Volume 4, Issue 9
September 2024
An Overview of Management and Complications of Severe Burns and Thermal Injuries
Suhail Mohammed Kashkary, Abdullatif Ahmed Alfaifi, Fatima Abdullah AlGhamdi, Maitham Saeed Alzaer, Atheer Ali Alabbasi, Zahraa Mohammed lawasani, Nashwa Mohammed Almatrodi, Abrar Ghazai Alanazi, Maryam Abdulredha Neama, Qanot Naser Alshatti
DOI: http://dx.doi.org/10.52533/JOHS.2024.40907
Keywords: severe burns, thermal injuries, burn management, grafting techniques, burn rehabilitation
Severe burns and thermal injuries present a significant medical challenge, requiring a comprehensive approach to management and rehabilitation. The initial phase of care focuses on stabilizing the patient through fluid resuscitation, wound care, and pain management. Early excision and grafting are critical to reduce the risk of infection and improve survival outcomes. Pain management is essential to minimize the stress response and promote healing, with multimodal analgesia often employed to achieve effective control. Long-term rehabilitation is equally important, addressing physical recovery, functional restoration, and psychological well-being. Physical and occupational therapy play key roles in preventing and managing complications such as contractures, which can severely limit mobility and independence. The psychological impact of severe burns is profound, with many survivors experiencing post-traumatic stress disorder, depression, and anxiety, underscoring the need for integrated mental health support throughout the recovery process. Grafting techniques, including autografting, allografts, and innovative approaches like cultured epithelial autografts and biosynthetic grafts, are vital in restoring skin integrity and function, especially in patients with extensive burns. Complications such as infections, hypertrophic scars, and metabolic disturbances pose ongoing challenges in the care of burn patients. Rigorous infection control measures, scar management strategies, and nutritional support are essential components of comprehensive burn care. The hypermetabolic response to severe burns necessitates careful management to prevent prolonged catabolism and support wound healing. Overall, the management of severe burns requires a multidisciplinary approach that addresses the acute phase of injury, long-term rehabilitation, and the prevention and treatment of complications. Advances in burn care continue to improve patient outcomes, but the complexity of these injuries demands ongoing research and innovation to enhance recovery and quality of life for burn survivors.
Introduction
Severe burns and thermal injuries remain a significant challenge in the field of medicine, both in terms of immediate management and long-term outcomes. These injuries, often resulting from exposure to high temperatures, chemicals, electricity, or radiation, can cause profound damage to the skin, underlying tissues, and other organs. The complexity of these injuries demands a comprehensive and multidisciplinary approach to treatment, ranging from initial emergency care to extensive rehabilitation efforts. Understanding the pathophysiology, management, and complications of severe burns is critical for improving patient outcomes and reducing morbidity and mortality associated with these injuries.
Burn injuries are classified based on the depth and extent of tissue damage. First-degree burns involve only the epidermis, resulting in redness and pain but usually healing without scarring. Second-degree burns extend into the dermis and may cause blistering, severe pain, and potential scarring. Third-degree burns, also known as full-thickness burns, destroy both the epidermis and dermis, leading to loss of sensation and necessitating surgical intervention for healing. The management of severe burns is complex and multifaceted, requiring prompt fluid resuscitation, wound care, pain management, and infection control to prevent complications such as sepsis, multi-organ failure, and contractures (1).
The advancements in burn care, including the development of specialized burn centers, have significantly improved survival rates and functional outcomes for patients with severe burns. However, the long-term rehabilitation of burn survivors remains challenging, with many patients facing physical and psychological obstacles that require ongoing care. These challenges include scarring, contractures, chronic pain, and psychological trauma, all of which can significantly impact a patient's quality of life (2). Furthermore, complications such as infections, systemic inflammatory responses, and metabolic disturbances often complicate the recovery process, necessitating a vigilant and proactive approach to management (3).
The understanding of burn pathophysiology and the evolution of treatment modalities over the past few decades have led to significant improvements in the prognosis of burn patients. Nonetheless, severe burns continue to pose a substantial burden on healthcare systems and patients alike, emphasizing the need for continued research and innovation in burn care. This review aims to provide an overview of the current management strategies for severe burns and thermal injuries, as well as the common complications that arise during the recovery process (4).
