Volume 4, Issue 12
December 2024
Advancements in Wound Care Nursing: A Review of Innovative Dressings and Techniques
Ayat Saeed Alzain, Ibrahim Abdulrahman Althobaiti, Hamed Break Aljameeli, Afrah Reda Albahrani, Samah Hajie Alrizq, Suad Othman Alghamdi
DOI: http://dx.doi.org/10.52533/JOHS.2024.41250
Keywords: wound, nurse, healing, dressing, technique
Wound healing involves a carefully orchestrated series of stages, overseen by cellular, humoral, and molecular processes. Although this complex progression unfolds organically, it can be enhanced and hastened by employing diverse dressing methods, products, and active substances. Demonstrably, adept wound care can forestall issues linked to persistent non-healing wounds, and the use of topical treatments has markedly elevated the chances of survival for individuals with substantial chronic wounds and burns. Nurses hold a pivotal position in wound care, and their grasp of fundamental wound management principles is anticipated to significantly impact the quality of wound treatment. Nurses offer accessible, cost-efficient, evidence-based, safe, and effective care. Therefore, studying innovative techniques and dressings for wound care is crucial in nursing practice as innovations in wound care can lead to better outcomes for patients, including faster healing, reduced pain, and decreased risk of infection. By staying abreast of the latest advancements, nurses can provide more effective care and improve the overall patient experience. This review aims to examine the evidence presented in current literature concerning the ramifications of employing novel wound care dressings and techniques in nursing practice. In recent years, advancements in wound dressings have emerged, introducing novel alternatives such as combinations of diverse polymers and the integration of nanotechnology to produce superior materials while ensuring an optimal healing environment. Progress in hydrogel fabrication, coupled with advancements in nanotechnology, holds promise for the development of innovative and versatile technologies in the realm of wound dressing and wound repair. Additionally, more innovative dressings are also being introduced in practice to further promote wound healing and enhance patient outcomes.
Introduction
Any disruption of the integrity of living tissue might be considered a wound. Preserving skin integrity and the ability to adequate wound healing are critical conditions for healthy survival. The process of wound healing involves a cascade of events aimed at restoring skin integrity (1). Wounds impose a significant economic burden on health and social care providers, additionally impacting the quality of life of patients. Chronic wound management is challenging, and to achieve optimal outcomes for patients, it is recommended that the individuals involved in their care and treatment have sufficient expertise and abilities (2). Effective management of the wounds is essential as wounds may not heal as expected, especially for patients with comorbidities and chronic conditions. Complications arise along the route, and they can have serious repercussions for both the patient and the health-care system (3).
Wounds pose an increasing healthcare challenge attributed to the aging demographic. Nurses hold a pivotal position in wound care, and their grasp of fundamental wound management principles is anticipated to significantly impact the quality of wound treatment (4). Compared to normal practice, chronic wound care provided by specialized nurses improves results in terms of wound healing, repair and regeneration, therapy time, and readmission rate (5). Nurses play a central role in ensuring optimal patient outcomes, positive experiences, and efficient resource utilization for individuals with wounds. In the practical realm, wound care often falls under the leadership of nurses. As such, nurses must make informed decisions regarding treatments in collaboration with their patients. However, navigating the myriad of available treatments and dressing options in wound care can be complex. In such situations, it is beneficial to reflect on fundamental principles and recognize that evidence-based practice in nursing encompasses more than just the best research evidence. It also incorporates patient preferences and experiences, as well as the expertise and knowledge of the nurse, to ensure the delivery of the most effective care (6). Based on findings from several studies, almost 70%-80% of wound patients are treated in the community, with community nurses serving as the primary providers. Managing wounds is frequently the most essential use of their time (3).
