Volume 4, Issue 9
September 2024
Socio-Demographic Determinants as Predictors of Gingivitis in Children: A Systematic Review
Raed Mohammed Alamoudi, Amal Rasheed Alrashidi, Alemad Mustafa Kawthar, Amirah Ibrahim Alalawi, Alhnoof khalaf Alshammari, Waad Ahmad Alghamdi, Elaph Nassar Alahmdi, Mohammed Khalid Jawi, Mishal Saleh Alqasoumi, Ali Abdulfatah Albajhan, Nada Saeed Alzahrani
DOI: http://dx.doi.org/10.52533/JOHS.2024.40903
Keywords: socio-demographic, factors, gingivitis, children, impact
Oral health is directly linked to socioeconomic issues and socio-economic status is a significant predictor of periodontal disease, particularly gingivitis. Numerous studies have linked high rates of gingival bleeding to lower educational and economic levels. Additionally, periodontal disorders are linked to factors such as race, family size, income, and parental education level. This study aimed to assess various socio-demographic factors that may contribute as predictors of gingivitis among children. As a result, we included original studies published in last 11 years 2013-2024 only for latest evidence that recruited pediatric and adolescents i.e. young adults population aged from 0 to 17 years suffering from gingivitis. We analyzed a total of 9 studies, comprising data from 12,774 patients. The findings revealed a varied pattern, with two studies indicating a higher likelihood of gingivitis among females, while two others suggested males were at greater risk. Additionally, concerning age distribution, most studies highlighted an increased risk of gingivitis during adolescence or puberty, although one study reported contradictory results. Lower socio-economic status was consistently associated with higher odds of gingivitis across multiple studies, although only one study addressed the maternal occupation's impact on gingivitis. Through our assessment, we identified several risk factors contributing to the elevated prevalence of gingivitis among the study cohorts. These factors included malocclusion, inadequate oral hygiene practices such as irregular tooth brushing, as well as the presence of dental calculus and plaque. Findings revealed that factors such as age, socioeconomic status, and habitation significantly influence gingivitis prevalence. Gender distribution had a variable effect on gingivitis prevalence. The study highlights the need for further research, including longitudinal studies and intervention trials, to better understand these sociodemographic determinants and develop targeted interventions aimed at reducing gingivitis burden among children.
Introduction
Various gingival diseases affect children and can progress to harm the periodontium in adulthood. The onset of periodontal diseases often begins in earlier stages of life, manifesting later in adults. It is crucial for dental professionals to identify and diagnose gingival and periodontal diseases early to enhance treatment outcomes (1). Monitoring the status of teeth, periodontium, and oral mucosa is essential for overall health. In children and adolescents, the most common form of gingivitis is dental plaque-induced gingivitis, which is a reversible and non-destructive periodontal disease (2). In developed nations, the prevalence of gingivitis among children aged 6 to 11 is approximately 73%, with rates increasing as age advances within this range. Studies indicate a significant rise in gingivitis prevalence during puberty, ranging from 50% to 99%. Gender differences are observed, with boys exhibiting higher prevalence rates, possibly attributed to variations in oral hygiene practices (1).
Periodontal diseases are of significant public health concern due to their high prevalence rates and profound societal impact. Recent research has established an association between these diseases and overall population health. Dental plaque is recognized as a key contributor to the initiation and advancement of periodontal diseases. This biofilm, composed of diverse microorganisms, accumulates on oral surfaces. The buildup of plaque at the gum line triggers inflammation, leading to gingivitis. Gingivitis is characterized by redness, swelling, and bleeding upon probing, without apparent loss of bone or tooth support structures. Fortunately, gingivitis can be reversed with appropriate treatment, preserving oral health. However, if left unaddressed, it can progress to periodontitis, causing irreversible damage to the bone surrounding the teeth and potentially resulting in tooth loss. Additionally, gingival inflammation can release inflammatory mediators into the bloodstream, potentially impacting overall health negatively (3).
Gingival tissue exhibits increased sensitivity to plaque biofilm, with gingival inflammation potentially exacerbated in adolescents during puberty. Elevated levels of sex hormones in circulation are linked to increased gingival inflammation. Factors such as oral health practices, gender, oral hygiene, the presence of dental calculus, and socioeconomic status also contribute to the risk of gingivitis (4). It has been proven that infrequent tooth brushing and a high intake of sugary foods have been associated with increased severity and extent of periodontal inflammation. Conversely, periodontal inflammation and bleeding impair the capacity to clean the teeth efficiently. Studies also suggest that various variables such as an unhealthy diet, the absence of oral and dental hygiene habits, and insufficient awareness among families and children, have increased the prevalence of poor oral hygiene status and gingivitis in children (5).
