Volume 4, Issue 10
October 2024
An Overview of Acute Drug Overdose and Poisoning in Emergency Medicine
Ahmed Amin Aljefri, Saud Faisal Nahhs, Rawan Mattouk Kheimi, Abdulelah Yousef Alhamdan, Turki Sanat Alharbi, Saud Sheher Alkahtani, Salem Tarheeb Alajmi, Faisal Naif Alotaibi, Badran Ahmed AlJardan, Reema Sulaiman Alsalmi
DOI: http://dx.doi.org/10.52533/JOHS.2024.41003
Keywords: Acute drug overdose, poisoning, emergency medicine, opioid overdose, naloxone, harm reduction, prevention
Acute drug overdose and poisoning are critical concerns in emergency medicine, often arising from both intentional and unintentional exposures to harmful substances. Poisoning occurs when a substance causes harm through its chemical effects, whereas an overdose usually involves taking an excessive amount of drugs, whether by accident or on purpose. The rising incidence of drug overdoses, particularly involving opioids, sedatives and stimulants, poses significant challenges to healthcare providers. Risk factors for overdose include individual characteristics such as male gender, chronic health conditions and prior overdose experiences. Drug-related factors, including polydrug use and the route of administration, also contribute to overdose risk. Timely intervention is crucial in managing overdoses, with treatments varying based on the substance involved. For instance, opioid antagonists like naloxone are vital in reversing opioid overdoses. Prevention strategies, including harm reduction and expanded access to naloxone, are essential in addressing this public health issue. Recognizing the symptoms, risk factors and treatment options for acute drug poisoning is crucial for enhancing patient outcomes and lowering mortality rates.
Introduction
Poisoning refers to the intentional or unintentional harm or impairment of a living organism caused by a substance's chemical action. This concept distinguishes between accidental toxic exposure, which occurs unintentionally, and toxic overdose, which can result from either intentional or accidental exposure to a harmful substance (1, 2). While the terms overdose and poisoning are often used interchangeably when discussing drugs of abuse, an overdose does not usually lead to poisoning unless it causes symptoms (1). The concept of overdose covers multiple aspects. A frequently referenced definition revolves around the straightforward notion of excessive use, such as an accidental or deliberate dose of a medication or street drug that exceeds what is typically used.
The use of illicit drugs, particularly in large quantities or after a period of abstinence, can result in an overdose. For instance, individuals who inject cocaine or opioids intravenously are at elevated risk for accidental overdose due to the narrow margin between achieving a pleasurable effect and experiencing an overdose (3). Overdose can occur either accidentally or intentionally. For example, unintentional overdose might happen when a person uses opioids along with other central nervous system (CNS) depressants (e.g., alcoholic beverages or sedative-hypnotics), potentially leading to respiratory depression (4).
Physicians, particularly in critical care and emergency medicine, frequently encounter intoxicated patients, facing various clinical scenarios such as known drug overdoses, unknown illicit drug intoxications, suicide attempts, and accidental exposures. The diverse and challenging manifestations of acute drug poisoning necessitate a high index of suspicion for intoxication in critical care practice (5). The treatment and complications of intensive care unit (ICU) patients with acute drug intoxication differ based on the type of substance ingested, the quantity consumed, and the concurrent use of other substances. According to the 2019 Global Burden of Disease (GBD) study, unintentional poisoning was responsible for 0.14% of global deaths, while self-harm accounted for 1.34%. Despite the relatively low mortality rate, the World Health Organization (WHO) continues to recognize poisoning as a significant public health concern (6).
Acute poisoning poses a complex public health challenge that demands prompt medical intervention and can lead to hospitalization or death for thousands of individuals. The WHO reports that around 800,000 people die annually due to suicide, with self-harm poisoning accounting for 1.34% of global deaths. The WHO has highlighted poisoning as a major public health issue, especially in middle- and low-income countries (6, 7).
