Volume 4, Issue 9
September 2024
Venous Varix of the External Jugular Vein: A Case Report
Fahad Almalki, Samaher Alnefaie
DOI: http://dx.doi.org/10.52533/JOHS.2024.40901
Keywords: Venous varix, dilations, jugular vein, thorax
Background: Venous dilations of the jugular veins are uncommon and external jugular varix even rarer. Venous varices arise with arteriovenous malformations, developmental venous anomalies and rarely as singular lesions. Most commonly, they appear as focal dilatations of the venous drainage of arteriovenous malformations. The preliminary diagnosis of venous varix is usually incorrect or overlooked due to inadequate clinical evaluation. Therefore, either imaging studies or histopathological analysis are crucial for concluding at the definitive diagnosis. However, the documented instances of venous varix in literature are scarce, with even fewer references regarding its investigative approaches and treatment modalities. We present here a unique case of external jugular vein varix in a female patient diagnosed at our clinic.
Case presentation: A 29-year-old female patient presented to the department of ENT with complaint of right neck swelling for the past three years. There was no significant medical and surgical history. Her physical examination was unremarkable, except for a soft, compressible mass lateral to the sternocleidomastoid muscle, which became more prominent whilst performing the Valsalva maneuver. The initial X-ray performed did not show any air-filled sac or soft tissue mass that could define the cause for the swelling on straining. Hence the patient was then referred for ultrasound scan of the neck which showed a thin walled, compressible, cystic lesion in the right side of the neck, which was confirmed upon doppler study as dilation of the lower third of the right external jugular vein. A computed tomography scan of the neck and thorax further performed showed asymmetry of the two external jugular veins, the right external jugular vein was dilated and very torturous but appeared patent still. The diagnosis of venous varix was suggested.
Conclusion: Our case significantly highlights the role of radiological evaluation in the confirmatory diagnosis of this rare entity additionally emphasizing the consideration of venous varix in clinical practice whenever patients present with swelling that manifests on coughing or other strenuous actions to avoid misdiagnosis and prevent complications.
Introduction
Venous dilations of the jugular veins are uncommon and external jugular varix even rarer (1). Venous Varix is an abnormal dilation of the vein associated with tortuosity. Among neck veins, varix of the neck is an extremely uncommon clinical anomaly, and the true incidence is unknown. It is proposed that the varix could stem from a developmental anomaly in a tributary of the external jugular vein additionally, it is also speculated that the absence of elastic lamina in veins, possibly due to pathology, could contribute to vein dilation and distortion. Instances of this condition are infrequently documented in literature, with a case noted in Nigeria in 1985 (2).
Venous varices arise with arteriovenous malformations, developmental venous anomalies and rarely as singular lesions. Most commonly, they appear as focal dilatations of the venous drainage of arteriovenous malformations. Isolated varix displays comparable histological features to those accompanied by developmental venous anomalies (3). An anomalous varix situated at an eccentric site should prompt consideration of an intravascular tumor. In one case study, an intravascular hemangioendothelioma accompanied by thrombosis impeded retrograde blood flow during Valsalva's maneuver or exertion. Consequently, this obstruction gradually widened the external jugular vein, culminating in the development of a varix (4).
Venous varix of neck is a benign, self-limiting condition and complications like thrombosis, embolism, rupture, thrombophlebitis are rarely reported (5). The preliminary diagnosis of venous varix is usually incorrect or overlooked due to inadequate clinical evaluation (2). Therefore, either imaging studies or histopathological analysis are crucial for concluding at the definitive diagnosis. However, the documented instances of venous varix in literature are scarce, with even fewer references regarding its investigative approaches and treatment modalities. Consequently, we present a case involving a 29-year-old female who exhibited a soft, non-tender swelling on the right side of her neck, initially suspected to be a laryngocele upon clinical examination but subsequently confirmed as a venous varix through radiological assessment. We highlight this case to underscore the significance of radiological investigations in similar clinical presentations, aiming to enhance understanding and awareness in this regard.
Case presentation
A 29-year-old Saudi female presented to the department of ENT of Prince Mansour Military Hospital in Taif, complaining of right neck swelling for the past three years. The swelling increases in size when she coughed, shouted, or became angry. She denied any pain or tenderness over the site. There was no history of prior illness or injury at the site. She had no other contributary medical history. Her physical examination was unremarkable, except for a soft, compressible mass lateral to the sternocleidomastoid muscle, which became more prominent whilst performing the Valsalva maneuver. The skin over the swelling was blue and appeared darker than the surrounding tissue.