Oral health is directly linked to socioeconomic issues, which influence knowledge, attitudes, and behaviors. Disparities in caries and gingivitis have been linked to oral hygiene behaviors and fluoride use among social strata. Demographic and sociological factors can impact diet, namely the amount of sugar consumed (6). Moreover, socioeconomic status is a significant predictor of periodontal disease, particularly gingivitis. Numerous studies have linked high rates of gingival bleeding to lower educational and economic levels. Additionally, periodontal disorders are linked to factors such as race, family size, income, and parental education level. While socioeconomic indicators include low father income, limited education up to primary school, and a lack of car ownership, periodontal attachment loss can lead to necrotizing ulcerative gingivitis. Access to school dental services may also affect gingival scores (7). Evidence has been established about the association between social determinants and several oral health issues, dental treatment utilization, and oral health habits (8).
Sociodemographic factors such as socioeconomic status, education level of parents, and access to dental care can influence a child's risk of developing gingivitis. By identifying these factors, public health initiatives can be designed to promote preventive measures like oral hygiene education, regular dental check-ups, and access to affordable dental care. Furthermore, understanding sociodemographic factors can help pinpoint which groups of children are most vulnerable to gingivitis. This information allows for targeted interventions to be developed to reach those who need them most. Researching sociodemographic factors can shed light on health inequalities related to gingivitis. It can highlight disparities in oral health outcomes among different socioeconomic groups and inform policies aimed at reducing these inequities. Hence, studying sociodemographic factors related to gingivitis among children is essential for developing targeted interventions, reducing health inequalities, and promoting better oral health outcomes for all children. Therefore, we aim to conduct this systematic review to elaborately study the influence of socio-demographic factors on the incidence of gingivitis among children using evidence from existing literature.
Methods
Definition of Outcomes and inclusion criteria
Our study aimed to assess various socio-demographic factors that may contribute as predictors of gingivitis among children. As a result, we included original studies that recruited pediatric and adolescents, i.e., young adults aged from 0 to 17 years, suffering from gingivitis. Additionally, we included studies published in the last 11 years (2013–2024) only for the latest evidence. The exclusion criteria comprised studies that involved children with systemic conditions such as diabetes or immunodeficiency disorders, which are known to influence gingival health. This was done to separate the effects of socio-demographic factors from other health-related variables. Also, studies mentioning children undergoing orthodontic treatment were excluded as they may affect gingival health and confound the results. Moreover, this review excluded case reports featuring small sample sizes and lacking descriptive statistics. Nonhuman or laboratory studies, non-original or incomplete investigations, abstract-only articles, protocols, theses, and articles not published in English or lacking English information were also excluded based on predetermined criteria.
Search Strategy
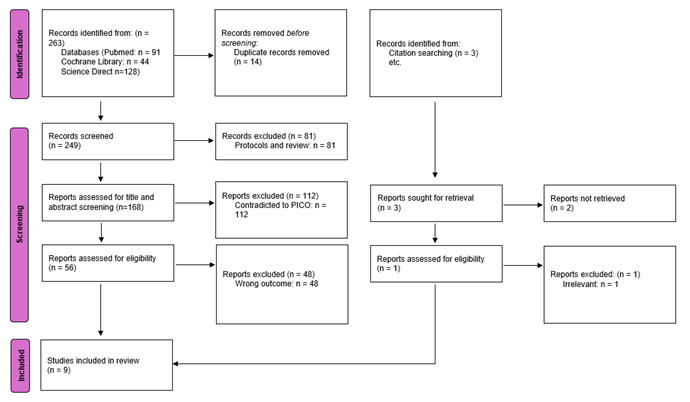
After achieving our desired outcomes, we conducted a brief manual screening of potential studies to extract relevant keywords for crafting an optimal search query. Our search strategy encompassed terms such as (gingivitis OR ‘gingival inflammation’ OR ‘gingival health’) AND (socio-demographic OR demographics OR ‘social factors’ OR ‘risk factors’) AND (children OR pediatrics OR adolescents). We utilized PubMed, Science Direct, and the Cochrane Library as our databases for the search. To ensure inclusivity of pertinent research, we limited our search to the titles and abstracts of retrieved results. Subsequently, we employed EndNote software to compile and eliminate duplicates across all databases. Additionally, we manually scrutinized the reference lists of included studies, related reviews, and relevant sections of comparable articles in PubMed to identify any potentially overlooked papers. Throughout this systematic review, we adhered to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Screening and extraction
Articles with irrelevant titles were excluded from consideration. In the subsequent phase, both the full text and abstracts of papers were meticulously reviewed to determine their compliance with the inclusion criteria. To streamline the process, titles and abstracts were organized, assessed, and scrutinized for any duplicate entries using reference management software (Endnote X8). To ensure the highest quality of selection, a dual screening approach was adopted, involving one screening for the evaluation of titles and abstracts and another for the comprehensive examination of the entire texts. Once all relevant articles were identified, a structured extraction sheet was created to capture pertinent information aligned with our specific objectives. This included delineating the desired outcomes and baseline characteristics such as study design and period, age, gender, and the geographical location of the study.
