Volume 4, Issue 12
December 2024
Mini Dental Implants Retaining Overdenture on Old Patients with Atrophic Ridges
Haitham Mohammed Binhuraib, Sahar Khalil Alhajrassi, Manal Bediwi, Osamah Abdullah Basudan, Ahmed Alfarsi, Jawad Ahmad
DOI: http://dx.doi.org/10.52533/JOHS.2024.41260
Keywords: mini dental implants, narrow diameter implants, survival rate, success rate, patient satisfaction
Mini dental implants (MDIs) utilized to conserve overdentures may provide adequate function and increase quality of life in elderly patients. They are particularly beneficial for patients with severe ridge atrophy or limited space for standard implants, offering a feasible treatment option and are associated with high success rates. This literature review discusses the success rate, survival rate, patient satisfaction, and the uses of MDIs when used for definitive prosthodontic treatment. An average success rate of 93% for MDIs and 96% for narrow-diameter implants. Both mini and narrow-diameter implants are viable options for retaining mandibular overdentures, demonstrating satisfactory clinical outcomes. Survival rates for MDIs ranged from 91.17% to 100%. Overdentures supported by locator attachments had higher survival rates compared to traditional implants. MDIs significantly enhance patient satisfaction, especially in treating mandibular overdentures. They provide stability, eliminate adhesive use, and reduce discomfort. MDIs are less invasive, reducing the need for additional surgeries and discomfort, making them an effective, economical, and patient-preferred solution for patients with mandibular edentulism.
Introduction
Tooth loss is a prevalent condition among elderly individuals, often resulting from cumulative oral diseases such as periodontitis, dental caries, and traumatic injuries. The loss of teeth, particularly in the context of atrophic alveolar ridges, presents significant challenges in dental rehabilitation. Atrophic ridges are defined by extensive resorption of the alveolar bone following tooth loss, resulting in a significant reduction in both bone height and width. Severely atrophic ridges present considerable challenges in clinical practice, as they further diminish denture retention, support, and overall stability, thereby posing a significant obstacle to the successful rehabilitation with complete denture prostheses (1). These challenges become particularly pronounced in elderly patients, who often face additional age-related factors such as reduced healing capacity, systemic health issues, and decreased manual dexterity.
Mini dental implants (MDIs) have emerged as a transformative solution to replace missing teeth as well as to support complete overdentures (2). MDIs are narrow-diameter implants, typically less than 3 mm in diameter, designed to provide a minimally invasive, cost-effective alternative to standard implants. The latest classification defines them as one-piece category 1 narrow implants with a diameter ranging from 1.8 to 2.5 mm. Their reduced diameter allows them to be placed in areas with limited bone volume without the need for extensive grafting procedures. This feature makes MDIs particularly suitable for elderly patients with atrophic ridges, who may not be ideal candidates for complex surgical interventions. Additionally, MDIs can support overdentures, which offer superior retention, stability, and functionality compared to conventional dentures. This is particularly beneficial for frail and elderly patients, especially those with bimaxillary atrophy, for whom a minimally invasive treatment may be appropriate (3). Minimally invasive treatment can be instituted to minimize physiological stress and costs. Oral implant rehabilitations are well-established as a reliable medium- and long-term solution for patients with partial or complete edentulism. Edentulous ridges significantly affect aesthetics and oral function, leading to diminished quality of life. Many patients rely on mandibular prostheses, which often face retention issues, causing discomfort. Implant-supported overdentures enhance patient satisfaction by providing improved stability and masticatory function. MDIs are associated with high success rates and reduced percutaneous exposure but require careful management of occlusal loads (4). They offer advantages such as ease of placement in narrow or wide ridges, simplified procedures, and the potential for immediate loading (5). The use of MDIs minimizes the need for extensive surgical procedures, thereby reducing patient morbidity and the operator's required experience. However, surgical interventions may still be necessary to address insufficient bone volume, which can carry risks, particularly for medically compromised or elderly patients. This has led to a growing interest in narrow-diameter implants as an alternative to more invasive treatments (6). The surgical placement of dental implants presents challenges when the available bone is insufficient for standard-width implants. Solutions for patients with narrow alveolar ridges include various surgical techniques such as ridge augmentation, vertical distraction osteogenesis, and ridge expansion, as well as the use of reduced-diameter implants. However, these reduced-diameter implants may not always be suitable for atrophic ridges, and patients may prefer to avoid additional surgeries. Management of edentulous mandibular patients using overdentures supported by two regular-size dental implants has proven to be an effective treatment option. However, the use of mini-diameter implants introduces a controversial alternative due to factors such as bone quality, financial constraints, and patients' surgical concerns. Mini diameter implants offer advantages including less invasive surgical options, such as flapless procedures and immediate loading, making them particularly suitable for medically compromised patients with limited bones. This literature review discusses the success rate, survival rate, patient satisfaction, and the uses of MDIs when used for definitive prosthodontic treatment.