Review
Severe burns and thermal injuries pose a complex challenge to healthcare providers due to the intricate interplay of physiological responses, the risk of complications, and the need for long-term care. The initial management of severe burns involves addressing life-threatening issues such as airway compromise, fluid loss, and shock, which are critical in the first 24 to 48 hours. Fluid resuscitation is paramount in preventing burn shock and ensuring adequate tissue perfusion, but it must be carefully monitored to avoid complications like fluid overload and edema, which can exacerbate tissue damage and lead to secondary injuries (5). Early excision and grafting of burn wounds have been shown to reduce mortality and hospital stay, but they require careful timing and consideration of the patient’s overall condition.
In addition to acute management, addressing long-term complications such as scarring, contractures, and chronic pain is crucial for improving the quality of life in burn survivors. The psychological impact of severe burns, including post-traumatic stress disorder (PTSD), depression, and anxiety, is often underappreciated yet significantly affects recovery and reintegration into society. Multidisciplinary rehabilitation programs, including physical therapy, occupational therapy, and mental health support, are essential for addressing these issues and promoting functional recovery (6). As research continues to evolve, new strategies in burn care are being explored, aiming to reduce complications and enhance recovery outcomes.
Acute Management Strategies for Severe Burns
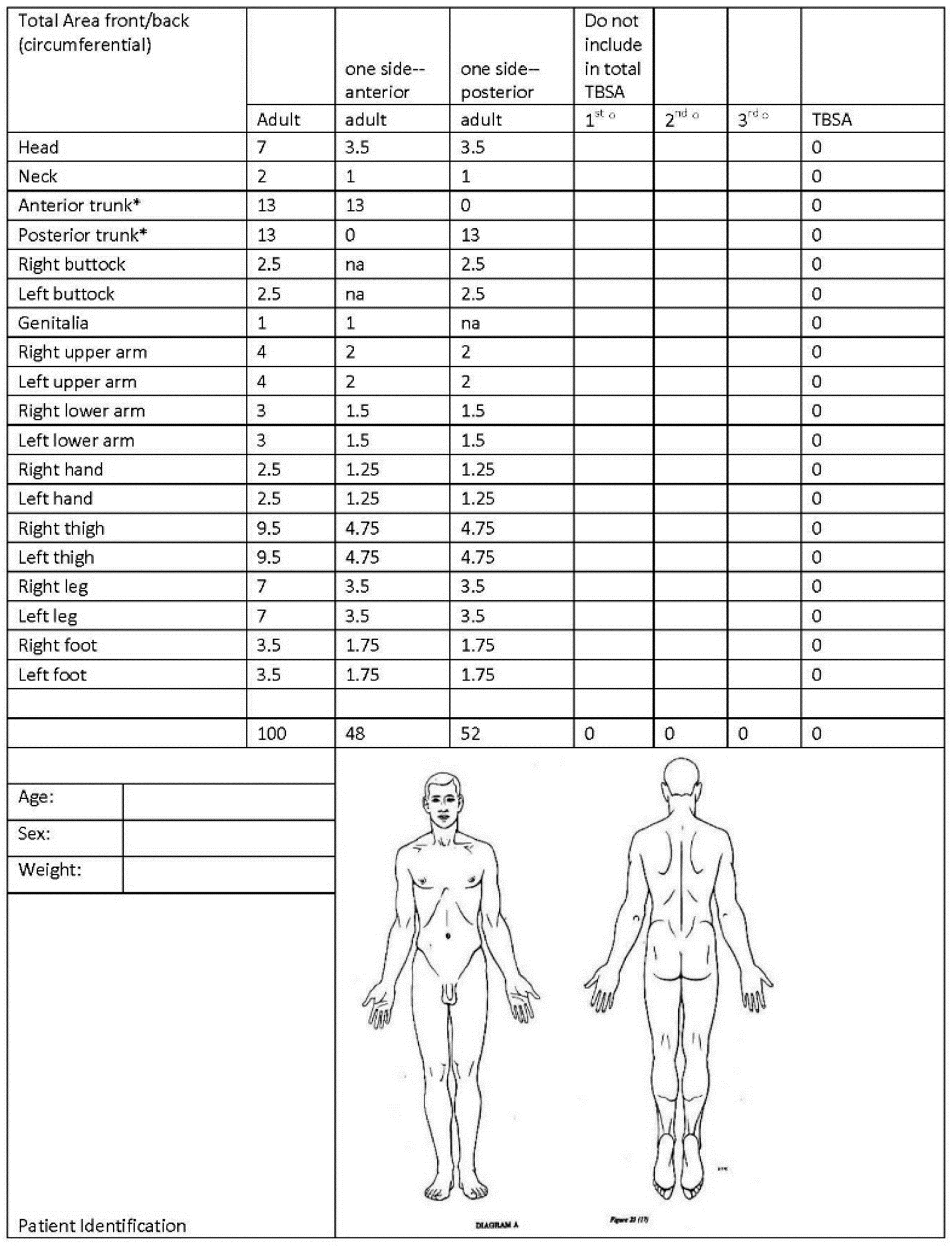
The acute management of severe burns is a critical phase that significantly influences the overall prognosis and survival of patients. Immediate and effective interventions are essential to mitigate the extensive physiological disruptions caused by burn injuries, which include fluid loss, electrolyte imbalance, infection risk, and systemic inflammatory response. One of the cornerstone principles in the acute management of severe burns is early and adequate fluid resuscitation. The Parkland formula, which estimates the amount of fluid required in the first 24 hours post-injury, remains a widely used guideline. This formula emphasizes the administration of isotonic crystalloids, typically lactated Ringer's solution, to restore circulatory volume and prevent burn shock, a life-threatening condition characterized by hypovolemia and reduced tissue perfusion (7). Calculation of the resuscitation includes calculating the total burn surface area (TBSA%) can also be done by using Lund–Browder charts (Figure 1). In addition