Volume 4, Issue 10
October 2024
A Review on Viral Skin Infections in Children: Types, Clinical Picture and Outcomes
Aljowharah Salman Ali, Fatema Hosam Madani, Ahmed Mohammedsaeed Baqasi, Sultan Musallam Alshammari, Seham Omar Aldogil, Rana Abdulrahim Alaeq
DOI: http://dx.doi.org/10.52533/JOHS.2024.41009
Keywords: Pediatric, Viral Skin Infections, Herpes Simplex Virus, Varicella-Zoster Virus, Human Papillomavirus, Molluscum Contagiosum, Coxsackievirus
Viral skin infections in children encompass a broad spectrum of conditions with diverse clinical manifestations and outcomes. These infections are caused by various viruses, including Herpes Simplex Virus (HSV), Varicella-Zoster Virus (VZV), Human Papillomavirus (HPV), Molluscum Contagiosum, and Coxsackievirus. Each virus presents with unique clinical features and management needs. Herpes Simplex Virus (HSV) infections, which include oral herpes, herpetic whitlow, and eczema herpeticum, present as painful vesicular lesions. HSV-1 typically affects the oral region, while HSV-2 is more common in genital infections. Herpetic gingivostomatitis and eczema herpeticum can cause extensive oral lesions and severe symptoms, requiring antiviral therapy for severe cases. Varicella-Zoster Virus (VZV) causes chickenpox, characterized by a rash that evolves through macules, papules, vesicles, and crusts, often accompanied by fever. Vaccination has significantly reduced the incidence and severity of VZV infections, but severe cases can still occur, particularly in vulnerable populations. Human Papillomavirus (HPV) infections present as warts on various body parts, including common warts, plantar warts, and flat warts. While many HPV warts are self-limiting, persistent or painful warts may require treatment with cryotherapy, topical therapies, or laser therapy. Molluscum Contagiosum, caused by a poxvirus, manifests as dome-shaped, umbilicated papules on the skin. The lesions are generally painless but can cause cosmetic concerns and secondary bacterial infections. Treatments include cryotherapy and topical therapies, though the infection often resolves spontaneously over several months. Coxsackievirus infections are known for causing Hand, Foot, and Mouth Disease (HFMD), presenting with a rash and oral lesions, along with systemic symptoms like fever. Severe manifestations, such as aseptic meningitis and myocarditis, are less common but require specific medical management. Vaccination and early treatment can mitigate severe outcomes and improve quality of life for affected children.
Introduction
Viral skin infections represent a prevalent and diverse group of conditions encountered in pediatric dermatology. These infections are caused by various viruses and are characterized by a range of clinical manifestations, which can vary from mild and self-limiting to severe and complicated (1). The diverse presentations and outcomes associated with viral skin infections in children necessitate a thorough understanding of their etiology, clinical features, and management strategies. The pediatric population is particularly susceptible to viral skin infections due to their developing immune systems, increased likelihood of exposure in communal settings, and the unique ways in which these infections present in younger patients (2). For instance, while some viral skin infections, such as Herpes Simplex Virus (HSV) and Varicella-Zoster Virus (VZV) infections, have well-established clinical features and management protocols, others, like Molluscum Contagiosum and Human Papillomavirus (HPV) infections, present with less distinctive symptoms that can complicate diagnosis. In addition to their clinical variability, viral skin infections in children can have significant implications for their overall health and well-being. While many viral skin infections are self-limiting and resolve with minimal intervention, others can lead to complications such as secondary bacterial infections, scarring, or more severe systemic involvement (3). Moreover, the social and psychological impact of visible skin lesions can affect a child’s quality of life and emotional well-being.
The introduction of vaccination programs has significantly altered the landscape of viral skin infections, particularly for conditions like varicella and, to a lesser extent, Human Papillomavirus (4). Vaccines have played a crucial role in reducing the incidence and severity of these infections, yet challenges remain in managing and preventing other viral skin conditions. Understanding the types, clinical presentations, and outcomes of viral skin infections is essential for accurate diagnosis and effective management. This review aims to provide a thorough examination of the different types of viral skin infections encountered in pediatric patients, describe their clinical features in detail, and discuss the outcomes associated with these conditions.