Ensuring appropriate medical care for patients affected by poisoning is essential. Healthcare providers should be encouraged to promptly report poisoning cases as notifiable medical conditions, including those involving lead, mercury, and agricultural or stock remedy poisoning (8).
The purpose of this study is to present an overview of acute drug overdose and poisoning in emergency medicine.
Methodology
This study is based on a comprehensive literature search conducted on August 22, 2024, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed an overview of acute drug overdose and poisoning in emergency medicine. There were no restrictions on date, language, participant age, or type of publication.
Discussion
A variety of psychotropic drugs have been associated with the occurrence of overdose, with opioids (primarily heroin), sedatives-hypnotics (such as barbiturates and benzodiazepines), prescribed opioid analgesics, ethanol, stimulants (including cocaine, amphetamine, and 3,4-methylenedioxy-methamphetamine (MDMA), and club drugs like gamma-hydroxybutyrate (GHB) being the most reported. The presentation of symptoms can vary significantly depending on the type of drug and the severity of the overdose, providing important clues for diagnosis. Even within the same medication category, the symptoms and risk of fatal outcomes can differ by compound, due in part to variations in onset time, duration of behavioural effects, and elimination half-life. For instance, Alprazolam and Flunitrazepam are more frequently associated with fatal overdoses than other benzodiazepines. Clinically, opioid overdose is typically diagnosed by the presence of CNS and respiratory depression, myosis, and evidence of opioid use (e.g., needle tracks or soft tissue infections). In cases of heroin overdose, a triad of abnormal mental status, depressed respiration, and miotic pupils provides a diagnostic sensitivity of 92% and specificity of 76%. Sedative-hypnotic overdoses are primarily diagnosed based on CNS and respiratory depression (4).
Risk factors
Over the past two decades, various reviews and studies have sought to identify the risk factors for both nonfatal and fatal overdoses, especially concerning opioids. These risk factors can be broadly categorized into four domains: individual-level characteristics, drug-related attributes, circumstances and time-related factors.
Individual-Level Characteristics
Across all drug categories, including illegal drugs (heroin, cocaine, amphetamine), prescription drugs (e.g., analgesics) and polydrug use, the male gender has consistently been associated with a higher risk of overdose. This excess risk persists even when accounting for the predominance of male drug users. The average age for fatal heroin overdose victims typically falls between the late twenties and early thirties, with nonfatal overdoses occurring at younger ages. Similar age-related risks have been observed for cocaine and unintentional pharmaceutical overdoses. Additionally, chronic health conditions, such as liver cirrhosis, ventricular hypertrophy, and bronchopneumonia, have been frequently linked to fatal overdoses. Other significant individual risk factors include a history of substance use disorders, changes in drug tolerance, and prior nonfatal overdose experiences. Individuals who have previously experienced nonfatal overdoses are at a higher risk of subsequent fatal overdoses, with the risk increasing with the number of prior nonfatal events (9, 10).
Drug-Level Characteristics
Drug-related factors play a crucial role in overdose risk, with polydrug use being particularly significant. For instance, heroin users who concurrently use alcohol or benzodiazepines are at a higher risk of overdose due to the combined depressant effects that can lead to respiratory depression. Similar risks are observed with cocaine, MDMA, and certain prescription drugs when used in combination with other substances. The route of drug administration is another critical factor; for example, intravenous heroin use is associated with a significantly higher risk of overdose compared to smoking, intramuscular, or subcutaneous routes. This pattern also holds for other drugs such as cocaine, amphetamine, and methadone, where intravenous use is more frequently linked to overdose than inhalation or oral intake (4).
Time-Level Characteristics
Time-related factors, such as periods of recent abstinence, also influence overdose risk. For instance, individuals recently released from prison are at a significantly higher risk of overdose, particularly within the first two to three weeks post-release. Similarly, the risk of fatal overdose is elevated shortly after discharge from hospital drug treatment programs or upon entry or re-entry into methadone maintenance programs, particularly within the first month of these changes (11, 12).