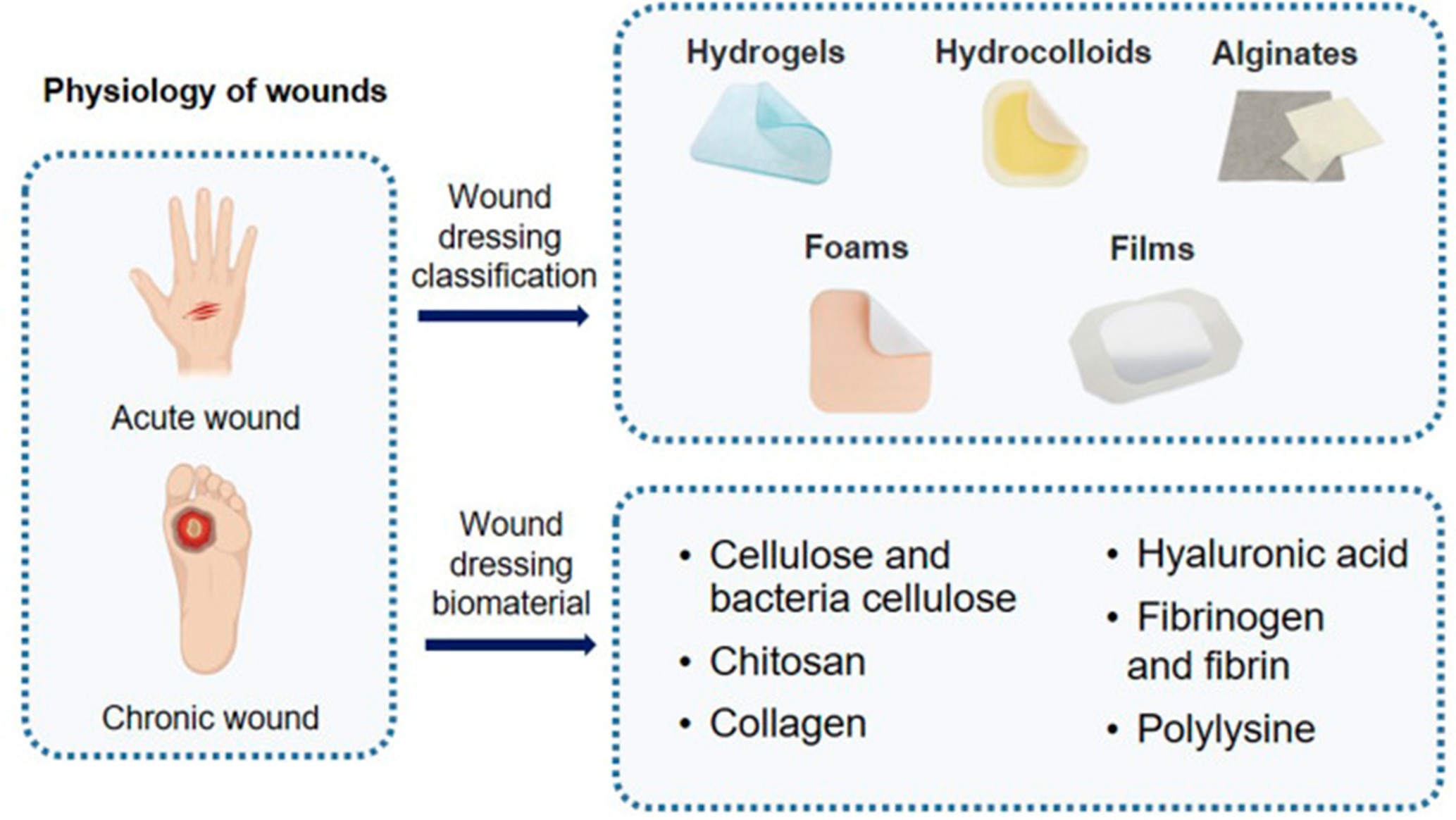
Numerous technologies have been developed to tackle the complexities encountered in the management of wounds, with a focus on topical therapies or dressings. Topical treatments like sterile saline, cadexomer iodine, hypochlorous acid, and superoxidized solutions are frequently used. The array of dressing options includes traditional cotton gauze, acrylics, honey alginates, hydrofibers, and hydrocolloids. Silver-infused dressings mainly target reducing microbial growth, providing temporary advantages in wound recovery, which warrants deeper exploration into metals' function in this context. Furthermore, recent encouraging experimental discoveries, like sprayable biodegradable substances, indicate continuous progress in this domain (7). Various dressing classifications on the basis of wounds are illustrated in Figure 1.