Quality Assessment
We collected data from the encompassed studies to evaluate the potential bias they might entail. For assessing the quality of observational studies, we employed the modified Newcastle-Ottawa Scale, encompassing four domains: methodological quality, comparability, outcome/exposure assessment, and outcome/exposure reporting. Each study was rated on a scale from 0 to 10 according to the extent of bias, categorized as excellent, good, satisfactory, or unsatisfactory.
Results
Search Results
We executed the search methodologies outlined previously, resulting in the identification of a total of 263 citations, which were subsequently reduced to 249 following the removal of duplicates. Upon screening titles and abstracts, only 56 citations met the eligibility criteria for further consideration. Through full-text screening, this number was further refined to 8 articles aligning with our inclusion and exclusion criteria. Additionally, one eligible study was identified from the reference search. Hence, a total of 9 studies were included in the final review. Figure 1 provides an in-depth depiction of the search strategy and screening process.
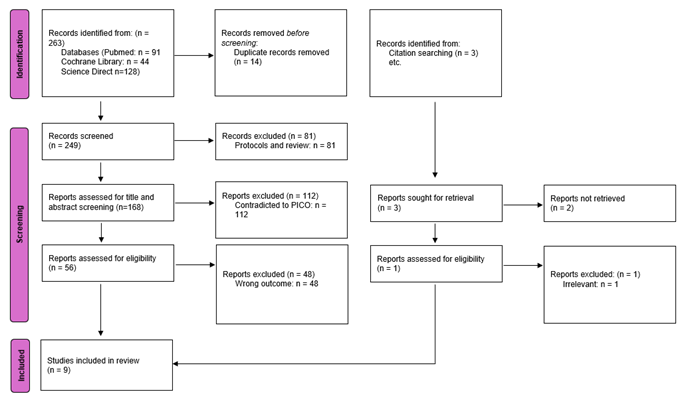
Figure 1: PRISMA flowchart
Results of Quality Assessment
Upon evaluating the quality of the studies included, it was determined that overall, the studies exhibited good quality with minimal risk of bias, and only one of the included studies had satisfactory quality. The detailed findings of the quality assessment are presented in Table 1.
|
Table 1. Quality assessment of Newcastle–Ottawa scale (NOS) for included studies. |
|||||
|
Study |
Selection |
Comparability |
Outcome |
Total Score |
|
|
Shailee FG, et al. (9) |
3 |
0 |
3 |
6 |
|
|
Kaur A, et al. (10) |
3 |
1 |
3 |
7 |
|
|
Gopinath VK, et al. (11) |
3 |
2 |
3 |
8 |
|
|
Agbaje HO, et al. (12) |
4 |
2 |
3 |
9 |
|
|
Hoffmeister L, et al. (13) |
4 |
2 |
3 |
9 |
|
|
Bashirian S, et al. (5) |
4 |
2 |
3 |
9 |
|
|
Chrysanthakopoulos NA. (14) |
4 |
2 |
3 |
9 |
|
|
Sharma N, et al. (15) |
4 |
2 |
3 |
9 |
|
|
Liu X, et al. (16) |
4 |
2 |
3 |
9 |
|
Characteristics of the included studies
We incorporated a total of 9 studies encompassing 12,774 patients, published between 2013 and 2024 (5, 9-16). The age range of participants varied from 1 year to 19 years, with the majority being male. Notably, all the studies were cross-sectional in nature. Geographically, three studies originated from India, followed by each study from China, the United Arab Emirates, Iran, Europe, South America, and Africa. A comprehensive summary of the baseline characteristics of these studies can be found in Table 2. Discrepancies in sample sizes across the included papers likely stem from differences in study objectives and inclusion criteria.