Circumstance-Level Characteristics
Overdoses that occur in public places or abandoned buildings are more likely to be fatal, due to delays in seeking medical help. Additionally, environmental factors like ambient temperature have been linked to accidental cocaine overdose deaths, with higher temperatures correlating with increased mortality rates (13-15).
Risk factors that lead to poisoning revolve around the age and mental maturity of the affected individual. Like children, who are susceptible to unintentional poisoning. There are many factors leading to child poisoning such as inadequate supervision, unsafe storage and unsafe environment (16). Other factors that can lead to accidental poisoning is primary education level of the individual, such as an elderly or people with learning disabilities.
Importance of History taking
The goal of history-taking is to identify the toxic agent responsible for the poisoning or overdose. An extensive history is crucial for understanding the individual's symptoms, exposure, and circumstances. Healthcare providers should approach the interview with confidence and calmness to encourage accurate information sharing. If the patient is unable to provide a full history, efforts should be made to obtain collateral information from friends or family members (1).
Physical examination
Healthcare professionals managing patients exposed to poisonous substances, such as nerve agents or organophosphate pesticides, should don appropriate protective gear before performing any procedures. A thorough physical examination is crucial for identifying toxidromes and guiding treatment decisions (Table 1) (8). Most of the time, drug overdose patients come in a state of drowsiness or an altered level of conscious, making it difficult for the physician to get direct answers from the patient (17). Therefore, it’s up to the physical examination to help initially guide the physician to the right overdosed drug.
|
Table 1. Major Clinical Signs and Symptoms of Toxicity (Toxidromes) (8) |
||
|
Clinical Sign/Symptom |
Description |
Associated Toxidromes/Substances |
|
Level of Consciousness |
Reduced consciousness; rule out diabetes, stroke, head injury, etc. |
- |
|
Pupil Reflexes |
Dilated pupils for cocaine, amphetamines, cannabis; pinpoint for opiates, organophosphates. |
Cocaine, amphetamines, cannabis, opiates, organophosphates |
|
Eye Movement |
Nystagmus from drugs. |
Phencyclidine, ethanol, phenytoin |
|
Breathing |
Kussmaul respiration for acidosis; hyperventilation for metabolic acidosis or methanol. |
Alcohol, salicylates, methanol |
|
Motor Function |
Flaccid paralysis; unresponsiveness. |
- |
|
Cardiac Arrhythmias |
Monitor for arrhythmias from cocaine, theophylline, digoxin, antidepressants, arsenic. |
Cocaine, theophylline, digoxin, antidepressants, arsenic |
|
Seizures |
Seizures from poisoning; benzodiazepines for control. |
Alcohol, sedative-hypnotics, benzodiazepines |
|
Gastrointestinal Disturbance |
Vomiting, bleeding, diarrhea; mercury may cause mucous diarrhea. |
Theophylline, iron, arsenic, lithium, mercury |
Vitals Stabilization
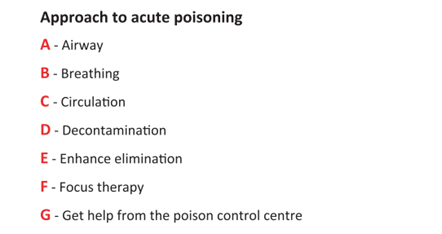
Patients with overdose or poisoning are often unstable and require immediate stabilization of their vital signs, including airway management, adequate ventilation, and circulation maintenance (Figure 1) (8).
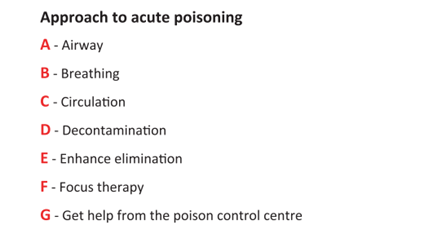
Figure 1: Approach to the poisoning case in the emergency room (8).