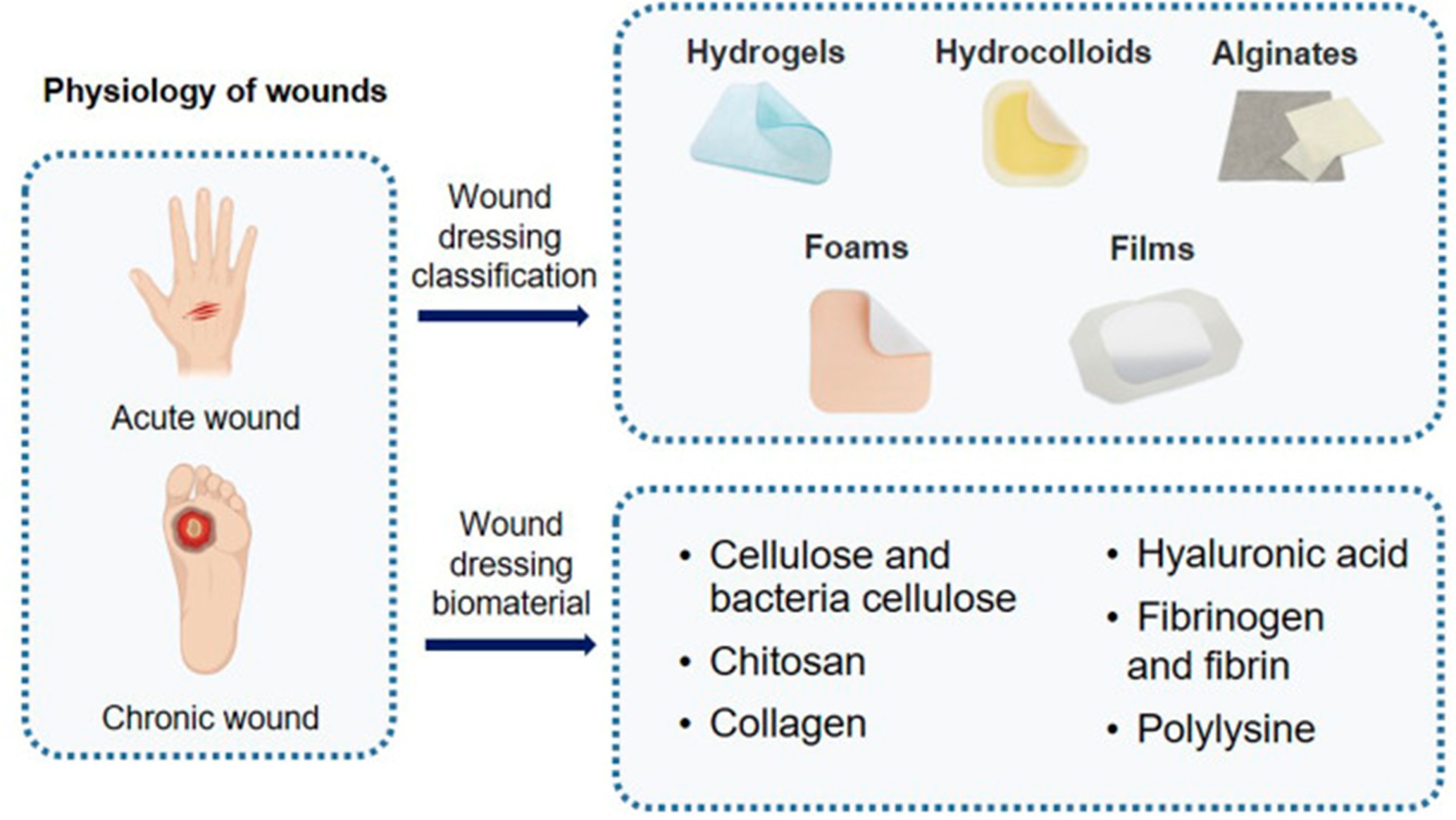
Figure 1: Diverse wound dressing materials employed in practice for acute and chronic wounds (8)
Studies in the literature demonstrate that nurses offer accessible, cost-efficient, evidence-based, safe, and effective care. They work jointly within a healthcare team. Nurse practitioners can evaluate and treat wounds, manage a patient's care, and refer to specialists as needed. Nurse practitioners can serve as patient care coordinators in both acute and community settings. Nurses play critical roles as consultants, educators, and researchers in multidisciplinary wound care teams. Nurses worldwide offer wound care in a variety of contexts, including hospital emergency rooms, long-term care homes, military, urology clinics, primary care, and communities (9). Therefore, studying innovative techniques and dressings for wound care is crucial in nursing practice as innovations in wound care can lead to better outcomes for patients, including faster healing, reduced pain, and decreased risk of infection. By staying abreast of the latest advancements, nurses can provide more effective care and improve the overall patient experience. Moreover, as patient populations change and medical conditions evolve, new challenges in wound care emerge. Innovative techniques and dressings help nurses adapt to these changes and provide tailored care that meets the evolving needs of patients. Hence, through this review, our objective is to examine the evidence presented in current literature concerning the ramifications of employing novel wound care dressings and techniques in wound care nursing. The outcomes of this investigation have the potential to augment the understanding of nurses operating within this field, thereby facilitating the enhancement of practices aimed at achieving optimal patient outcomes.
