficacy of SGLT2 inhibitors, focusing on articles published up to 2024. Particular attention was given to highly influential trials, including EMPA-REG OUTCOME, CANVAS, and DAPA-CKD. The findings were synthesized to assess the mechanism of action, efficacy, clinical application, and safety profile of SGLT2 inhibitors.
Discussion
SGLT2 inhibitors primarily act by inhibiting the SGLT2 protein, which is located in the proximal convoluted tubule, in which most of the blood glucose reabsorption occurs along the functional unit of the kidney (nephrons). In the kidney proximal tubule, SGLT2 transporters normally reabsorb approximately 90% of the blood glucose filtered by the renal glomeruli (6).
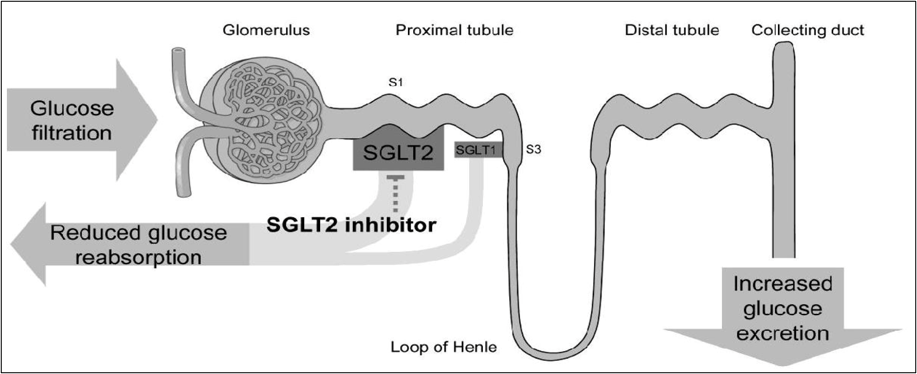
Figure 1: Mechanism of action of SGLT2 inhibitors*
*Adapted from the background document of the Food and Drug Administration on Dapagliflozin (7).
SGLT2 inhibitors render glucose unreabsorbable by inhibiting this transporter, which in turn increases the excretion of urine glucose and leads to a reduction of the blood glucose level.
Inhibition of SGLT2 has additional important hemodynamic consequences aside from its renal protective role, including osmotic diuresis caused by increased glucose excretion, which lowers the blood pressure and decreases plasma volume. Consequently, this may contribute to a reduction in DKD progression (8). The osmotic diuresis from the increased glucose excretion induced by SGLT2 inhibitors reduces blood pressure and plasma volume (9). Consequently, it is anticipated that intraglomerular pressure would decrease, which is a desirable outcome. Besides, SGLT2 inhibitors are thought to reduce oxidative stress and renal inflammation, two key parameters implicated in the development of DKD. They may also improve endothelial function of the kidney through a series of molecular pathways, reduce the production of pro-inflammatory cytokines, and enhance the activity of antioxidant enzymes (6).
By modifying renal hemodynamics and decreasing glomerular filtration pressure, SGLT2 inhibitors also have the additional role of albuminuria “which is a key marker of renal disease in diabetic patients (10). Thus, SGLT2 inhibitors could represent a novel treatment strategy for DKD that combines the benefits of diuresis, glucosuria, and improved renal blood dynamics. Several large clinical studies have confirmed its myriad benefits beyond blood glucose control in protecting both kidneys and heart from DKD (11-13).
Research has substantiated the benefits of SGLT2 inhibitors in precluding or delaying the progression of diabetic conditions, though findings from various trials have also raised some concerns. Crucial studies have demonstrated that the advantages of these medications extend beyond their renal effects, encompassing significant cardiovascular benefits that are integral to managing the comorbidities commonly associated with diabetes and kidney disease (14).