Certain chemicals or drugs may compromise the respiratory tract, necessitating rapid sequence intubation and ventilatory support. Conditions such as corrosive ingestion, chlorine inhalation, pulmonary edema, bronchorrhea, CNS depression, seizure and aspiration require urgent attention.
Diagnostic tests
Diagnosis for acute drug overdose or poisoning are essential to help identify the drug or poison causing the symptoms. It is important for healthcare professionals to know which tests to do first, especially in an emergency setting where there is limited time. Table 2 displays the important diagnostic tests and how they can detect poisoning within the body.
|
Table 2. Common Diagnostic Tests for Poisoning (8) |
|
|
Diagnostic Test |
Description |
|
Full Blood Count (FBC) |
Assesses overall health and detects various types of poisons. |
|
Serum Electrolytes |
Measures levels of electrolytes to detect imbalances. |
|
Urea and Creatinine |
Evaluate kidney function and identify renal impairment. |
|
Blood Glucose |
Measures blood sugar levels to identify hyperglycemia or hypoglycemia. |
|
Serum Calcium |
Determines calcium levels, which can be disrupted in certain poisonings. |
|
Urinalysis |
Analyzes urine to detect abnormalities and identify toxins. |
|
Prothrombin Time (PT) |
Assesses blood clotting ability and can indicate liver dysfunction. |
|
Pulse Oximetry |
Measures oxygen saturation in the blood. |
|
12-Lead Electrocardiography (ECG) |
Evaluate heart rhythm and detect potential cardiac issues. |
|
Arterial Blood Gas (ABG) Analysis |
Measures blood gases to assess respiratory and metabolic functions. |
|
Toxicology Drug Screen |
Identifies the presence of specific drugs and toxins. |
|
Liver Function Tests |
Assesses liver health, crucial in cases of acetaminophen or paracetamol toxicity. |
Management of drug overdose and poisoning
Management of drug overdose requires prompt and effective intervention, particularly given that less than one-quarter of overdoses occur within three hours of drug administration, offering a critical window for action. For opioid, heroin, or methadone overdoses, opioid antagonists like naloxone (Narcan) are essential, as they reverse the effects of these substances by blocking mu-opiate receptors, with higher doses required for buprenorphine overdoses due to its strong receptor affinity. Naloxone's availability to high-risk opioid users has been crucial in preventing fatalities. In sedative-hypnotic overdoses, the primary focus is on maintaining the airway and ventilator support, with flumazenil used to reverse the sedative effects of benzodiazepines, especially short-acting ones. Stimulant overdoses are treated with medications like bupropion, aripiprazole, and topiramate, which act on catecholamine reuptake sites, and receptors, or reduce drug availability in the central nervous system, alongside vigilant monitoring for complications such as seizures, cardiac arrhythmias, and stroke. These strategies, when applied promptly, can significantly mitigate the risk of fatal outcomes in overdose cases (4).
Decontamination
Skin and Eyes
Water is commonly used to decontaminate the skin and eyes, effectively reducing the impact of dermal exposure (1). For burns caused by toxic exposure, it is essential to adhere to established burn management protocols, which involve applying wound dressings and monitoring for signs of infection.
Gastrointestinal Tract
Pre-Absorption Elimination: Decontamination strategies should be tailored to the individual (1).
Activated Charcoal: Activated charcoal binds various substances, reducing their systemic absorption in the gastrointestinal tract. It is most effective if administered within an hour of ingestion (8). Recommended dosages are 0.5 g – 1 g for children and 25 g – 100 g for adults. For life-threatening toxic doses undergoing enteroenteric or enterohepatic circulation, multiple doses may be necessary. Sorbitol-containing charcoal should be avoided in infants due to its emetic and dehydrating effects. Charcoal administration is not suitable for individuals with compromised airways or reduced consciousness levels until intubation is completed (1).