Methodology
A comprehensive literature search in the PubMed, Science Direct and Cochrane databases utilizing the medical topic headings (MeSH) and relevant keywords such as ‘wound’, ‘management’, ‘care’, ‘chronic wound’, ‘nurses’, ‘novel techniques’, ‘strategies’, ‘dressing’ and a combination of all available related terms were performed on May 16, 2024. All relevant peer-reviewed articles involving human subjects, and those available in the English language were included. Using the reference lists of the previously mentioned studies as a starting point, a manual search for publications was conducted through Google Scholar to avoid missing any potential studies. There were no limitations on date, publication type, and participant age.
Discussion
The ongoing discussion within nursing education revolves around two primary approaches to wound dressings: aseptic technique and the wound field concept. The aseptic technique involves a hands-off method aimed at promoting healing and minimizing infection risk by preventing microorganisms on hands, surfaces, and equipment. It has long been considered the standard practice, but its effectiveness in reducing surgical site infections is under debate. In both acute care and community settings, the wound field concept is proposed as a viable alternative to aseptic technique. This approach acknowledges wounds as inherently non-sterile environments, where the presence of contaminants from the patient and the wound itself does not necessarily worsen infection. Only external items introduced onto the wound surface are seen as potential sources of infection. Although some researchers argue that dressing practices have traditionally been guided by rituals rather than scientific principles (10).
Another area of debate within wound care concerns the optimal timing for removing dressings during the postoperative phase. There is uncertainty regarding whether it is necessary to keep an incision covered with a dressing beyond the initial 48 hours, or if bathing or showering could negatively impact wound healing. While there is evidence indicating that early exposure of acute wounds may elevate the risk of contamination and surgical site infections, some studies indicate that prolonging the duration of dressing application offers minimal advantages. Currently, clinical recommendations typically advise maintaining surgical dressings for up to 48 hours following surgery (10).
The criteria for the ideal dressing is its ability to maintain a moist environment, manage excess exudate, potentially possess antimicrobial properties, facilitate autolytic debridement, prevent bacterial contamination, be hypoallergenic, minimize pain, accommodate support needs, allow easy application and removal, provide thermal insulation, and be cost-effective. Recently, Hawthorne expanded on these qualities, highlighting the importance of preventing dehydration and scab formation, promoting oxygen permeability, sterilizability, mechanical protection, non-toxicity, anatomical conformity, tear resistance, soil resistance, non-flammability, consistent properties across different environmental conditions, long shelf life, compactness, and compatibility with medications (11) (12).
The evidence supporting the efficacy of moisture-retentive dressings is expanding. Optimal selection of these dressings should be based on the specific characteristics of the wound in relation to the properties of the dressing. For instance, superficial wounds may benefit from films, hydrocolloids, or polymer membrane dressings (PMD), while wounds with eschar may require hydrogels, hydrocolloids, or PMDs. Exudative wounds might be best managed with calcium alginates, hydrofibers, foams, or PMDs, whereas granulating wounds could benefit from hydrocolloids, foams, or PMDs. Wounds with slough might require protease-lowering dressings, hydrogels, or hydrocolloids. Deep or tunneling wounds may benefit from alginates, hydrofibers, or hydrogels, while infected or colonized wounds might be treated with silver and iodide-based dressings. Polymer membrane dressings are transforming dressing technology, offering versatility for application on various wound types. Recent advancements have integrated nanotechnology into dressings, allowing customization in wound management based on data provided by the dressing. It is anticipated that smart dressings incorporating such technologies will become more widely accessible for clinical use in the coming years (13).