Methods
An electronic search of literature enriched by hand searches was performed in PubMed and Google Scholar databases to identify suitable publications. The keywords used were: “mini dental implants” and “success rate,” “mini dental implants” and “survival rate,” “mini dental implants” and “atrophic ridge” and “knife-edge ridge,” “small-diameter implants” and “fixed survival rate” and “success rate,” “small-diameter implants,” and “knife-edge ridge,” and “atrophic ridge." Only clinical studies published from January 2000 through October 2024 were included. The review included studies of the following types: case reports, cross-sectional, cohort, randomized clinical trials, systematic reviews, and meta-analyses. Inclusion criteria were studies involving older patients who could not undergo invasive surgeries, papers directly relevant to the key terms, English-language studies, and those reporting implant diameters less than 3.5 mm. Exclusion criteria were studies involving pediatric patients, manufacturer-sponsored publications, mini-implants for orthodontic anchorage, and implant diameters greater than 3.5 mm.
Discussion
The use of MDIs to retain overdentures in elderly patients with atrophic ridges has gained substantial attention due to its effectiveness in improving oral function, esthetics, and patient satisfaction. This discussion evaluates the available evidence on the success rates, survival rates, and patient satisfaction of MDIs considering clinical, prosthetic, and patient-centered outcomes. A patient with an atrophic edentulous ridge was managed using 2.5-mm-diameter mini-implants that were immediately loaded, as illustrated in Figure 1, which demonstrates the clinical presentation and treatment approach
Success rate
Recent studies have highlighted the effectiveness of narrow-diameter and MDIs in supporting prostheses, particularly in the context of mandibular overdentures. Both mini and narrow implants showed adequate clinical behavior as overdenture retainers. Management of atrophic mandibular ridges with an MDI system is reported to be safe, as well as a highly successful rate procedure, and can be done in cases with poor bone quality as well (3). It gives the patient and the dentist access to a wide range of treatment options. According to a recent meta-analysis, NDIs exhibit better long-term predictability for retaining overdentures, with most studies adopting conventional loading protocols. According to a recent meta-analysis, NDIs exhibit better long-term predictability for retaining overdentures, with most studies adopting conventional loading protocols (7). Rosa A. et al. reported a success rate of 89% for narrow implants in their meta-analysis, with notably higher rates observed in studies with longer follow-up periods. These findings suggest that the longevity of implant function may improve with time and consistent monitoring. Furthermore, the study indicated that the success rates of MDIs are comparable to those of regular implants, provided that essential biomechanical principles are adhered to during placement.

Figure 1: The patient presented with an atrophic edentulous ridge that was treated with 2.5-mm-diameter mini implants and immediately loaded (3).
Interestingly, the findings also caution against the assumption that increasing the number of implants necessarily enhances overall success. Instead, excessive implant placement may increase patient morbidity without yielding proportional benefits (6). A systematic review and meta-analysis further reinforced these insights, revealing an average success rate of 93% for MDIs, which ranges from 84% to 100%, and a slightly higher average success rate of 96% for narrow-diameter implants, ranging from 85% to 100%. Also, long-term success rates for narrow-diameter implants were reported at 94% in studies with follow-up durations exceeding four years. These findings confirm that both MDIs and narrow diameter implants are viable options for retaining mandibular overdentures, demonstrating satisfactory clinical outcomes (7).
Historical data from Griffitts et al. corroborated these findings, showing a remarkable success rate of 97.4% for MDIs. The study highlighted their stability and financial advantages, making them a valuable adjunct for enhancing patient comfort and satisfaction (8). Additionally, a 2012 prospective cohort study by Šćepanović et al. demonstrated impressive outcomes with 100% overdenture success and 98.3% success for loaded implants among patients receiving four immediately loaded MDIs. Despite some intraoperative complications being observed, the overall results underscore the potential of these implants to provide effective and reliable solutions for edentulous patients transitioning from conventional complete dentures (9).