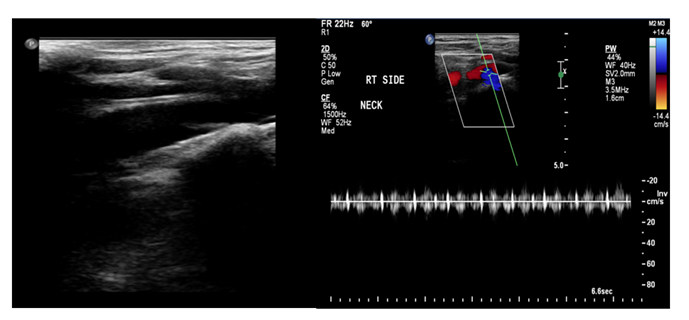
A plain radiograph of the neck was taken with the patient performing a Valsalva maneuver which failed to show neither an air-filled sac nor any soft tissue mass that defines the cause for the swelling on straining. An ultrasound scan of the neck at this stage showed a thin walled, compressible, cystic lesion in the right side of the neck, which was confirmed upon doppler study as dilation of the lower third of the right external jugular vein (Figure 1). A Computed Tomography (CT) scan of the neck and thorax showed asymmetry of the external jugular veins, the right external jugular vein was dilated and very torturous but appeared patent still (Figure 2). The initial diagnosis of laryngocele was precluded, and the diagnosis of venous varix was suggested.
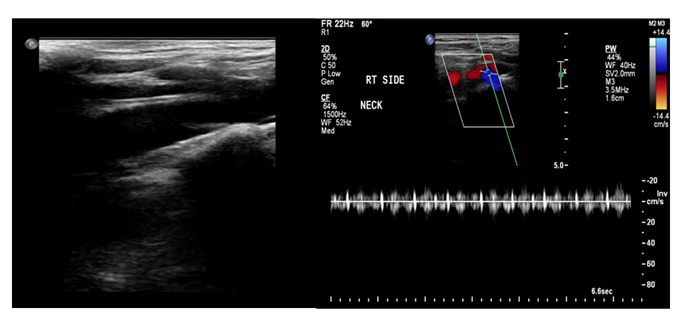
Figure 1: Doppler ultrasound showed a thin walled, compressible, cystic lesion in the right side of the neck, which was confirmed upon doppler study as dilation of the lower third of the right external jugular vein
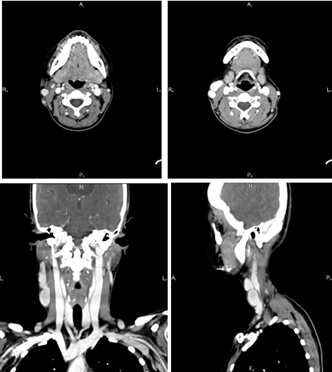
Figure 2: CT scan of neck and thorax exhibited asymmetry of the external jugular veins, the right external jugular vein was dilated and very torturous but appeared patent still
Discussion
The illustration of our case of external jugular venous varix highlights the role of radiological evaluation in the confirmatory diagnosis of this rare entity which can aid in establishing diagnostic criteria facilitating early diagnosis and prompt management since the jugular venous aneurysm is a rare presentation. Mostly the patients describe a painless swelling in their necks that manifests while coughing, straining, bending, or holding their breath (6). Jugular venous phlebectasia in adults is rare and only seen in isolated cases. Jugular vein varices, characterized by dilatation and tortuosity, are less common. A review of the literature found only two cases of external jugular varix discovered utilizing head and neck ultrasound imaging, as well as one case of external jugular venous aneurysm. The literature's inconsistent terminology and the rarity of external jugular venous anomalies hinder the understanding of their true natural history (1, 2, 4, 7).
