Volume 4, Issue 12
December 2024
Strategies for Managing Overcrowding in Emergency Departments
Abdu Dahesh Tohary, Sultan Owaid Alharthi, Nawal Saeed Asiri, Fatim Yahya Majrashi, Rawan Abdullah Khormi, Mohamed Ahmed Alhomrani
DOI: http://dx.doi.org/10.52533/JOHS.2024.41253
Keywords: Emergency department overcrowding, triage systems, resource optimization, predictive analytics, telemedicine
Emergency department (ED) overcrowding remains a critical global challenge, affecting patient safety, staff efficiency, and healthcare delivery. Key factors contributing to overcrowding include increasing patient visits, prolonged length of stay, and limited inpatient capacity. Innovative strategies are required to address these issues and optimize ED operations. Advances in patient flow and triage systems, resource allocation, and technology integration offer promising solutions. Streamlined triage systems, such as split-flow models and automated prioritization tools, improve efficiency by categorizing patients based on acuity and care requirements. These approaches significantly reduce waiting times and enhance throughput. Resource optimization strategies, including dynamic staffing models and task-shifting, ensure that healthcare professionals are allocated effectively, minimizing delays and preventing burnout. Predictive analytics further support these efforts by forecasting surges and enabling preemptive resource planning. Technology-driven solutions, such as telemedicine and artificial intelligence, have revolutionized ED operations. Virtual consultations reduce unnecessary visits, while automated triage systems ensure timely interventions. Real-time monitoring and location systems enhance workflow efficiency, enabling faster decision-making and improved patient tracking. While these innovations demonstrate significant potential, challenges such as financial constraints and workforce adaptation must be addressed for successful implementation. Investments in training, infrastructure, and stakeholder collaboration are critical to maximizing these advancements. By integrating these strategies, healthcare systems can mitigate overcrowding, improve patient outcomes, and build resilience in emergency care.
Introduction
Emergency department (ED) overcrowding is a pervasive and critical issue impacting healthcare systems globally. Studies indicate that more than 90% of EDs in developed countries report experiencing overcrowding at some point during the year, with significant consequences for patient care and system efficiency (1). In the United States, ED visits increased from approximately 119 million in 2006 to over 145 million in 2016, a trend that continues to rise annually (2). This surge in demand strains the resources and capacity of EDs, often leading to prolonged waiting times, delayed treatments, and adverse patient outcomes. Furthermore, one of the primary indicators of overcrowding is the length of stay (LOS) in EDs. On average, patients spend over 4 hours in EDs, with admitted patients experiencing even longer boarding times due to delayed transfers to inpatient wards (3). Research from the United Kingdom highlights that patients who board in EDs for more than 6 hours are at a 10% higher risk of mortality within 30 days compared to those who are promptly transferred (4). Such delays not only compromise patient safety but also contribute to staff burnout, reduced efficiency, and heightened operational costs.
The financial burden of ED overcrowding is equally concerning. It is estimated that hospitals lose approximately $4 billion annually in revenue due to increased LOS and decreased patient throughput in EDs (4). This financial strain is exacerbated by the growing prevalence of non-urgent visits. For instance, studies suggest that up to 30% of ED visits in the United States are classified as non-urgent, diverting critical resources away from patients with acute needs (3). In lower-income settings, the problem is compounded by inadequate infrastructure and limited access to primary care, further increasing reliance on EDs as the primary point of healthcare access. Globally, overcrowding is driven by several interrelated factors. Aging populations in many countries have led to an increase in patients with complex and chronic conditions, who require more time and resources during ED visits. Additionally, seasonal variations, such as flu outbreaks, can cause surges in patient numbers, overwhelming the system's capacity. For instance, during peak flu seasons, patient arrivals can increase by 20–30%, intensifying bottlenecks in triage and treatment (5). Efforts to address ED overcrowding must consider multifaceted solutions that span triage optimization, inpatient bed management, and the integration of technology. The role of predictive analytics, telemedicine, and workflow redesign has been increasingly recognized as pivotal in mitigating the impact of overcrowding. Nonetheless, disparities between countries, regions, and healthcare settings necessitate tailored approaches to ensure equitable and efficient access to emergency care services. This review aims to discuss strategies for managing overcrowding in emergency departments.