Figure 2 shows the load distribution in mandibular overdentures retained by MDIs under three scenarios: bilateral posterior, unilateral posterior, and anterior loading. It highlights the role of implant positioning in ensuring stability and functional efficiency (10).
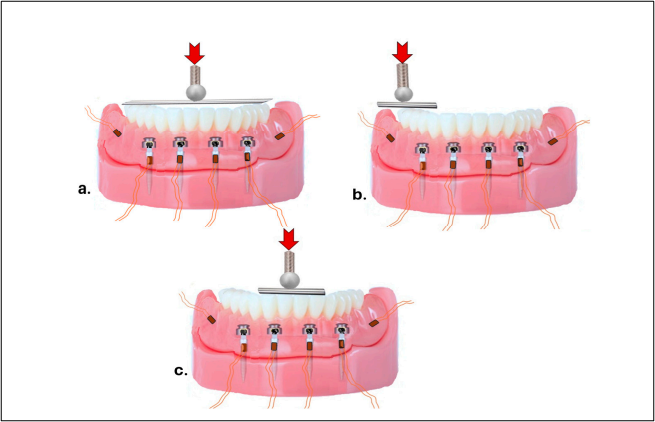
Figure 2: Schematic Representation of Load Distribution in Mandibular Overdentures Retained by MDIs.
Survival rate
Survival rate, often used interchangeably with success rate but measured by the physical presence of the implant in the oral cavity regardless of complications, has also been extensively studied. MDIs showed excellent survival rates in the short to medium term. Recent studies have demonstrated a high survival rate of 97.9% for mini-implants in mandibular overdentures, based on an analysis of 184 implants monitored over a 15-year period. These findings establish MDIs as a reliable choice for elderly patients. Of the implants evaluated, only five (2.5%) fractured, while three (1.52%) were removed due to instability, highlighting the long-term durability and success of this treatment modality (4). In addition, a one-year clinical trial aimed at enhancing the quality of life for complete denture wearers involved thirty participants, divided into two groups: one group received minimally invasive surgery while the other underwent standard treatment. The minimally invasive group achieved a 100% survival rate after one year and reported significant improvements in their dental health-related quality of life compared to those in the standard treatment group (11). These results underline the efficacy of minimally invasive approaches in enhancing patient outcomes and satisfaction. Further evidence of the reliability of mini-implants comes from a 10-year follow-up study that assessed the health of peri-implant tissues and bone areas. This study involved 20 patients with compromised mandibular ridges, all receiving 1.8 mm implants. Fourteen of these patients had a 100% survival rate for 56 implants after the decade-long follow-up, and the overall prosthesis survival rate was 93%. The findings concluded that one-piece mini-implants with O-ring attachments are particularly effective for patients with compromised mandibular ridges (12).
Another investigation compared early and immediate loading of MDIs, revealing cumulative survival rates of 96.7% for early loading and 91.7% for immediate loading, with an overall survival rate of 94.2% over three years. Both loading protocols demonstrated favorable clinical results and maintained healthy peri-implant tissue (13). Additionally, a study evaluating the stability and marginal bone levels of immediately loaded MDIs found a clinically acceptable bone level, with a stability rate of 98.3% after one year (14).
A systematic review analyzing the survival rates of MDIs indicated an overall survival rate of 98%. For studies with follow-up periods shorter than two years, the survival rate was 96%, while those with longer follow-ups reported a survival rate of 92%. This reinforces the reliability of mini-implants as effective retainers for mandibular overdentures (7). However, some cohort studies noted complications such as fractures near metal housings, which were resolved by reinforcing the overdentures, highlighting the importance of robust material design (9).
In a review of 41 studies on small-diameter implants, survival rates for MDIs ranged from 91.17% to 100% over follow-ups from four months to eight years. A critical six-month period was identified as a benchmark for stability, indicating that the risk of implant failure significantly decreases beyond these follow-ups (15). Research also showed a cumulative survival rate of 95.5% for implants placed in patients with severe residual ridge resorption, with few reported complications (16).
Recent findings indicated that overdentures supported by locator attachments had higher survival rates compared to those using traditional implants (6). Another study reported a mid-term survival rate of 92% for MDIs among a substantial number of patients. While these survival rates are encouraging, there were notable occurrences of prosthetic issues, such as fractures in denture bases, emphasizing the need for careful monitoring and maintenance of these restorations (17). Literature consistently supports the high efficacy and survival rates of MDIs in mandibular overdenture applications. The collective findings highlight the significance of implant design, loading strategies, and diligent patient management in optimizing outcomes and improving the quality of life for edentulous individuals.