to fluid resuscitation, the management of the burn wound itself is critical in the acute setting. Early excision of necrotic tissue and wound closure through skin grafting are strategies that have been shown to decrease the risk of infection, reduce the inflammatory response, and improve survival rates. Early excision, usually within the first week post-injury, helps limit the systemic effects of prolonged inflammation and reduces the risk of sepsis, which remains a leading cause of mortality in burn patients (8). This approach, however, requires careful patient selection and timing, as the physiological stress of surgery must be balanced against the patient’s ability to tolerate the procedure.
Pain management is another essential aspect of acute burn care, as inadequate pain control can lead to increased stress response, delayed wound healing, and long-term psychological sequelae. Multimodal analgesia, which includes the use of opioids, non-steroidal anti-inflammatory drugs (NSAIDs), and regional anesthetic techniques, is often employed to manage pain effectively. The use of patient-controlled analgesia (PCA) allows for individualized pain management and has been shown to improve patient comfort and satisfaction during the acute phase (10).
Moreover, addressing airway management is paramount, especially in cases of burns involving the face, neck, or inhalation injury, where the risk of airway obstruction is high. Early intubation is recommended in patients with significant inhalation injury or extensive facial burns to secure the airway before edema develops. The administration of high-flow oxygen and the use of bronchodilators may also be necessary to manage airway inflammation and bronchospasm. The acute management of severe burns requires a comprehensive and multidisciplinary approach that addresses fluid resuscitation, wound care, pain management, and airway protection. Early and aggressive intervention in these areas is crucial for improving outcomes and reducing the mortality associated with severe burns.
Long-Term Rehabilitation and Functional Recovery
Long-term rehabilitation following severe burns is a multifaceted process that focuses on restoring physical function, minimizing complications, and addressing the psychological impact of the injury. The complexity of burn injuries often necessitates an extended period of rehabilitation, which can include physical therapy, occupational therapy, and psychosocial support. The primary goal of long-term rehabilitation is to enhance the patient's quality of life by improving functional outcomes, preventing secondary complications, and facilitating reintegration into daily activities.