Methodology
This study is based on a comprehensive literature search conducted on August 7, 2024, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed types, clinical picture and outcomes associated with viral skin infections in children. There were no restrictions on date, language, participant age, or type of publication.
Discussion
The spectrum of viral skin infections in children is diverse, encompassing several distinct conditions, each with unique clinical features and management strategies. This discussion aims to synthesize the key findings related to Herpes Simplex Virus (HSV), Varicella-Zoster Virus (VZV), Human Papillomavirus (HPV), Molluscum Contagiosum, and Coxsackievirus infections, while exploring their clinical implications and outcomes (Table 1).
Herpes Simplex Virus (HSV) infections are a common concern in pediatric dermatology, with HSV-1 and HSV-2 being the primary strains affecting children (5). HSV-1 is most associated with oral lesions, while HSV-2 typically causes genital infections. Herpes Labialis, also known as cold sores, is one of the most recognizable manifestations of HSV-1 in children. It presents as painful, fluid-filled vesicles that initially appear on the lips or around the mouth. These vesicles eventually rupture, leading to crusting and healing within 1-2 weeks (6). The infection is often accompanied by systemic symptoms such as fever, irritability, and lymphadenopathy. The recurrent nature of herpes labialis, triggered by factors like stress or sun exposure, often necessitates antiviral therapy, such as acyclovir, to reduce the frequency and severity of outbreaks (Figure 1).

Figure 1: Herpes simplex on the buttocks of a child (2).
Herpetic Gingivostomatitis is another significant manifestation of HSV-1 in children, particularly in younger age groups (7). This condition is characterized by extensive oral lesions that include vesicles and ulcers on the gingiva, tongue, and roof of the mouth. Children with herpetic gingivostomatitis often present with fever, irritability, and difficulty eating or drinking due to pain. The disease generally resolves within 1-2 weeks with supportive care, including hydration and pain management. In severe cases or in immunocompromised children, antiviral medications may be prescribed to manage symptoms and prevent complications. Herpetic Whitlow is a less common but notable presentation of HSV infection in children, characterized by painful vesicular lesions on the fingers (8). This condition often occurs in children who have had direct contact with HSV-infected lesions, either through oral lesions or from other infected individuals. Herpetic whitlow can cause significant discomfort and may require antiviral treatment to control the infection and prevent secondary bacterial infections. Eczema Herpeticum occurs in children with pre-existing eczema and is marked by widespread vesicular eruptions on eczematous skin (9). This condition can be particularly severe, with the potential for extensive skin involvement and significant systemic symptoms. Eczema herpeticum often requires antiviral treatment to manage the infection and prevent complications such as bacterial superinfection. Overall, HSV infections in children can have a considerable impact on their health and quality of life. While many cases resolve with minimal intervention, antiviral therapy can be crucial for managing severe infections and reducing the frequency of recurrences. Early diagnosis and appropriate treatment are essential for minimizing discomfort and preventing complications associated with HSV infections.
Varicella-Zoster Virus (VZV) is responsible for causing varicella, commonly known as chickenpox, a highly contagious viral infection prevalent in children (13). The clinical presentation of varicella is characterized by a distinctive exanthematous rash that progresses through several stages, which are crucial for both diagnosis and management. The initial stage of varicella presents with small, red macules that quickly evolve into papules (Figure 2). These papules then develop into vesicles filled with clear fluid. The vesicles eventually crust over, with the rash usually beginning on the trunk and face before spreading to the extremities. The progression of the rash through these stages—macules, papules, vesicles, and crusts—typically occurs within a few days, and new lesions can continue to appear for several days (12). In addition to the rash, affected children commonly experience systemic symptoms such as fever, malaise, and pruritus, which contribute to the overall discomfort of the infection. Varicella is usually a self-limiting condition, with the rash and systemic symptoms resolving within 1-2 weeks. However, complications can arise, particularly in children with weakened immune systems, pregnant women, and newborns. Potential complications include secondary bacterial infections of the skin, varicella pneumonia, and, in rare cases, encephalitis (11). Secondary bacterial infections can occur when vesicles become crusted or when children scratch the lesions, leading to additional skin infections that require antibiotic treatment. The introduction of the varicella vaccine has significantly impacted the prevalence and severity of chickenpox.