Patient satisfaction
One of the most significant advantages of MDIs is the high level of patient satisfaction they provide. Elderly patients often report substantial improvements in comfort, masticatory efficiency, speech, and overall quality of life following the placement of MDI-retained overdentures. Unlike conventional dentures, which often suffer from poor retention and instability, MDI-supported overdentures provide enhanced stability, eliminating the need for adhesive use and reducing the risk of discomfort or denture movement. Studies have highlighted improvements in four key areas: speaking ability, chewing ability, comfort, and retention (Figure 3). Specifically, retention ratings surged from an average of 2.23 before treatment to an impressive 8.60 afterward, while scores for chewing ability rose from 2.79 to 9.00. Improvements in speaking ability and comfort were also notable, increasing from 3.50 to 8.00 and from 3.25 to 9.29, respectively. These findings emphasize the role of mini-implants in improving the quality of life for patients with edentulous mandibles, particularly in terms of both aesthetic and functional aspects (4).
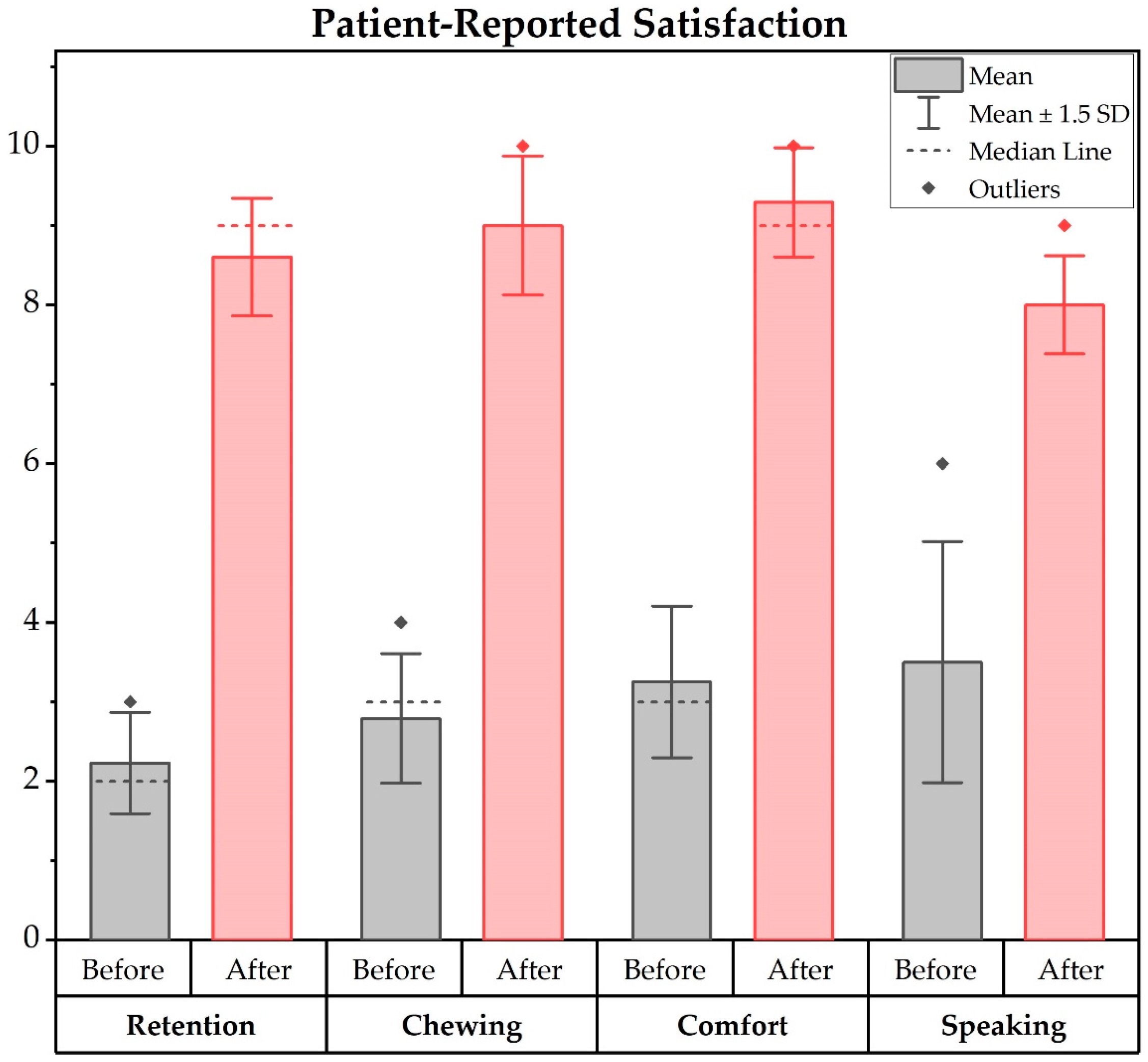
Figure 3: Patient-reported satisfaction domains before and after MDIs (4).