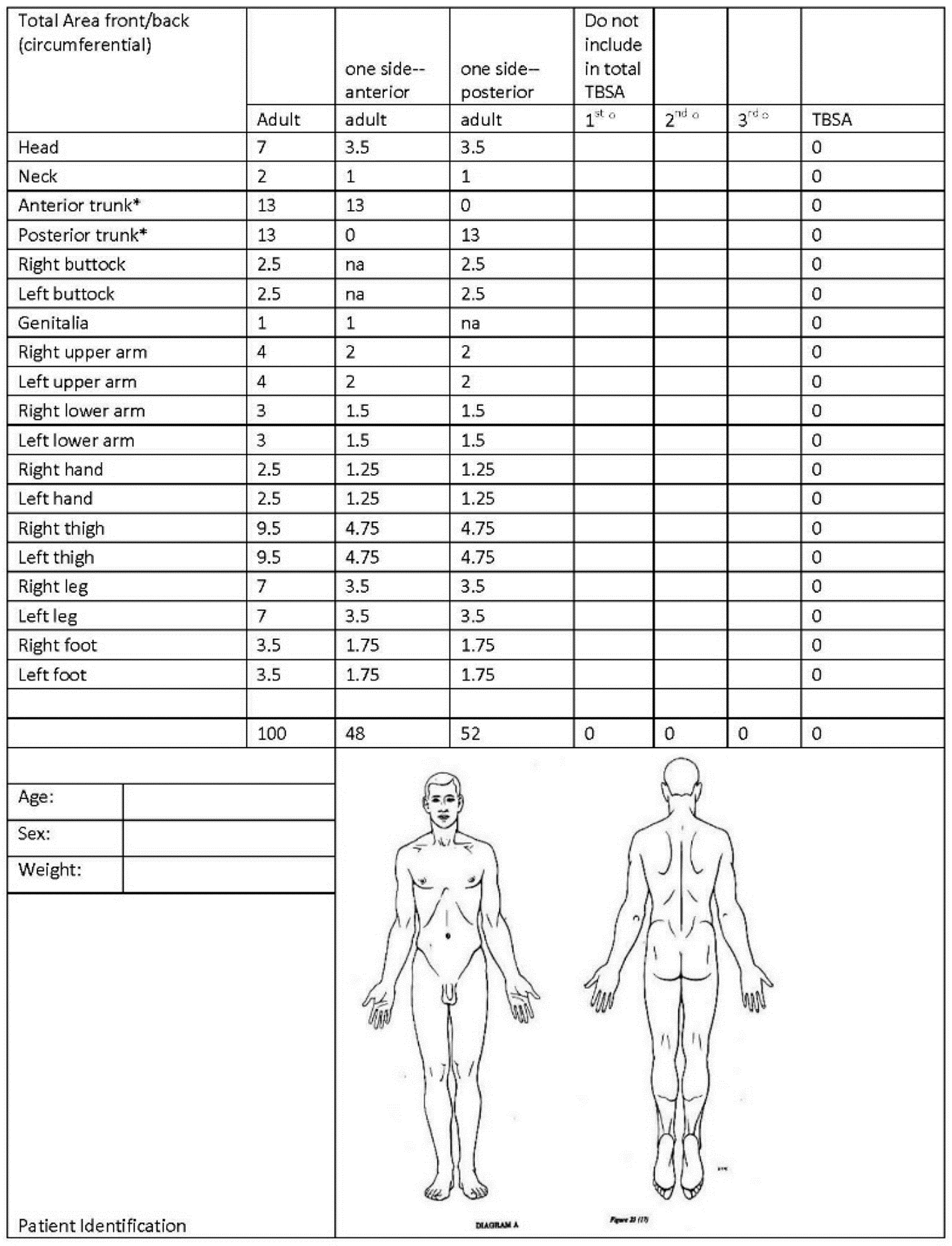
Figure 1: Lund–Browder Diagram used to document location of burns and to calculation of %TBSA (9).