Novel dressings and techniques employed in nursing practice for wound care
Various dressings utilized in practice for wound care nursing are briefly discussed below.
Hydrocolloids
Hydrocolloid dressings are effective for treating wounds with low to moderate exudate levels, granulated or necrotic wounds, as well as different types of acute wounds such as partial and full-thickness burns, surgical or postsurgical wounds in pediatric patients. These dressings consist of a hydrophilic and self-adhesive colloid granule covered with an external waterproof polyurethane film. Typically, they utilize gelatin, pectin, and carboxymethyl cellulose as materials for the colloid granules. They come in various shapes, sizes, and thicknesses to accommodate different wound types and sizes. The outer polyurethane layer acts as a barrier against bacteria, foreign particles, and environmental factors. Notably, hydrocolloid dressings exhibit high fluid absorption capacity while maintaining water vapor impermeability, fostering a moist wound healing environment. Additionally, their impermeability to oxygen promotes epithelialization and collagen synthesis, lowers wound exudate pH, thereby reducing bacterial proliferation. They facilitate autolytic debridement, preventing contamination, and often eliminate the need for secondary dressings (8). The structure of hydrocolloids is depicted in Figure 2.
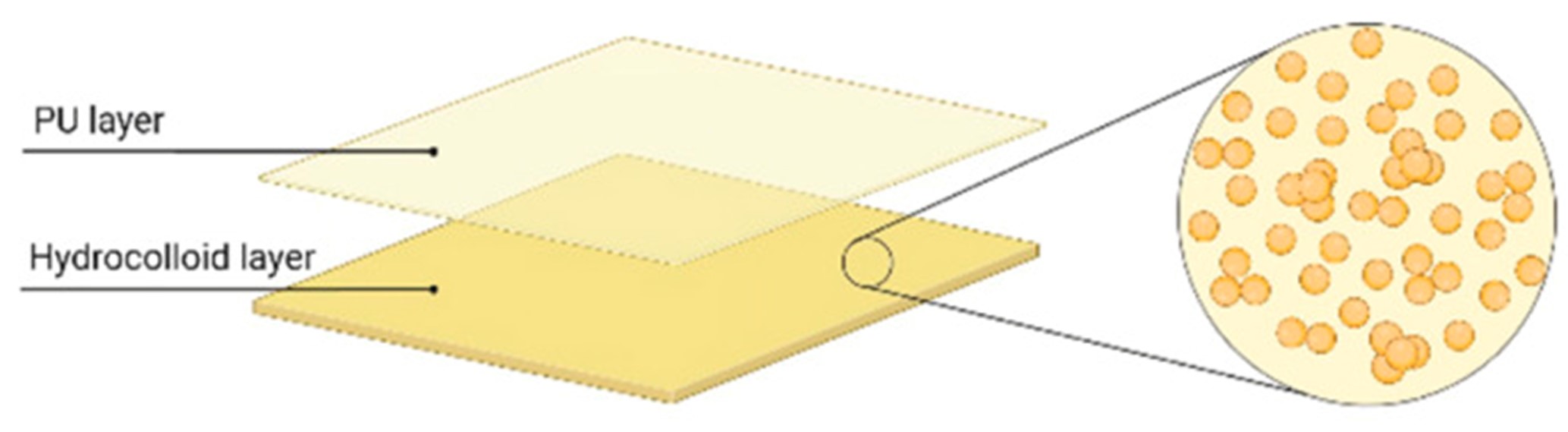
Figure 2: Internal structure of hydrocolloid dressing (8)
Nano-technology based dressings
The emergence of nanotechnology-based platforms has sparked considerable interest, particularly in biomedical and pharmaceutical domains, aiming to prevent or treat diseases, including wound management. Apart from nanoparticles, nanotechnology-based delivery systems encompass nanofibers, hydrogels, hydrocolloids, and more recently, nanohybrids, which combine various nanotechnological approaches. When materials are reduced to a nanoscale, their surface area and surface area-to-volume ratio undergo significant augmentation, resulting in enhanced physicochemical properties. Consequently, nanomaterials can play a role in wound healing by facilitating the carriage and delivery of therapeutic agents to the wound site or by virtue of their intrinsic characteristics (14). Nanoparticles represent a breakthrough in drug delivery of biocompatible agents, heralding a new era in wound healing dressings that prioritize non-antigenicity, resistance to shear stress, and gas exchange permeability. Several products have emerged from nanomaterials, aiming to develop practical wound healing solutions. Numerous studies have identified and characterized diverse nanomaterials and nanoproducts for wound healing. Electrospinning of natural and synthetic materials yields fine products that can be combined with other wound healing compounds and herbal remedies. Many of these produced nanomaterials exhibit significant efficacy in experimental wound healing models and hold potential for commercial utilization (15).