|
Table 2. Baseline characteristics of included studies |
|||||||||
|
Author |
Journal publisher |
Country |
Year |
Study design |
Study period |
Total participants |
Age range |
Gender |
Funding |
|
Shailee FG, et al. (9) |
J Int Soc Prev Community Dent |
India |
2013 |
Cross sectional |
2009 |
1011 |
12 and 15 years |
61.92%/38.08% |
NR |
|
Kaur A, et al. (10) |
Indian Journal of Dental Research |
India |
2014 |
Cross sectional |
NR |
1269 |
5,12 and 15 years |
NR |
NR |
|
Gopinath VK, et al. (11) |
European Journal of Dentistry |
UAE |
2015 |
Cross-sectional |
2011 -2013 |
405 |
3–6 years and 6–12 years |
57%/ 43% |
NR |
|
Agbaje HO, et al. (12) |
Journal of periodontology |
Africa |
2016 |
Cross-sectional study |
2013 |
992 |
1-12 years |
51.2%/48.8% |
Self- sponsored |
|
Hoffmeister L, et al. (13) |
Elsevier Espana |
South America |
2016 |
Cross-sectional |
2009-2010 |
2,987 |
2 and 4 years |
NR |
The Ministry of Health of Chile contributed to the accomplishment of this work |
|
Bashirian S, et al. (5)
|
PLOS ONE |
Iran |
2018 |
Cross sectional |
2016 |
988 |
7–12 years |
50.91%/49.09% |
Hamadan University of Medical Sciences, grant number: IR.UMSHA.REC.1394.473. |
|
Chrysanthakopoulos NA. (14) |
European Journal of General Dentistry |
Europe |
2021 |
Cross sectional |
2013 -2014 |
812 |
13-16 Years |
47.29%/52.71% |
NIL |
|
Sharma N, et al. (15) |
Journal of Indian Association of Public Health Dentistry |
India |
2021 |
Cross sectional |
2019-2020 |
1400 |
6–19 years |
47.7%/ 52.3% |
Uttarakhand Council of Science and Technology, Dehradun. |
|
Liu X, et al. (16) |
BMC oral health |
China |
2022 |
Cross sectional |
2021 |
2880 |
6–12 years |
52.64%/47.36% |
received no specific grant from any funding agency in the public, commercial, or not for profit sectors. |
NR: not reported
Study outcome measures
Various socio demographic factors were assessed and analyzed in correlation with the prevalence of gingivitis among the included studies (Table 3a). A study by Shailee et al. demonstrated that at age 12, gingivitis rates were higher compared to those at age 15. Private school children exhibited a greater proportion of healthy gums than their counterparts in government schools. Additionally, females demonstrated a higher level of gingival health compared to males across both age groups (9). While Kaur et al. noted that the incidence of gingivitis was markedly greater among 5-year-old children (67%) and those aged 15 (98%) living in rural regions (10). Findings of the study by Gopinath et al. reported that children aged 6 years or younger had a significantly reduced likelihood of gingivitis compared to those older than 6 years (OR: 0.33, 95% CI: 0.17-0.62, p = 0.00). Furthermore, males exhibited a lower likelihood of gingivitis according to logistic regression analysis (OR: 0.47, 95% CI: 0.24-0.93, p = 0.03) (11). Results of a study by Agbaje et al. indicated that for children aged 1 to 5 years, the odds ratio of gingivitis was 0.21 with a 95% confidence interval (CI) of 0.14 to 0.31, indicating a highly significant association (p < 0.001). There was no notable correlation found between gender and gingivitis. However, individuals from a low socioeconomic background demonstrated increased odds of gingivitis, with an adjusted odds ratio of 2.09 and a 95% CI of 1.32 to 3.31 (p = 0.002) (12). Hoffmeist et al. observed that in the 4-year-old age group, there was a correlation between gingivitis and the DMFT index, with a prevalence ratio of 1.64 and a 95% CI of 1.28 to 2.09 (13). Moreover, a study by Bashirian et al. depicted that gingival bleeding exhibited an odds ratio of 1.44 with a 95% CI of 1.31 to 1.59, indicating a highly significant association (p < 0.001). Children residing in urban areas showed a lower odds ratio (OR: 0.69) with a 95% CI of 0.51 to 0.93 (p = 0.01) for gingival bleeding. Boys had a higher odds ratio (OR: 1.54) with a 95% CI of 1.16 to 2.06 (p = 0.003) for experiencing gingival bleeding. Regarding maternal employment status, those who were not employed had an odds ratio of 0.55 with a 95% CI of 0.29 to 1.05 (p = 0.07), while self-employed mothers had an odds ratio of 0.40 with a 95% CI of 0.18 to 0.86 (p = 0.02) for gingival bleeding in their children (5). A stepwise logistic regression analysis by Chrysanthakopoulos NA. revealed several predictors of gingivitis. Males had an odds ratio of 1.511 with a 95% CI of 1.014 to 2.252, indicating a significant association (p = 0.042*). Low education levels were associated with an increased odds ratio (OR=1.890) and a 95% CI of 2.421 to 2.881 (p = 0.003*). Additionally, individuals with low-income levels exhibited a higher odds ratio (OR=2.123) with a 95% CI of 1.368 to 3.300 (p = 0.001*) (14). While Sharma et al. observed in their findings that gingivitis was more prevalent among children older than 12 years, with a rate of 23.3%, compared to younger children, who had a prevalence of 15.6%. There were no significant differences observed in the occurrence of gingivitis between boys and girls. However, among children in classes 4 and 5, the frequency of gingivitis was higher, with an adjusted odds ratio of 1.48 and a 95%CI of 1.10 to 2.00 (p = 0.010) (15). while Liu et al. noted that the age range of 6-12 years demonstrated a notable influence on the occurrence of gingivitis, with a prevalence of 28.58%, indicating a significant disparity (p < 0.05). The odds ratio was determined to be 1.132, with a 95% CI spanning from 1.063 to 1.206, and a p-value of 0.000 (16).
|
Table 3a. Socio demographic determinant of included studies |
|||||
|
Author |
Socio demographic determinant |
||||
|
Age |
Residence district |
Gender |
Mothers’ occupation |
Socio Economic Status |
|
|
Shailee FG, et al. (9) |
Gingivitis was higher at the age of 12 years as compared with 15 years |
Children in the private schools had a higher proportion of healthy gingival as compared with government schools |
Females had higher level of healthy component of gingiva than males at both the ages |
NR |
NR |
|
Kaur A, et al. (10)
|
NR |
The results showed that the percentage of children affected with gingivitis was significantly higher in the rural areas in 5 years (67%) and 15-year-old children (98%) |
NR |
NR |
NR |
|
Gopinath VK, et al. (11) |
children aged ≤6 years were 3.06 times less likely to have gingivitis than those aged >6 years (OR: 0.33), 95% CI: (0.17-0.62), P = 0.00 |
NR |
A logistic regression analysis of the predictors of gingivitis showed that males (OR):0.47,95%[CI]:0.24-0.93, P = 0.03) |
NR |
NR |
|
Agbaje HO, et al. (12) |
Age: 1 – 5 years, (OR:0.21) 95%CI: (0.14 -0.31), P=<0.001 |
NR |
no significant relationship between gender |
NR |
low socioeconomic status (AOR: 2.09; 95% CI:(1.32 – 3.31); p=0.002). |
|
Hoffmeister L, et al. (13) |
4 years age group, gingivitis was associated with the DMFT index (PR = 1.64) 95%CI:( 1.28-2.09). |
NR |
NR |
NR |
NR |
|
Bashirian S, et al. (5)
|
Gingival bleeding:(OR 1.44)95% CI (1.31–1.59), P=<0.001 |
children living in the urban areas: (OR:0.69), 95% CI: (0.51–0.93), P=0.01 |
gingival bleeding for boys: (OR:1.54)95%CI: (1.16–2.06), P=0.003 |
•mothers not employed: (OR=0.55), 95%CI:(0.29–1.05), P=0.07. •mothers’ self-employed: (OR= 0.40),95%CI: (0.18–0.86), P= 0.02 |
NR |
|
Chrysanthakopoulos NA. (14) |
NR |
NR |
A stepwise logistic regression analysis of the predictors of gingivitis showed that males: (OR =1.511),95%CI (1.014-2.252), P=0.042* |
Education level low: (OR=1.890),95%CI: (2.421-2.881), P=0.003* |
Income level low: (OR=2.123),95%CI:( 1.368-3.300), p=0.001* |
|
Sharma N, et al. (15) |
Gingivitis was more frequent among children >12 years, 23.3% as compared to the younger children (15.6%) |
NR |
no significant differences in the prevalence of gingivitis among the boys and girls |
NR |
The frequency of gingivitis was more among children of class 4 and 5:(AOR 1.48),95%CI:(1.10–2.00), (P = 0.010) |
|
Liu X, et al. (16) |
Age 6-12 years had a statistically significant effect on the prevalence of gingivitis (28.58%), with a statistically significant difference (P < 0.05). (OR=1.132),95%CI:(1.063-1.206), P=0.000 |
NR |
NR |
NR |
NR |
NR: not reported, OR: adjusted odds ratio, CI: confidence interval, DMFT: the sum of the number of Decayed, missing due to caries, and Filled Teeth in the permanent teeth, PR: prevalence ratio