Review
ED overcrowding poses a multifaceted challenge requiring a combination of immediate and long-term strategies. A critical approach involves improving patient flow through streamlined triage systems and accelerated discharge processes. Studies have shown that implementing rapid triage models, which prioritize patients based on acuity, reduces waiting times and enhances overall efficiency (4). This approach is particularly effective when coupled with dedicated discharge lounges, where patients awaiting transportation or final paperwork can be moved to free up critical ED space.
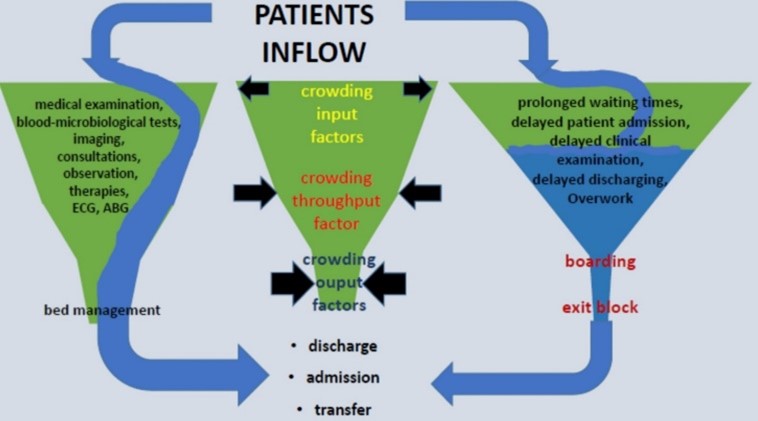
Another vital strategy involves addressing the root causes of boarding, such as delays in transferring admitted patients to inpatient wards. This issue is often linked to hospital-wide bed management inefficiencies. Optimizing inpatient workflows, expanding critical care capacity, and fostering better communication between departments can significantly alleviate boarding-related congestion. Recent evidence suggests that reducing boarding times correlates directly with improved patient outcomes, including lower mortality rates (3). Crowding in emergency departments can be visualized as a funnel: the wide opening represents the catchment area and input factors, such as the number of patients and their methods of presentation. The body of the funnel symbolizes the throughput processes, where patients are assessed and treated. The narrow neck of the funnel reflects the output factors, such as the availability of inpatient beds or discharge mechanisms. When crowding occurs, the wide opening expands to accommodate more patients, while the body and neck contract due to increased workload in the throughput processes or limitations in output capacity. This imbalance results in stagnation and congestion, disrupting the smooth flow of patient care (Figure 1) (6).
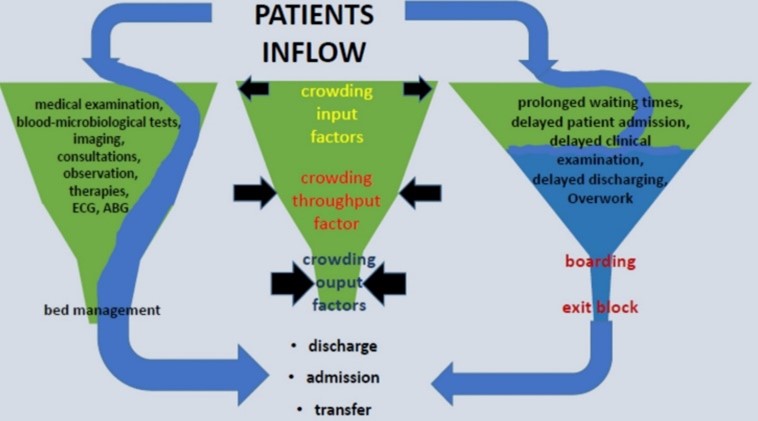
Figure 1: Patient flow in emergency department (6).