One of the critical aspects of long-term rehabilitation is the management of contractures, which are a common complication in burn survivors. Contractures occur when scar tissue tightens and restricts the movement of joints, leading to functional impairment. Physical therapy plays a vital role in preventing and managing contractures through a combination of stretching exercises, splinting, and, in some cases, surgical intervention. Early initiation of physical therapy, often during the acute phase, has been shown to significantly reduce the incidence of contractures and improve functional outcomes in burn survivors (11). In addition to physical rehabilitation, occupational therapy is essential for helping patients regain independence in daily activities. Occupational therapists work with burn survivors to develop adaptive strategies and use assistive devices that facilitate the performance of activities of daily living (ADLs). This approach is particularly important for patients with severe burns involving the hands or other functional areas. By focusing on improving fine motor skills, enhancing strength and endurance, and promoting adaptive techniques, occupational therapy contributes to the overall functional recovery of burn survivors (12).
Psychosocial support is another crucial component of long-term rehabilitation. Burn injuries can have a profound psychological impact, leading to conditions such as PTSD, depression, and anxiety. The emotional and psychological challenges faced by burn survivors can hinder their recovery and affect their overall quality of life. Therefore, integrating mental health support into the rehabilitation process is essential. Cognitive-behavioral therapy (CBT), counseling, and peer support groups are commonly used interventions that help burn survivors cope with the emotional aftermath of their injuries and build resilience (13). Long-term rehabilitation and functional recovery in burn survivors require a comprehensive and individualized approach that addresses the physical, functional, and psychological aspects of recovery. Early and ongoing rehabilitation efforts, combined with a multidisciplinary team approach, are critical for optimizing outcomes and improving the quality of life for individuals who have suffered severe burns.
Grafting Techniques Utilized in Severe Burn Injuries
Grafting is a crucial intervention in the management of severe burn injuries, particularly for patients with extensive full-thickness burns where natural healing processes are inadequate to restore skin integrity. The choice of grafting technique depends on various factors, including the size, depth, and location of the burn, as well as the patient’s overall health and the availability of donor sites. Autografting, the transplantation of the patient's own skin, remains the gold standard for burn wound coverage due to its superior integration and lower risk of rejection. However, the limited availability of donor sites in patients with extensive burns necessitates the use of alternative grafting techniques (14).
Split-thickness skin grafts (STSGs) are commonly used in burn treatment and involve the removal of the epidermis and a portion of the dermis from a donor site, which is then transplanted to the burn wound (Figure 2). STSGs offer the advantage of covering large wound areas while preserving some dermal elements at the donor site, allowing for potential regrowth. Despite their effectiveness, STSGs may result in significant scarring and contracture, particularly in functional areas such as joints, which can impact the long-term mobility and quality of life of the patient (15).
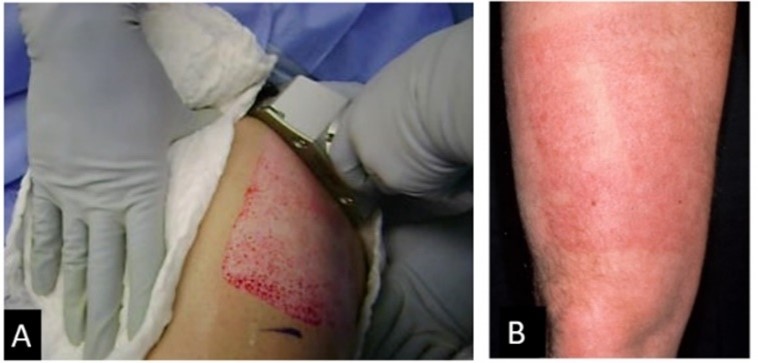
Figure 2: An example of split thickness skin graft: (A) Harvest of the skin graft with an electric dermatome. (B) Appearance at 3 months post-surgery. The wound was re-epithelialized in 10 days (16).