Furthermore, among the included studies, we analyzed certain risk factors that may contribute to the incidence of gingivitis (Table 3b). Shailee et al. considered that the increased prevalence of malocclusion among 12-year-olds (58.1%) compared to 15-year-olds (53.5%) might have raised the risk of gingivitis in this population (9). Kaur A et al. noted that children who brushed their teeth once daily showed a greater prevalence of gingivitis compared to those who brushed more than once per day across all age groups (10). Bashirian et al. reported that higher percentage of the boys in the age group of 12 years old had periodontal bleeding (52.9%) (5). A study by Chrysanthakopoulos NA. showed that insufficient oral hygiene practices, including daily tooth brushing, were associated with increased odds of oral health issues, with an odds ratio of 4.202 and a 95% CI of 2.674 to 6.579 (p = 0.000) (14). Similarly, lack of dental floss use demonstrated a higher odds ratio of 2.604 and a 95% CI of 1.543 to 4.386 (p = 0.000). Additionally, smoking was linked to a higher odds ratio of 2.26 with a 95% CI of 1.433 to 5.348 (p = 0.000). Furthermore, Sharma et al. stated that malocclusion showed a significant association with an odds ratio of 2.9 and a 95% CI of 2.18 to 3.82 (p = 0.000). Children who brushed their teeth occasionally during the week had a 1.5 times higher likelihood of experiencing gingivitis compared to those who brushed daily, with an adjusted odds ratio of 1.47 and a 95% CI of 1.10 to 1.96 (p = 0.009). Moreover, children whose main staple food was rice had twice the likelihood of developing gingivitis compared to those who consumed wheat, with an adjusted odds ratio of 1.85 and a 95% CI of 1.27 to 2.71 (p = 0.001) (15). while a binary logistic regression analysis by Liu et al. showed that dental calculus, plaque, and dental crowding were significantly associated with a high prevalence of gingivitis (16).
|
Table 3b. Other risk factors of included studies |
|
|
Author |
predictors of associated risk factors |
|
Shailee FG, et al. (9) |
The prevalence of malocclusion among the 12- year-old (58.1%) was more as compared with that among the 15-year-old (53.5%) |
|
Kaur A, et al. (10)
|
The children who brushed once a day had higher prevalence of gingivitis as compared to children who brushed more than once per day in all the age groups |
|
Gopinath VK, et al. (11) |
NR |
|
Agbaje HO, et al. (12) |
NR |
|
Hoffmeister L, et al. (13) |
NR |
|
Bashirian S, et al. (5) |
Higher percentage of the boys in the age group of 12 years old had periodontal bleeding (52.9%) |
|
Chrysanthakopoulos NA. (14) |
Inadequate oral hygiene: Daily tooth?brushing: (OR=4.202), 95%CI: (2.674-6.579), P=0.000* Dental floss use: (OR=2.604),95%CI:( 1.543-4.386), P=0.000* smoking: (OR=2.26),95%CL: (2 1.433-5.348), P=0.000* |
|
Sharma N, et al. (15) |
Malocclusion: (OR=2.9),95%CI: (2.18-3.82), P=0.000 Children who brushed sometimes in a week were 1.5 times more affected by gingivitis than those who brushed daily (AOR =1.47), 95%CI:(1.10–1.96), P = 0.009 Children consuming rice as a main staple food had two times more chances of being affected by gingivitis than the children consuming wheat (AOR= 1.85), 95%CI:(1.27–2.71), P = 0.001 |
|
Liu X, et al. (16) |
binary logistic regression analysis showed that dental calculus, plaque, and dental crowding were significantly associated with a high prevalence of gingivitis |
NR: not reported, OR: adjusted odds ratio, CI: confidence interval
Discussion
This study aimed to analyze the influence of diverse socio-demographic characteristics, including age, gender, population habitation (urban or rural), mother's occupation, and socio-economic status, on the prevalence of gingivitis among children. Findings exhibit a variable trend, as two of the studies observed a higher probability of gingivitis among females, while another two studies observed that males were at higher risk of suffering from gingivitis. Moreover, regarding the age distribution, the majority of the studies reported that the higher risk of gingivitis was associated with increasing age, like in the in the teenage years; however, one study reported the contrary findings. Higher odds of gingivitis were related to low socio-economic status, while only one of the included studies discussed gingivitis as an aspect of a mother's occupation.