Gastric Lavage: Gastric lavage involves blind insertion of a large-bore tube into the stomach and is highly controversial, dependent on practitioner expertise. Potential complications include hypoxia, gastrointestinal perforation, and aspiration pneumonitis. It is indicated for severe cases where substances were ingested within an hour but are contraindicated for petroleum products, acidic substances, and when airway protection cannot be assured (1, 18).
Whole Bowel Irrigation: This involves administering a large volume of polyethylene glycol via the mouth or nasogastric tube to rapidly clear toxic substances from the gastrointestinal tract. It is particularly useful for substances like lithium, iron, enteric-coated drugs, and cases of body packing with heroin, cocaine, or opioids. Administer polyethylene glycol solution at 25 mL/kg/hr – 40 mL/kg/hr until the effluent is clear. Whole bowel irrigation is contraindicated in cases of gastrointestinal bleeding, bowel obstructions, or unstable conditions where airway protection is not feasible (8).
Post-Absorption Elimination
Several methods can accelerate the clearance of toxins after gastrointestinal absorption:
Multidose Activated Charcoal: This method, also known as "gastrointestinal dialysis," disrupts enterohepatic circulation (1).
Extracorporeal Methods: Techniques such as peritoneal dialysis, haemodialysis and haemoperfusion are used for poisonings likely to cause toxic metabolic activation and severe metabolic acidosis, especially when conventional treatments are ineffective. This includes cases involving ethylene glycol, and methanol, and situations unresponsive to standard support measures (19).
Antidote Administration
The use of specific antidotes is crucial in clinical toxicology. Administering an antidote within the first hour following exposure is often recommended for stabilization. Common poisons and their corresponding antidotes (8).
Monitoring and Disposition
Patients with poisoning need symptomatic care and continuous monitoring. Since the exact toxic substance may be unknown, it is crucial to closely monitor oxygen saturation, vital signs, and cardiac rhythm, particularly in severe cases (2). Unstable patients who cannot have their airways protected may require transfer to a high-care or intensive care unit for continuous monitoring and ventilatory support. Employing a multidisciplinary approach is highly recommended (20).
For patients with pre-existing conditions like diabetes or heart failure, close monitoring is particularly important, as poisoning may worsen these conditions (19). Additionally, careful observation is necessary to manage injuries resulting from the overdose. Patients who have intentionally self-poisoned should undergo a psychosocial assessment before discharge, considering their psychosocial disorder status (2, 20).
Prevention
Preventing drug overdose and poisoning remains a critical public health challenge. Promising strategies, including opioid substitution therapies like Methadone and Buprenorphine, harm-reduction activities and expanding access to Naloxone, have shown potential in reducing overdose-related deaths. Community-based interventions aimed at training users and their families on emergency responses further support these efforts. Although prescription drug overdose prevention is still under investigation, ongoing initiatives such as physician education and prescription monitoring hold promise. Continued research and implementation of these strategies are essential for addressing both poisoning and drug overdose mortality (21-23).
Future directions
Future directions in tackling poisoning and drug overdoses emphasize enhanced surveillance, personalized treatment options, and expanded harm reduction services, including supervised consumption sites. Integrating mental health and substance use treatments in healthcare settings and launching public education campaigns on polydrug use is crucial. Policy reforms to reduce stigma and encourage help-seeking, along with research on long-term effects and preventive interventions, are essential for reducing poisoning and overdose fatalities.
Conclusion
Addressing drug overdoses requires a multifaceted approach, combining prevention, treatment, and harm reduction strategies. Strengthening healthcare integration, advancing public education and implementing policy reforms are vital. Continued research and innovative interventions are essential for reducing fatalities and supporting those at risk, fostering a more effective response to the overdose crisis.
Disclosures
Author Contributions
All authors have reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Consent for publications
Not applicable
Ethics Statement
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not Applicable