Additionally, Mohanty et al. described that the presence of a soft and compressible swelling in the course of an external jugular vein superficial to the sternomastoid muscle, as well as non-filling when the external jugular vein is compressed during the Valsalva maneuver, confirms the diagnosis of an external jugular vein aneurysm. Color Doppler ultrasound enables for precise lesion delineation and is widely regarded as the gold standard for diagnosis confirmation (6). Similarly, our patient was presented with chronic swelling as it had lasted for three years and was more prominent when coughing or shouting. The examination revealed a soft, compressible mass lateral to the sternocleidomastoid muscle, which became more prominent whilst performing the Valsalva maneuver. Kindzelski et al. reported that cervical venous duplex scanning with the Valsalva maneuver is the preferred diagnostic method for suspected cervical venous malformation. Contrast-enhanced axial imaging, such as CT scan or magnetic resonance venography, should only be used in selected cases and for surgical planning. The rarity of the condition makes it challenging to develop intervention guidelines as the natural history is uncertain (1).
In the present time Iqbal K. reported a case of a 43-year-old woman who presented with one year of painless right supraclavicular swelling. She observed that the swelling increased with the Valsalva maneuver. Neck ultrasound with color Doppler revealed a vascular formation with turbulent blood flow, measuring 2.9 x 1.2 cm and appearing partially thrombosed. During additional evaluation, the patient had a CT scan of the neck with intravenous contrast, which revealed a right supraclavicular mass measuring 2.3 x 3.5 cm, most likely an external jugular vein saccular aneurysm. The author further highlights that clinical symptoms such as painless neck swelling that worsens with the Valsalva maneuver, coughing, or straining could indicate the diagnosis. Doppler ultrasonography is commonly used to confirm a diagnosis (8). We initially performed a plain X-ray which did not yield any significant or conclusive findings as radiograph did not show any air-filled sac nor any soft tissue mass that could define the cause for the swelling on straining. Hence the patient was additionally referred for an ultrasound scan of the neck which exhibited a thin walled, compressible, cystic lesion in the right side of the neck, which was confirmed upon doppler study as dilation of the lower third of the right external jugular vein. Similarly, Kumar et al. also agreed that the preferred method of diagnosis is ultrasonography with Doppler before, during, and after the Valsalva manoeuvre (9). Furthermore, in our patient the CT scan of the neck and thorax was performed which revealed asymmetry of the 2 external jugular veins, the right external jugular vein was dilated and very torturous but still appeared patent. The diagnosis for venous varix was then hence confirmed.
Differential diagnoses include laryngocele, cystic hygroma, branchial cyst, and superior mediastinal mass. These disorders have the greatest prevalence in children and might be difficult to diagnose. Furthermore, the incidence of this disease is minimal, with just about 100 cases of phlebectasia described in the English literature to date in various neck veins, with the internal jugular being the most common to be afflicted, followed by the external jugular and anterior jugular veins. However, there is insufficient data in the literature on size regression without intervention. Radiological examinations are required to establish the diagnosis and keep records so that serial monitoring can be done and documented. Chest X-rays can rule out the diagnosis of laryngocele or mediastinal tumor since the images will show no air or a large mediastinum. The diagnosis is confirmed using an ultrasound combination with Doppler flow imaging or a spiral CT scan with contrast [10]. Initially, in our patient, we also predicted the diagnosis of laryngocele. However, it was ruled out after the chest radiograph findings, which did not exhibit any air-filled sac or tissue mass.
Nana et al. suggests that external jugular vein anomalies should be considered as a differential diagnosis for neck masses. High clinical suspicion along with reliable imaging are required for diagnosis (10). Venous ultrasonography is becoming the first diagnostic procedure of choice, replacing more invasive treatments (11). Ultrasound has high sensitivity and specificity, making it a preferred diagnostic modality. CT/ magnetic resonance venography may be necessary for surgery to determine the extent and relationship to adjacent structures, as well as to differentiate from other regional pathology that may not be detected by ultrasonography (12). The presentation of our case along with evidence from literature profoundly emphasizes the critical role of radiological evaluation in the diagnosis of this rare condition. Radiological evaluation is indispensable in the diagnosis and management of external jugular venous varix, providing essential information for accurate diagnosis, treatment planning, and monitoring of the condition.
Conclusion
External jugular venous varix is a rare condition with very limited cases published till date which makes the presentation of our case unique. Moreover, our case significantly highlights the role of radiological evaluation in the confirmatory diagnosis of this rare entity additionally emphasizing the consideration of venous varix in clinical practice whenever patients present with swelling that manifests on coughing or other strenuous actions to avoid misdiagnosis and prevent complications.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.