To mitigate these outcomes, the use of meshed grafts, where the graft is expanded to cover a larger area, can be employed. This technique also allows for drainage of exudates, reducing the risk of graft failure. In cases where donor skin is limited or unavailable, allografts and xenografts are alternative options. Allografts, which involve the use of cadaveric skin, and xenografts, which use animal skin (typically porcine), are often used as temporary biological dressings to protect the wound and promote granulation until autografting is possible. These grafts are eventually rejected by the body, but they provide a crucial temporary solution that can stabilize the wound environment and prevent infection (17).
Recent advancements in tissue engineering have led to the development of cultured epithelial autografts (CEAs) and biosynthetic grafts, which offer promising alternatives for patients with limited donor sites. CEAs involve the expansion of a small biopsy of the patient's skin in vitro to produce large sheets of epithelial tissue, which can then be grafted onto the burn wound. While this technique reduces the need for extensive donor sites, it is associated with challenges such as fragility of the grafts and longer healing times. Biosynthetic grafts, which combine biological and synthetic materials, aim to replicate the structure and function of human skin and have shown potential in improving wound healing and reducing scarring. Grafting techniques are essential in the treatment of severe burn injuries, with various options available depending on the specific needs of the patient. The choice of grafting method must balance the goals of wound coverage, functional recovery, and aesthetic outcomes, often requiring a multidisciplinary approach to optimize patient care.
Complications and Their Management in Severe Thermal Injuries
Severe thermal injuries are associated with a myriad of complications that can significantly impact patient outcomes and recovery. These complications often arise from the complex interplay between the extensive tissue damage caused by the burn and the body’s systemic response to the injury. Effective management of these complications is crucial to improving survival rates and enhancing the quality of life for burn survivors.
One of the most common and serious complications following severe thermal injuries is infection. Burn wounds, particularly those involving full-thickness burns, create an ideal environment for bacterial colonization and subsequent infection. Infections can range from localized wound infections to life-threatening systemic sepsis, which is a leading cause of mortality in burn patients. The disruption of the skin barrier, along with the immune suppression that often accompanies severe burns, predisposes patients to infections. The management of infections involves strict wound care protocols, including regular debridement, topical antimicrobial agents, and the use of systemic antibiotics when necessary (18). In addition, infection control measures, such as isolation procedures and sterile dressing techniques, are essential in preventing nosocomial infections.
Another significant complication of severe thermal injuries is the development of hypertrophic scars and keloids, which result from abnormal wound healing. These scars can lead to significant functional and cosmetic issues, particularly when they occur over joints or other areas where mobility is critical. The management of hypertrophic scars and keloids includes a combination of surgical and non-surgical approaches. Pressure garments, silicone gel sheets, and intralesional corticosteroid injections are commonly used to reduce scar formation and improve the appearance of the scar tissue (19). In more severe cases, surgical interventions such as scar revision or excision may be necessary, often followed by postoperative radiation therapy to minimize recurrence.
Metabolic disturbances are also a frequent complication of severe thermal injuries. The hypermetabolic response, characterized by increased energy expenditure, protein catabolism, and alterations in glucose metabolism, can persist for months following the injury. This state significantly impacts the patient’s nutritional status and wound healing ability. Nutritional support is a cornerstone of managing this complication, with enteral feeding preferred to ensure adequate caloric and protein intake. Pharmacological interventions, such as the use of beta-blockers to reduce hypermetabolism or anabolic agents to promote muscle preservation, have also been employed to counteract these metabolic challenges (20). The management of complications in severe thermal injuries requires a comprehensive approach that addresses the multifaceted nature of these challenges. By implementing rigorous infection control measures, utilizing effective scar management strategies, and providing adequate nutritional and metabolic support, healthcare providers can significantly improve the outcomes for burn survivors and enhance their long-term recovery.
Conclusion
The management of severe burns and thermal injuries is a complex process that extends from acute intervention to long-term rehabilitation, requiring a multidisciplinary approach to optimize patient outcomes. Addressing complications such as infection, scarring, and metabolic disturbances is crucial for improving survival rates and enhancing the quality of life for burn survivors. Continued research and advancements in burn care are essential to further refine these strategies and provide better support for patients throughout their recovery journey.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable
Consent for publications
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The author declare no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.