Similar to our findings, Fan et al. demonstrated in their findings that the weighted prevalence of gingivitis among children aged 12 to 15 was 29.6%, with 22.6% having localized gingivitis and 7.0% having generalized gingivitis. The prevalence of gingivitis varied by age. According to the multivariate logistic regression analysis results, characteristics such as growing age, being the only child, missing regular annual dental check-ups, and having extensive dental calculus were strongly related to the higher prevalence of gingivitis. Furthermore, the association of gingivitis with these characteristics differed between urban and rural areas (4). Another cross-sectional study from Tanzania showed that the prevalence of gingivitis was 56.6% among 15–17-year-olds in comparison to 12–14-year-olds, where the prevalence was 38.8%. Adolescents born in the Arusha region and older age groups had a 2.0-times (OR = 2.0, CI 1.2–3.3) and 1.6-times (1.0–2.5) higher risk of gingival bleeding than those born outside Arusha and younger age groups (17). While a Romanian cross-sectional study depicted that the gingival scores indicated mild inflammation and gingivitis was prevalent at 91%, Boys showed higher gingival (0.19 vs. 0.18; p < 0.05) and plaque scores (0.71 vs. 0.59; p < 0.01) compared to girls. Children who did not live in overcrowded families, whose parents had a higher education, and had direct access to school dental services had better gingival conditions (p < 0.05). Gingivitis was more severe on the upper teeth, with the highest score achieved at the right upper lateral incisor; 0.63 on distal surface (7). Results of a Yemini cross-sectional study showed that the 12-year-old children had significantly greater mean plaque index, calculus index, and gingival index (P < 0.001), with 78.6% presenting with gingivitis and 47.8% with mild gingivitis. In comparison, the values were 27.2% and 3.1% in the younger group (P < 0.001). There were considerable differences depending on gender, area of residence, and governorate. Regression analysis revealed that mean plaque index (OR = 35), mean calculus index (OR = 7.7), male gender (OR = 1.6), living in rural regions (OR = 1.4), and belonging to Hajjah or Sana'a were independent risk variables for gingivitis severity in the older group (18). It has been reported that marginal gingivitis occurs in childhood, increases in prevalence and severity at puberty, and then gradually declines throughout the second decade of life (19).
Our findings are in accordance with these findings of the literature, as our results signify the linear increasing trend of age and gingivitis, with only one included study reporting contrary findings. However, similar to this, another retrospective study concluded that pediatric patients have a high prevalence of gingivitis, although there is no significant association between age, gender, and gingivitis severity (20). This disparity and diverse gender distribution of the prevalence of gingivitis observed in our study emphasizes the necessity for further investigation, particularly through systematic reviews and meta-analyses, to offer comprehensive, evidence-based insights into this matter. Furthermore, in our review, we identified and assessed certain risk factors that may contribute to the increased prevalence of gingivitis among the study cohort. The primary risk factors identified among the included studies were malocclusion and inadequate oral hygiene practices such as infrequent brushing of teeth, while others were dental calculus, plaque, and consumption of rice as a staple food.
Similarly, Kolawole et al. reported that the significant factors related to gingivitis were poor dental hygiene (p < 0.001), increased overjet (p = 0.003), and anterior open bite (p = 0.014) (21). Additionally, Salim et al. concluded that malocclusion could increase the risk of caries and periodontal disease; the magnitude of this risk grows exponentially among groups with poor oral health and limited access to oral healthcare services (22). A study by Kyaw et al. demonstrated that the mother's occupation, tooth brushing frequency, consumption of sugary drinks, oral hygiene practice, and bacterial levels in dental plaque were significant predictors of gingivitis (23). In our review, only one of the included studies by Bashirian et al. discussed the risk of gingivitis with respect to a mother's occupation; they highlighted that children of self-employed mothers have a significantly lower likelihood of experiencing gingival bleeding compared to mothers of different employment statuses (5). Another study, in our review by Chrysanthakopoulos, observed that the lower educational level of the mother was significantly associated with higher odds of gingivitis (14).