The EMPA-REG OUTCOME study was a landmark trial conducted to assess the cardiovascular and renal effects of empagliflozin in patients with type II diabetes and established cardiovascular diseases. Although the primary objective of the study was to evaluate cardiovascular outcomes, several secondary analyses revealed significant improvements in renal parameters (15, 16). Notably, the study demonstrated a 39% reduction in the relative risk of developing microalbuminuria and a 32% overall reduction in the risk of renal disease progression.
The EMPA-REG OUTCOME trial remains one of the most critical studies regarding the cardiovascular and renal benefits of empagliflozin in patients with T2D and established CVD. While renal outcomes were primarily observed in secondary analyses, the study’s main objective was to evaluate cardiovascular events (17). Findings from the trial indicated that treatment with empagliflozin reduced the risk of a sustained decline in eGFR by 32% and decreased the progression to microalbuminuria by 39%. If these results hold, they suggest that empagliflozin may significantly slow the progression of kidney disease in high-risk patients (18, 19).
The CANVAS study evaluated the effectiveness of the SGLT2 inhibitor canagliflozin in patients with type 2 diabetes at high risk for cardiovascular events. The study reported that canagliflozin significantly reduced kidney-related events, including a composite endpoint of a sustained ≥40% reduction in eGFR, end-stage renal disease, or death from renal causes (20). Notably, the composite kidney endpoint was reduced by 40%, further reinforcing the renal protective effects attributed to SGLT2 inhibitors (21).
The DAPA-CKD trial was a phase 3 pivotal study aimed at evaluating the efficacy of dapagliflozin, an SGLT2 inhibitor, in reducing adverse renal and cardiovascular events in patients with chronic kidney disease (CKD), with or without type II diabetes (22). Conducted across 386 centers in 21 countries, the study enrolled 4,304 participants with an eGFR range of 25–75 mL/min/1.73 m2 and significant albuminuria. All participants were receiving the maximum tolerated doses of renin-angiotensin system inhibitors unless contraindicated.
The primary outcome, a composite of sustained eGFR decline of 50% or more, progression to end-stage renal disease (ESRD), or death from renal or cardiovascular causes, was significantly reduced in the dapagliflozin group (23). The hazard ratio for this outcome was 0.61, indicating a 39% lower risk compared to the placebo group. Secondary outcomes, including rates of hospitalization for CKD and heart failure, as well as overall mortality, were also significantly improved. These results underscored the renal and cardiovascular protection offered by dapagliflozin in patients with CKD, regardless of diabetic status, further affirming its efficacy in slowing CKD progression and reducing mortality. This trial has significantly influenced treatment guidelines, establishing SGLT2 inhibitors as critical tools in the management of CKD and DKD, beyond their role in glycemic control (24).
In addition, another seminal study investigated the effects of the SGLT2 inhibitor canagliflozin on cardiovascular and renal outcomes in patients with type 2 diabetes and CKD (25). The trial demonstrated that canagliflozin significantly reduced the risk of overall mortality, serum creatinine doubling, and the composite outcome of ESRD by 30%. These findings further highlight the transformative impact of SGLT2 inhibitors in managing diabetes and chronic kidney disease.
These benefits were consistent across various subgroups, regardless of glycemic index or baseline kidney function (26). The CREDENCE study firmly established SGLT2 inhibitors as a cornerstone treatment, marking a paradigm shift in managing CKD in patients with T2D. Its findings emphasized personalized therapy, balancing glycemic control objectives with cardiovascular and kidney protection. The study demonstrated that canagliflozin could slow the progression of CKD beyond glucose management, likely through mechanisms such as reducing inflammation and intraglomerular pressure (27). However, it also highlighted safety concerns, including a slightly increased risk of vaginal infections and diabetic ketoacidosis, underscoring the need for careful patient selection and monitoring (28).
The CREDENCE study positioned SGLT2 inhibitors as a transformative treatment, reshaping approaches to CKD management in T2D patients. Its findings provide the foundation for personalized treatment strategies that address both cardiovascular and renal protection while achieving glycemic control goals (27, 29).