|
Table 1. Overview of Viral Skin Infections in Children |
|||||
|
Virus/Condition |
Type of Infection |
Clinical Presentation |
Common Locations |
Typical Outcome |
Treatment Options |
|
Herpes Simplex Virus (5-10) |
Oral herpes, Herpetic whitlow, Eczema herpeticum |
Painful vesicular lesions, ulcers, eczema complications |
Lips, fingers, body areas affected by eczema |
Generally self-limiting; antiviral treatment for severe cases |
Antiviral medications, supportive care |
|
Varicella-Zoster Virus (11-13) |
Chickenpox (Varicella) |
Rash with macules, papules, vesicles, and crusts; fever |
Trunk, face, limbs |
Self-limiting; complications in high-risk groups |
Symptomatic treatment, antiviral medications for severe cases |
|
Human Papillomavirus (14-18) |
Common warts, Plantar warts, Flat warts |
Rough, raised lesions; pain or discomfort for plantar warts |
Hands, feet, face, legs |
Often self-limiting; treatment for persistent or painful warts |
Topical treatments, cryotherapy, laser therapy |
|
Molluscum Contagiosum (19-21) |
Molluscum Contagiosum |
Dome-shaped, umbilicated papules |
Trunk, arms, legs, face |
Self-limiting; cosmetic concerns or secondary infection may occur |
Cryotherapy, topical treatments |
|
Coxsackievirus (22-27) |
Hand, Foot, and Mouth Disease (HFMD), Aseptic meningitis, Myocarditis |
Rash, oral vesicular lesions, fever; headache, neck stiffness for meningitis; chest pain for myocarditis |
Hands, feet, mouth; general body areas for systemic symptoms |
HFMD is self-limiting; meningitis and myocarditis require medical management |
Supportive care; antiviral treatment for severe cases; specific management for myocarditis |

Figure 2: Varicella: initial lesions on the head (2).
Vaccination programs have led to a marked reduction in the incidence of varicella and its associated complications (13). The vaccine has also contributed to a decrease in hospitalizations and severe outcomes related to varicella. For children who do develop chickenpox, antiviral medications like acyclovir can be used in severe cases or in those at high risk for complications to reduce the severity and duration of symptoms. Overall, while varicella is generally a mild and self-limiting infection in healthy children, the potential for complications and the impact on public health make vaccination and effective management strategies essential. Understanding the clinical progression of varicella and recognizing potential complications can help in providing appropriate care and ensuring the well-being of affected children.
Human Papillomavirus (HPV) infections in children present as various types of warts, which are benign, localized growths caused by different HPV strains (18). These infections are relatively common in pediatric populations and can affect various body parts, each presenting distinct clinical features. Common Warts are the most prevalent form of HPV infection in children, typically appearing on the hands and fingers (Figure 3). These warts are characterized by their rough, raised surface and may be slightly hyperkeratotic (17). They often have a characteristic appearance with a grayish or brownish hue and can be multiple or single. Common warts are generally asymptomatic but can sometimes be tender or cause discomfort, especially if they are located on pressure-bearing areas like the palms. They are usually self-limiting and can resolve spontaneously over several months to years. However, persistent warts may require treatment to alleviate symptoms and prevent transmission to others.

Figure 3: Periungual warts (28).
Plantar Warts are found on the soles of the feet and are particularly notable for their painful nature (16). These warts are often presented as thickened, rough lesions with a characteristic appearance due to the pressure from walking and standing. Plantar warts can cause significant discomfort and difficulty in walking, making them a more serious concern compared to common warts. The pain associated with plantar warts is due to their location and the pressure they endure. Treatment options for plantar warts include cryotherapy, topical treatments, and laser therapy. Persistent warts may require more aggressive interventions. Flat Warts are another type of HPV infection, typically presenting as smooth, slightly raised lesions that can appear on the face, arms, or legs. These warts are often multiple and can be less conspicuous than common or plantar warts. Flat warts are usually less symptomatic but can be aesthetically concerning, especially when located on visible areas like the face (15). Treatment for flat warts may involve topical therapies, such as salicylic acid or imiquimod, and other methods like cryotherapy or laser therapy for persistent cases. The outcomes of HPV infections in children vary depending on the type and location of the warts. While many warts resolve spontaneously without intervention, some can persist for extended periods or become recurrent. Treatment is often aimed at alleviating symptoms, preventing the spread of the virus, and reducing the likelihood of recurrence. In some cases, warts can be resistant to treatment, requiring repeated or combined therapies. Additionally, while HPV infections are generally benign, certain high-risk strains are associated with more severe conditions, including genital warts and potential progression to cancer in other populations (14). Overall, HPV infections in children are common and typically benign, but they can cause discomfort and aesthetic concerns. Effective management involves both therapeutic interventions and preventive measures to minimize the spread of the virus and address the specific needs of affected children.