Moreover, children residing in rural areas and belonging to low-socioeconomic levels had a higher risk of gingivitis. This may be explained in the context of inadequate oral hygiene practice due to limited resources and knowledge among these cohorts. Similarly, Almajed et al. highlighted in their review findings that lower socioeconomic status is linked to worse oral health outcomes for children, driven by factors such as parental education, home income, food security, and community environment (24). A recent study from Saudi Arabia noted that in rural areas, a higher percentage of children reported better gum health compared to those in urban areas (48.2% versus 41.3%, respectively). Pain emerged as the primary motivator for seeking dental care in rural regions, with 55.7% citing it as the reason for their dental visit, compared to 54.5% in urban areas. Notably, sugar consumption was notably higher among rural children. Despite this, the majority of children in both settings maintained oral hygiene by using a toothbrush and toothpaste. However, dental appointments were not routine; rather, they were sought primarily in response to toothaches (25). Although they reported better oral health among children in rural areas, contrary to our findings, they did not define the risk of gingivitis.
In our review, inadequate brushing of the teeth was associated with a higher risk of gingivitis. Maintaining oral health and preventing conditions like periodontal disease and dental caries can be achieved through consistent daily plaque removal. Tooth brushing stands out as the most widely practiced and effective method to uphold oral hygiene. It should be ingrained as a routine, ideally performed twice daily, in the morning and evening. Apart from enhancing oral cleanliness and warding off periodontal disease, brushing with fluoride toothpaste also fortifies teeth against decay. The habits formed during youth, including oral care routines, can significantly impact both immediate and long-term health outcomes. Many behavioral patterns are established early in life, making oral hygiene practices a crucial component of an individual's lifestyle (26). Folayan et al. also concluded that the daily use of fluoridated toothpaste appears to reduce the risk of moderate/severe gingivitis (27). This systematic review delves deep into the intricate relationship between socio-demographic factors and gingivitis prevalence among children, presenting a comprehensive understanding of the topic. A notable strength lies in the inclusion of studies conducted within the last decade, ensuring the relevance and currency of the evidence presented. Moreover, our emphasis on high-quality research adds rigor and credibility to our findings, enhancing the trustworthiness of the conclusions drawn. Additionally, our meticulous search methodology, coupled with the thorough analysis of relevant keywords, further strengthens the robustness of this study. By systematically synthesizing the latest evidence from the literature, we offer valuable insights into the multifaceted influences shaping gingivitis outcomes in children, thus contributing to the advancement of knowledge in the field of pediatric oral health.
Limitations and future research directions
Our review is subject to certain limitations. Primarily, the study conducted by Sharma et al. (15), which encompassed a study population up to the age of 19 years (study population aged 6-19 years), exceeded the age criteria outlined in our inclusion criteria. However, we opted to include this study to ensure comprehensive coverage of the available evidence in the current literature defining the pediatric population. Additionally, despite efforts to include high-quality studies, variations in study methodologies and definitions of socio-demographic factors may introduce heterogeneity into the analysis, limiting the comparability of findings across studies. Moreover, the exclusion of non-English language studies may introduce language bias and overlook relevant research conducted in other languages. Furthermore, the reliance on available literature may overlook unpublished or grey literature sources, potentially omitting valuable data.
Future research directions for understanding gingivitis incidence among children include a multifaceted approach. Longitudinal studies would provide crucial insights into the progression of gingivitis over time and how socio-demographic factors contribute to its development. Intervention trials targeting various socio-demographic groups can help identify effective strategies for reducing gingivitis prevalence. A qualitative exploration of cultural and access-related influences would shed light on the underlying social determinants affecting oral health behaviors and outcomes. Gender-specific analysis would help discern any disparities in gingivitis prevalence and risk factors. Examination of geographical variations would highlight regional differences in gingivitis prevalence and associated factors. Investigations into health equity would aim to address disparities in oral health outcomes across different socio-demographic groups. Multifactorial analyses would allow for a comprehensive understanding of how various factors interact to influence gingivitis incidence. Ultimately, these research endeavors aim to inform targeted interventions tailored to different populations, thereby mitigating the burden of gingivitis and improving oral health outcomes on a broader scale.
Conclusion
This study investigated the impact of various sociodemographic factors on gingivitis incidence in children. Findings revealed that factors such as age, socioeconomic status, and habitation significantly influence gingivitis prevalence. Adolescents, rural residents, and those from low socioeconomic backgrounds were found to be at higher risk. Gender distribution had a variable effect on gingivitis prevalence. Additionally, risk factors like malocclusion, poor oral hygiene, and dental plaque were identified as contributors to gingivitis incidence. The study highlights the need for further research, including longitudinal studies and intervention trials, to better understand these sociodemographic determinants and develop targeted interventions aimed at reducing gingivitis burden among children.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable
Consent for publications
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The author declares no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not Applicable