Stimulus-responsive dressings
Due to rapid progress in nanotechnology, many antibacterial dressings with responsive characteristics have emerged. These dressings integrate photothermal, photodynamic, or analogous treatments. Photothermal therapy harnesses the photothermal properties of substances such as graphene and polydopamine nanoparticles, transforming absorbed light into heat energy. This heat energy disrupts bacterial membranes, culminating in bacterial death. Meanwhile, photodynamic therapy demonstrates considerable promise in eradicating pathogenic bacteria by generating excessive reactive oxygen species (16). In the foreseeable future, hydrogel-based dressings responsive to stimuli hold promise for finely regulating wound healing processes. When coupled with a compact sensor system, these dressings could enable tailored therapeutic approaches. It's noteworthy that intelligent hydrogels combined with sensors are envisioned to provide real-time insights into the wound healing process. Given the dynamic changes in various processes and parameters during wound healing, real-time monitoring becomes crucial, challenging the development of a dressing that can effectively address the evolving needs of the entire healing trajectory. Moreover, the integration of other functional ingredients such as hemostatic, conductive, or adhesive materials is poised to significantly advance potential clinical applications (17). The concept of this smart wound dressing is represented in Figure 3.
Anti-bacterial agent containing dressings
Wound dressings containing antimicrobial compounds have recently emerged as effective methods for reducing wound bacterial colonization and infection, hence improving the healing process (19). The antimicrobial efficacy of dressings can also be attained by incorporating diverse antimicrobial agents, encompassing metal ions like zinc, iron, and silver ions, metal nanoparticles such as silver and gold nanoparticles, antibiotics for example vancomycin, and other antimicrobial compounds. Nevertheless, some antimicrobial agents may induce significant biological toxicity. For instance, vancomycin has been linked to nephrotoxicity and can provoke acute interstitial nephritis at elevated concentrations. Hence, concerted efforts are necessary to mitigate the biological toxicity of antimicrobial agents and precisely regulate their release (20, 21). Consensus exists within guidelines advocating for the utilization of topical antimicrobials as a preventive measure against infection, with many recommending the application of dressings containing silver in various situations. Nonetheless, there is presently no universally recommended topical antimicrobial agent suitable for all clinical contexts. There is a need for the formulation of more uniform recommendations to establish standardized clinical practices (22).

Figure 3: The concept smart wound dressing (18)
Enzyme-based debridement dressings
Managing deep second-degree burn injuries presents considerable challenges due to the extensive tissue necrosis involved. The natural resolution or detachment of this necrotic tissue typically takes two to three weeks, leaving a vulnerable period during which infections can exacerbate the wounds. While current dressings have improved abilities to absorb necrotic tissue and prevent infections, they lack the capacity to actively dissolve it. Bromelain has shown significant effectiveness in dissolving necrotic tissue, promoting spontaneous healing and managing scars after enzymatic debridement of deep second-degree burns. Integrating bromelain into burn wound dressings has demonstrated anti-infective and anti-inflammatory properties, significantly aiding the healing process and reducing inflammation in such wounds. Thus, combining bromelain for continuous necrotic tissue dissolution with antibacterial agents within a multifunctional dressing may offer improved effectiveness in treating deep second-degree burn injuries (23, 24).