Molluscum Contagiosum is a viral skin infection caused by the Molluscum Contagiosum virus (MCV), a member of the poxvirus family (21). This infection is characterized by the development of distinctive skin lesions that can be particularly concerning in pediatric patients due to their appearance and potential for spread. Molluscum Contagiosum typically manifests as small, dome-shaped papules with a characteristic central umbilication. These lesions are usually flesh-colored or pearly white and have a smooth surface. They can range in size from 1 to 5 millimeters in diameter and are often found in clusters. Common sites of infection include the trunk, arms, legs, and sometimes the face. In the case of children, the lesions are frequently located in areas where the skin is in frequent contact, such as the inner thighs and the abdominal region (20). The papules are generally asymptomatic, although they can occasionally become inflamed, itchy, or irritated. Secondary bacterial infections can occur if the lesions are scratched or traumatized. Molluscum Contagiosum lesions are usually painless, but their appearance can cause psychological distress, particularly if they are located on visible areas of the body (Figure 4).

Figure 4: Molluscum contagiosum: pearly papules, some of them with umbilication. (2).
Molluscum Contagiosum is often a self-limiting condition, with the lesions typically resolving spontaneously within 6 to 12 months. The duration of the infection can vary, with some cases lasting longer, particularly in immunocompromised individuals or those with extensive lesions. While the infection is generally benign, it can cause significant cosmetic concerns and discomfort. Treatment options are available for children who experience significant discomfort, have numerous lesions, or whose lesions persist for extended periods. These treatments include cryotherapy, curettage, and topical therapies such as imiquimod or tretinoin (19). Other methods, like laser therapy or chemical treatments, may also be employed depending on the severity and persistence of the infection (Table 2).
Despite treatment, Molluscum Contagiosum can have a high recurrence rate, and new lesions may appear even after initial treatment. This can be due to the contagious nature of the virus and the potential for transmission to other areas of the skin or to other individuals. Therefore, preventive measures, such as avoiding direct contact with infected individuals and practicing good hygiene, are crucial in managing the spread of the virus. Overall, while Molluscum Contagiosum is typically a benign and self-limiting infection, it can present challenges in terms of treatment and recurrence. Understanding the clinical presentation and outcomes of Molluscum Contagiosum can help guide appropriate management strategies and alleviate concerns for affected children and their families.
Coxsackievirus infections, a member of the enterovirus family, commonly affect children and are associated with several distinct clinical syndromes (27). These infections are notably recognized for causing hand, foot, and mouth disease (HFMD), but they can also lead to other conditions with varying presentations. Hand, Foot, and Mouth Disease (HFMD) is the most common manifestation of Coxsackievirus infection in children. It typically presents with a triad of symptoms: a rash on the hands and feet, oral vesicular lesions, and systemic symptoms such as fever and malaise (26). The rash associated with HFMD often begins as small, red spots that rapidly develop into vesicles. These vesicles are most commonly found on the palms, soles, and buttocks (Figure 5). The oral lesions, which can be painful, appear as small, vesicular lesions on the mucous membranes of the mouth, including the tongue, gums, and inner cheeks. The systemic symptoms usually precede or accompany the rash and include fever, irritability, and occasionally mild gastrointestinal symptoms.