Recent studies and clinical trials have highlighted the advantages of MDIs in improving the quality of life and satisfaction among complete denture wearers. A one-year trial demonstrated that patients receiving minimally invasive surgery with two splinted mini-implants experienced significantly greater improvements in dental health-related quality of life compared to those fitted with standard complete dentures, emphasizing the efficacy of MDIs in enhancing patient satisfaction (11).
The less invasive nature of MDIs, which eliminates the need for additional surgeries like bone grafting, further adds to their appeal by reducing discomfort and complications (18). Patient-reported outcomes from follow-up questionnaires revealed remarkable improvements across critical criteria, including retention (from 1.7 to 9.6), chewing ability (from 2.3 to 9.3), speaking ability (from 5.3 to 8.5), and comfort (from 2.2 to 9.4), solidifying MDIs as an effective, economical, and patient-preferred solution for individuals with low denture tolerance (8).
Another relevant study involved thirty patients who received mandibular overdentures supported by four immediately loaded MDIs placed in the interforaminal region. Prior to this intervention, these patients used traditional complete dentures. The study found significant improvements in speech, chewing capability, stability, comfort, and overall quality of life following implant placement. These results contribute to the growing body of evidence suggesting that MDIs retained overdentures can serve as a valuable treatment for patients with mandibular edentulism (9).
Mini dental implant uses
Rosa et al research in 2023 highlighted the benefits of MDIs for patients with limited alveolar bone volume. They found that using MDIs with locators to support overdentures reduces bone loss and provides greater stability for the prosthesis (6). This is especially important for those with significant bone atrophy. Implant-supported overdentures distribute occlusal loads more evenly, preserve the vertical dimension of occlusion, minimize movement of the prosthesis, and reduce bone resorption. They also enhance tooth positioning and smile aesthetics. MDIs are less invasive, requiring quicker healing times and reducing the need for bone grafts. However, they may not be suitable for individuals with habits like teeth clenching or grinding (18). Overall, MDIs present a valuable solution for patients with narrow or atrophic alveolar ridges, as well as those who might be medically compromised and aren't ideal candidates for more conventional surgical procedures (5). A 2012 review by Gleiznys et al. further supported the use of small diameter and MDIs for narrow ridge tooth replacements. These implants stabilize removable dentures using multiple implants in both the mandible and maxilla, allowing patients to load a solid denture immediately. The procedure is quicker, causes less bleeding, and often eliminates the need for sutures, reducing postoperative pain and speeding up recovery (15).
While MDIs offer numerous advantages, their application in elderly patients with atrophic ridges is not without limitations. Potential complications include implant fracture, peri-implantitis, and loosening of the overdenture attachment. Additionally, systemic health conditions and reduced manual dexterity in elderly patients can impact on oral hygiene maintenance, increasing the risk of implant infections. Future studies are needed to establish standardized guidelines for MDI placement and management in geriatric patients, ensuring optimal outcomes.
Conclusion
Mini dental implants represent a successful and patient-satisfying option for dental rehabilitation in individuals with atrophic bone conditions; patients cannot withstand the surgeries and can't afford the cost of regular implants and surgeries. With an average success rate and survival rate over 90% of MDIs provide a valuable alternative to conventional implants, particularly in patients with limited bone volume. The high levels of patient satisfaction underscore the clinical benefits of this treatment modality. Continued research is essential to refine protocols, enhance outcomes, and expand the application of MDIs in diverse patient populations.
Disclosures
Author contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics statement
Not applicable.
Consent for publications
Not applicable.
Data availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not applicable.