Technology integration offers additional promise in tackling overcrowding. For instance, predictive analytics and real-time monitoring systems can anticipate patient surges, enabling proactive resource allocation. While these solutions hold potential, their implementation requires robust investment and workforce training to ensure seamless adoption. Collaborative efforts across healthcare systems remain essential, emphasizing policy-level interventions alongside operational innovations to achieve sustainable outcomes.
Innovative Patient Flow and Triage Systems
Innovative patient flow and triage systems are fundamental to addressing the persistent challenges of ED overcrowding. Traditional models often struggle to cope with fluctuating demand and variability in patient acuity. Recent innovations aim to enhance efficiency by redesigning triage methods and introducing advanced technologies to streamline operations. One promising development involves the use of real-time decision support systems to predict hospital admissions at the time of triage. By employing machine learning algorithms, these systems analyze variables such as patient vitals and historical data to prioritize resources efficiently (5). This predictive approach reduces bottlenecks and ensures that critical cases are managed promptly while preventing unnecessary delays for lower-acuity patients.
Split-flow models, another notable innovation, segment patients based on the complexity of care required rather than using a linear, first-come-first-served approach. This method has shown significant success in reducing waiting times and enhancing throughput. A study evaluating split-flow implementation reported a 30% reduction in overall length of stay, benefiting both patients and healthcare providers (7). Such systems not only improve outcomes but also optimize workforce deployment, alleviating stress on medical staff. Digital triage applications have gained traction, particularly in urban settings where ED visits often surpass capacity. These applications enable pre-hospital assessment through patient self-reporting and video consultations, ensuring that individuals are directed to appropriate care pathways before arrival. An evaluation of one such system demonstrated a 25% decrease in non-urgent ED visits, underscoring its efficacy in mitigating overcrowding (8). Furthermore, digital platforms integrate seamlessly with hospital information systems, facilitating smoother transitions from triage to treatment.
Innovations also extend to physical and operational layouts within EDs. Modular triage zones, equipped with resources for immediate care, expedite decision-making and treatment initiation. These zones are particularly effective in managing surges during peak hours or disaster scenarios. Research highlights that modular setups reduce initial triage times by up to 40%, providing a scalable solution adaptable to diverse healthcare contexts (9). Despite these advancements, challenges remain in the widespread adoption of innovative systems. Financial constraints and resistance to change within institutions often hinder implementation. To overcome these barriers, it is essential to promote pilot programs that demonstrate measurable benefits, ensuring buy-in from stakeholders. Additionally, ongoing training and support are vital for healthcare professionals to adapt to novel technologies and workflows effectively. By integrating predictive analytics, digital tools, and restructured workflows, innovative triage and patient flow systems are transforming the way emergency care is delivered. These advancements not only address the immediate demands of overcrowding but also lay the foundation for a more responsive and efficient healthcare system.
Resource Optimization and Workforce Strategies
Effective resource optimization and workforce strategies are critical in managing the challenges faced by overcrowded EDs. By improving staffing models, deploying task-shifting techniques, and integrating innovative technologies, healthcare systems can enhance their operational efficiency and patient outcomes. Flexible staffing models have emerged as a key element in addressing fluctuating patient volumes. These models utilize predictive analytics to forecast peak times and dynamically adjust workforce allocation. For instance, integrating demand-based scheduling, where additional staff are deployed during anticipated surges, significantly reduces wait times and improves service delivery (10). This approach is particularly effective in urban EDs where patient volumes are unpredictable and often exceed capacity.
Task-shifting and skill-mix optimization represent another crucial strategy in resource management. By delegating specific tasks traditionally performed by physicians to trained nurses or physician assistants, healthcare systems can maximize resource utilization. A study demonstrated that implementing task-shifting protocols improved patient throughput by 20%, highlighting its potential to streamline workflows without compromising care quality (11). Such approaches also mitigate burnout among senior medical staff by redistributing workload more evenly across the team.