|
Table 2. Key Clinical Features and Management Strategies for Viral Skin Infections in Children |
|||||
|
Virus/Condition |
Condition |
Key Clinical Features |
Risk Factors |
Management Strategies |
Prevention |
|
Herpes Simplex Virus (5-10) |
Herpes Simplex Virus |
Painful oral lesions, recurrent outbreaks |
Close contact, immunocompromised status |
Antiviral medications, symptomatic relief |
Good hygiene, avoid sharing utensils |
|
Varicella-Zoster Virus (11-13) |
Varicella-Zoster Virus |
Rash in multiple stages, fever |
Lack of vaccination, close contact |
Symptomatic treatment, antiviral medications if severe |
Vaccination, good hygiene practices |
|
Human Papillomavirus (14-18) |
Human Papillomavirus |
Various types of warts with different appearances |
Direct contact with infected lesions |
Topical treatments, cryotherapy, laser therapy |
Avoiding direct contact with warts, good hygiene |
|
Molluscum Contagiosum (19-21) |
Molluscum Contagiosum |
Umbilicated papules, usually painless |
Close contact, atopic dermatitis |
Cryotherapy, topical treatments |
Avoid sharing personal items, good hygiene |
|
Coxsackievirus (22-27) |
Coxsackievirus |
Rash, oral lesions, systemic symptoms like fever, headache |
Close contact, crowded environments |
Supportive care, antiviral medications if necessary |
Good hygiene, avoiding contact with infected individuals |
Aseptic Meningitis and Myocarditis are less common but significant manifestations of Coxsackievirus infections (25). Aseptic meningitis presents with symptoms such as headache, neck stiffness, photophobia, and fever, often without the characteristic rash of HFMD. It is typically self-limiting, but severe cases may require supportive care. Myocarditis, though rare, can occur and is characterized by symptoms of heart failure, including shortness of breath, fatigue, and chest pain (24). This condition requires prompt medical attention and management to prevent serious complications. HFMD is generally mild and self-limiting, with most children recovering within 7-10 days. The main focus of treatment is symptomatic relief, including managing fever and pain. Hydration and a soft diet may help alleviate discomfort from oral lesions. While HFMD resolves on its own, it is highly contagious, and outbreaks are common, especially in settings like daycare centers and schools. Preventive measures, such as good hygiene practices and isolation of affected individuals, are essential to control the spread of the virus (23). Aseptic Meningitis and Myocarditis associated with Coxsackievirus infections require careful monitoring and supportive care. Aseptic meningitis usually resolves with minimal intervention, while myocarditis may require more intensive management, including hospitalization and treatment tailored to the specific cardiac symptoms (22). In summary, Coxsackievirus infections in children primarily present as HFMD, characterized by a distinctive rash and oral lesions. While HFMD is typically mild, other manifestations such as aseptic meningitis and myocarditis can occur and require appropriate medical attention. Understanding the clinical presentation and outcomes of Coxsackievirus infections is crucial for effective management and prevention of complications.
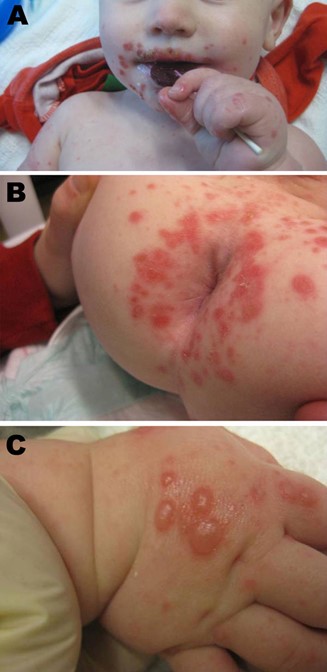
Figure 5: Manifestations of hand, foot, and mouth disease in patients, Boston, Massachusetts, USA, 2012. Discrete superficial crusted erosions and vesicles symmetrically distributed in the perioral region (A), in the perianal region (B), and on the dorsum of the hands (C) (29).
Conclusion
Viral skin infections in children encompass a range of conditions with varied clinical presentations and outcomes. While many infections, such as Herpes Simplex Virus and Varicella-Zoster Virus, generally resolve with minimal intervention, some, like Molluscum Contagiosum and Human Papillomavirus infections, may require specific treatments due to their persistent nature or impact on quality of life. Coxsackievirus infections, including Hand, Foot, and Mouth Disease, are usually self-limiting but can present with more serious complications such as aseptic meningitis or myocarditis. Vaccination programs have significantly reduced the incidence and severity of certain viral infections, yet challenges in management persist. Effective diagnosis, treatment, and preventive measures are essential in addressing the diverse spectrum of viral skin infections and minimizing their impact on pediatric patients.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable
Consent for publications
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The author declares no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.