Additionally, data from smaller trials and observational studies have confirmed the renal benefits of SGLT2 inhibitors. These drugs have been associated with reductions in albuminuria levels and improvements in kidney function, particularly in patients with early diabetic kidney disease (30). Furthermore, meta-analysis results suggest that SGLT2 inhibitors are linked to a reduced risk of hospitalization for heart failure and diabetic kidney disease, as well as lower overall mortality in patients with DKD (17, 31).
Adverse effects of SGLT2 in individuals with diabetic kidney disease
Now, SGLT2 inhibitors have begun to gain major recognition for their profound impact on kidney function and cardiovascular health, hence they are in very frequent application in DKD treatment. These are effective drugs to decrease albumin levels and retard the disease process.
However, it is important to consider the side effects of SGLT2 inhibitors (32). The most commonly reported adverse effects include genital fungal infections, particularly in uncontrolled diabetic patients with higher urine glucose levels. Urinary tract infections, though less frequent, are also noted as potential side effects. Volume depletion and low blood pressure are additional concerns, especially in patients with hypotensive tendencies or those on diuretics, necessitating close monitoring of fluid status.
In rare cases, severe renal impairment may lead to complications such as hyperkalemia or hypomagnesemia, which could further complicate treatment. One of the most serious adverse effects is an increased risk of diabetic ketoacidosis (DKA), specifically euglycemic DKA, which can occur even when blood glucose levels are normal. This rare condition requires prompt recognition and treatment and may be exacerbated by fasting, acute infections, or significant reductions in insulin dosing. Gastrointestinal disturbances, including nausea and abdominal discomfort, are also common.
Some studies have suggested a potential association between canagliflozin and an increased risk of amputations and bone fractures, though this remains a subject of ongoing investigation.
Overall, while SGLT2 inhibitors offer significant benefits for diabetic kidney disease patients, their use requires careful patient selection, close follow-up, and proactive management of side effects to ensure maximum benefit and safety. Further research is necessary to understand their long-term effects and to refine clinical protocols (33).
Limitations and safety considerations of SGLT2 inhibitors
Although the role of SGLT2 inhibitors in slowing the progression of DKD has been well-established, several challenges remain regarding their administration. One significant issue is the variability in patient response to these medications. While many patients experience substantial benefits, some show only minimal responses, particularly those with advanced renal impairment or comorbid health conditions.
Moreover, the side effects mentioned earlier, such as urinary tract infections, fungal infections, and dehydration, are particularly concerning in elderly patients or those with a history of low blood pressure (34). These adverse effects necessitate careful patient selection and monitoring to ensure safe and effective use.
Finally, comprehensive long-term safety data are still needed to fully assess the risks associated with chronic use of SGLT2 inhibitors, especially in patients with severe renal impairment. Such data are essential for guiding treatment decisions and optimizing the use of SGLT2 inhibitors in diverse patient populations (35).
Conclusion
SGLT2 inhibitors represent a significant advancement in the management of DKD, offering strong evidence of effectiveness in slowing disease progression through albuminuria reduction and improving cardiovascular outcomes. These benefits suggest they could be first-line treatment for patients with type 2 diabetes and early to moderate DKD or those at high risk of progression. However, challenges remain, including patient response variability, potential side effects such as volume depletion and genital infections, and concerns about affordability. A patient-centered approach is essential, considering individual risk factors, renal function, and possible adverse effects. Further research is needed to optimize SGLT2 inhibitor use, particularly in combination with renin-angiotensin-aldosterone system inhibitors, and to gather long-term safety and efficacy data in advanced kidney disease, non-diabetic populations, and high-risk groups. Addressing these gaps will help unlock the full potential of SGLT2 inhibitors in improving clinical outcomes and quality of life for patients worldwide.
Disclosure
Declaration
The authors declare no conflict of interest.
Funding
None.
Ethical Considerations
Not applicable.
Data Availability
All data is available within the manuscript.
Author Contribution
All authors contributed equally to the conceptualization, data collection, data analysis and writing of the paper.