Incorporating artificial intelligence (AI) into ED operations provides additional opportunities for optimization. AI-powered tools assist in real-time decision-making, aiding in triage prioritization, bed allocation, and discharge planning. These systems enhance efficiency by minimizing human error and accelerating critical processes. One AI application reduced average length of stay in EDs by 15%, underscoring its role in achieving operational excellence (12). Moreover, AI facilitates continuous learning by analyzing trends and providing insights for ongoing improvement in resource allocation.
The integration of telemedicine has further revolutionized workforce strategies, particularly in rural and resource-constrained settings. Virtual consultations enable specialists to extend their expertise to multiple locations, ensuring that patients in remote areas receive timely care. Telemedicine platforms have been instrumental in reducing unnecessary hospital admissions by enabling real-time assessments and guiding appropriate management decisions (13). This approach not only alleviates pressure on urban EDs but also optimizes the distribution of limited healthcare resources. To support these advancements, healthcare systems must invest in training and development programs. Preparing staff to adapt to new technologies and workflows is essential for successful implementation. Additionally, fostering a culture of collaboration and communication within teams enhances the effectiveness of these strategies. Regular feedback mechanisms ensure that workforce optimization measures align with evolving needs and challenges, creating a resilient and adaptive healthcare environment.
Technology-Driven Solutions for Overcrowding
Technology-driven solutions are transforming how EDs address overcrowding. Advanced systems not only improve patient flow but also enhance the overall efficiency of care delivery through predictive analytics, real-time monitoring, and automated processes. Predictive analytics have become a cornerstone in preemptive resource management. By analyzing historical patient data and trends, hospitals can anticipate surges and allocate resources accordingly. For example, one study demonstrated that implementing predictive models reduced waiting times by 25% during peak hours, directly improving patient satisfaction and outcomes (14). These models also enable dynamic staff scheduling, ensuring that personnel are deployed effectively during high-demand periods.
Telemedicine has emerged as a critical tool, particularly in rural or resource-limited areas. Virtual consultations allow patients to connect with healthcare providers without the need to visit overcrowded EDs. This approach has significantly decreased non-urgent ED visits, as evidenced by a reduction of 30% in urban centers employing telehealth platforms (15). Additionally, telemedicine supports continuity of care by connecting patients to specialists, expediting treatment decisions, and reducing unnecessary admissions. Automated triage systems represent another innovative application. These systems leverage artificial intelligence to assess patients' conditions upon arrival and prioritize care based on severity. An evaluation of such systems showed a 40% improvement in triage efficiency, as well as a decline in errors associated with manual evaluations (16). By streamlining this critical step, automated triage not only reduces bottlenecks but also ensures timely intervention for high-acuity cases.
Real-time location systems (RTLS) have also been integrated into ED workflows to optimize patient tracking and resource utilization. These systems provide precise data on patient movement and bed availability, enabling healthcare providers to make informed decisions rapidly. RTLS implementation in one hospital led to a 15% increase in patient throughput, illustrating its potential to alleviate overcrowding (17). Moreover, these systems allow administrators to identify inefficiencies and adjust protocols dynamically. As these technologies are adopted, healthcare systems face challenges in integration and staff training. Continuous education programs and robust infrastructure investments are necessary to ensure seamless implementation. By addressing these barriers, hospitals can maximize the benefits of technology-driven solutions and enhance their capacity to deliver high-quality, efficient care.
Conclusion
In addressing emergency department overcrowding, a multifaceted approach combining innovative triage systems, resource optimization strategies, and technology-driven solutions is essential. These interventions not only improve patient flow and outcomes but also alleviate systemic inefficiencies. Investments in staff training and infrastructure are crucial to maximize these advancements. By fostering collaboration and leveraging technology, healthcare systems can create sustainable, patient-centered emergency care environments
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical consideration
Non applicable.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.