Hemostatic dressings
Severe injuries can cause extensive skin damage, deep tissue wounds, and vascular trauma, resulting in significant bleeding that hampers wound healing and increases infection risks. The ability of dressings to absorb water is closely tied to their hydrophilic nature. Materials with high water absorption can extract moisture from the blood, increasing blood viscosity and promoting platelet aggregation and clotting. Silk fibroin contains amino acids with hydrophilic groups such as lysine, histidine, and arginine. Silk fibroin nanofibers exhibit exceptional hemostatic properties due to their small pore size and extensive specific surface area (16). Hemostatic materials serve to halt bleeding through various mechanisms. For instance, traditional options like gauze achieve hemostasis through physical compression, often applied using pressure wraps. Hemostatic sponges, functioning as efficient absorbents, swell upon absorbing local blood, leading to localized compression. Polyurethane sponges, utilized as nasal tamponades, also facilitate local compression. Additionally, several hemostatic materials activate hemostatic pathways within the human body via diverse mechanisms. For instance, chitosan sponges promote hemostasis by stimulating platelet activation and aggregation, leveraging the negative charges on the chitosan surface. Concurrently, the sponge's absorbent nature enhances the local concentration of platelets and coagulation factors at the wound site, thereby promoting the coagulation cascade. Furthermore, hemostatic materials can be laden with hemostatic drugs. Nanofibers, serving as effective drug carriers, contribute to hemostasis and promote wound healing. Natural polymers, synthetic polymers, inorganic materials, and metal-containing materials constitute the primary categories of materials employed to achieve hemostasis (25). Pictorial representation of various hemostatic dressings are shown in Figure 4.
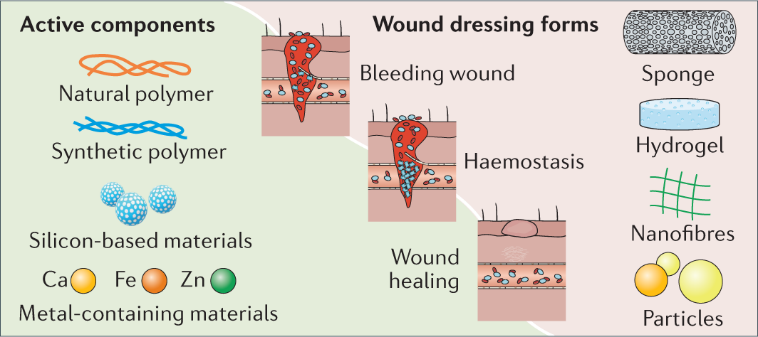
Figure 4: Diverse hemostatic dressings for wound management (25)
Healing-promoting dressings
The process of wound healing necessitates a complex and intricate interaction of growth factors and cytokines to control the recruitment and interaction of various cell types at the wound sites. Growth factors not only prove efficient and safe in addressing acute skin wounds but also stimulate wound healing without inducing significant adverse effects. When injected exogenously, they are promptly deactivated in the wound environment (26). This is an emerging and innovative form of dressing hence further research is warranted to determine its efficacy in practice.
Cell-seeded dressings
Cell-seeded wound dressings are created by combining skin-derived cells or stem cells cultured in vitro, whether autologous or allogeneic, with biomaterials such as collagen, chondroitin sulfate, hyaluronic acid, and chitosan through tissue engineering techniques. These dressings, incorporating cells, have shown the capacity to accelerate wound healing and improve its quality, indicating their potential as innovative skin replacements. While the application of a single growth factor topically is known to enhance wound healing, the utilization of cultured autologous or allogeneic cells proves to be more effective and physiologically relevant. These cells secrete various mediators that coordinate and regulate the healing process. A bilayered bioengineered skin substitute exemplifies this approach (16). Our review provides deep insights into modern and innovative dressings employed in clinical practices to ensure effective wound management with the most recent evidence available in literature. However, the efficacy of each technique was not determined as we considered it beyond the scope of this paper although research in future shall target to determine the effectiveness of these novel dressing techniques analyzed through population cohort studies to develop guidelines for practice.
Conclusion
This review underscores the significant strides made in wound care nursing through the exploration of innovative dressings and techniques. By delving into the latest advancements, this paper has shed light on the evolving landscape of wound management in which the role of nurses is vital for effective implementation of these innovative dressings. The comprehensive evaluation of various dressings and techniques highlights their potential to revolutionize patient care by promoting faster healing, reducing complications, and enhancing overall quality of life. Moving forward, continued collaboration, research, and education within the nursing community will be essential in harnessing the full benefits of these innovations and ensuring optimal outcomes for patients across diverse wound care settings.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical consideration
Non applicable.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.