Volume 4, Issue 8
August 2024
Systemic and Oral Health Relationship Among Adults Attending Makkah Armed Force Medical Centre Dental Clinic
Tahani M. Binaljadm, Somayah A. Halabi, Ghassan M. Rummani, Hani B. Alsaadi, Anan A. Alandanousi, Yousef S. Alalyani, Abdulaziz S. Alzahrani, Nisreen N. Hassan
DOI: http://dx.doi.org/10.52533/JOHS.2024.40803
Keywords: oral health, oral index, systemic health, systemic index, panoramic radiograph
Background: Oral health affects systemic health and vice versa. Several systemic disorders such as such as osteoporosis, acquired immunodeficiency syndrome (AIDS), and hypertension may impact oral tissue either directly or indirectly. Oral health conditions can have an impact on systemic health by reducing patients’ nutritional intake and quality of life. Our aim in this study is to investigate the presence of a correlation between patients’ oral health and systemic health via panoramic radiography.
Methods: In this original study, the included population comprised patients older than 18 years who received dental treatment at Makkah Armed Forces Medical Center between March 1 and August 30, 2023. We collected oral scores based on patients’ panoramic radiograph, and we assessed medical conditions based on patients’ medical records. We collected data using an Excel spreadsheet and statistically analyzed them using IBM’s SPSS Statistics software.
Results: Over a period of 6 months, we collected data from 491 participants. Their mean age was 40.4 years (±14.4 SD). Most of the patients we examined (67.8%) were normal healthy individuals (medical index: 0). We found no statistically significant difference between gender and nationality with respect to the medical index (MI) or oral index (OI). In contrast, age significantly affected both indexes. We found a positive correlation between the OI and MI.
Conclusions: Our study proved that there is a link between oral and systemic health. With increasing age, both systemic and oral health deteriorated. However, future clinical studies with a large sample size are necessary.
Introduction
A variety of irritants can harm the oral cavity in different ways. Because the mouth is the primary opening to the body, a steady stream of bacteria, viruses, and fungi infiltrate it. In addition, the mouth is home to a variety of unique substrata and microenvironments that support a highly dynamic microbial ecosystem. Other nearly constant environmental challenges that the oral cavity faces include the host’s food, salivary flow, masticatory pressures, and the entry of exogenous microorganisms. Throughout life, the host’s genetic makeup and maternal transmission influence the composition of the oral microbiome. Environmental factors that also have an impact include diet choices, dental hygiene practices, medications, and systemic factors (1).
Oral health influences systemic health and vice versa. Many systemic diseases such as osteoporosis, acquired immunodeficiency syndrome (AIDS), and hypertension may affect oral tissue directly or indirectly. Epidemiologic and large population research, clinical studies, and in vitro animal studies highlight the crucial importance of oral health to overall health. Conditions that occur in the oral cavity might affect systemic health through impairing patients’ nutrition and their quality of life. Oral microorganisms reach distant tissue in the body via blood vessels or the gastrointestinal tract. In a recent study, researchers identified the presence of oral bacteria, primarily P. gingivalis, in diseased organs and a link between impaired oral microbiota and an elevated risk of pancreatic and liver illnesses (2).
Evidence also shows that there is a bidirectional association between oral health and some systemic diseases. Many variables have been proposed to mediate this correlation between oral and systemic health, including microbial dysbiosis and bacteremias, medications, environmental factors (stress), habits (smoking, high-fat diets, consumption of highly processed foods), predisposing and precipitating factors (gene polymorphisms), and altered host immune responses. These correlations are present in the context of systemic inflammation, persistent bacteremias, and/or immune system abnormalities (3).
An example is the correlation between diabetes and periodontal disease. Patients diagnosed with diabetes experience periodontitis more often than patients without diabetes do (4). Many interventional studies (5, 6) have established the correlation between the effect of dental treatment on medical disorders, such as periodontal therapy on glycemic management or cardiovascular illnesses. Engebretson et al. investigated the cause behind the bidirectional correlation between diabetes and periodontal disease and found that both share the inflammatory process (7). The World Health Organization identifies oral health as a “key indicator of overall health, well-being, and quality of life” and notes that oral health shares “modifiable risk factors with the leading noncommunicable diseases (cardiovascular diseases, cancer, chronic respiratory diseases, and diabetes)” (8).
The aim of this study is to investigate whether there is a correlation between patients’ systemic health and oral health via panoramic radiography in Saudi Arabia.
Methods
This is an original study, which includes a population comprised male and female patients older than 18 years, who received dental treatment with good panoramic radiograph quality at Makkah Armed Forces Medical Center between March 1 and August 30, 2023. We excluded patients under 18 years old or with poor panoramic radiograph quality. We removed all repeated file numbers and collected data using an Excel spreadsheet.
Two independent examiners—an experienced senior registrar in restorative dentistry and a senior registrar in conservative dentistry—took panoramic radiography oral health data from patients’ records. Data collected from the panoramic radiograph were caries, periapical health, bone loss, and tooth loss. Total scores ranged from 0 to 8. We based systemic health scores on medical conditions reported in patients’ records. The medical scores ranged from 0 to 6 based on patients’ systemic conditions and functional limitations. The data findings are displayed in (Table 1). We obtained our criteria to calculate the oral and medical indexes, using a modified version of the oral health scale, in addition to the types of statistical tests in the current study, from Joseph et al.’s 2016 study (9).
|
Table 1: Criteria of Medical index and Oral index |
|||||
|
Medical index (0 to 6) |
Dental index (0 to 8) |
||||
|
Score |
Medical condition |
Caries |
Bone loss |
Periapical Health |
tooth loss |
|
0 |
Normal and healthy |
No lesion |
Healthy – no bone loss |
No lesion |
All teeth present except 3rd molar |
|
1 |
Mild systemic disease |
1-3 lesion |
Moderate – Less than 50% bone loss |
Less than 3 lesions |
Less than 10 missing teeth |
|
2 |
Moderate Systemic Disease |
More than 3 lesions |
Sever – Less than 50% bone loss |
3 or more lesions. |
10 or more missing teeth. |
|
3 |
Severe systemic disease that limits activity but is not incapacitating. |
||||
|
4 |
Severe systemic disease that limits activity and is a constant threat to life. |
||||
|
5 |
Severe systemic disease that limits activity and is a constant threat to life |
||||
|
6 |
Terminally-ill patients. |
||||
Statistical Analysis
Using IBM’s SPSS Statistics version 26 software, we arranged, tabulated, and statistically analyzed the data. We calculated the range, mean, and standard deviation for quantitative data. We created an independent-samples t-test for comparisons between more than two means of parametric data. Qualitative data define a categorical set of data by frequency, percentage, or proportion of each category. We used Spearman’s rank correlation coefficient (r) to assess the correlation between the variables. To interpret the findings of tests of significance, we defined significance as ρ < 0.05 and extreme significance as ρ < 0.001.
Before conducting our study, we obtained ethical approval from the Medical Services General Directorate Research & Ethics Committee Western Region, reference number REC.2023-676, February 1, 2023.
Results
Our study included 124 male (31%) and 367 (68%) female patients seen between March 1 and August 30, 2023. Their mean age was 40.4 years (±14.4 SD), ranged between 18 and 91 years old. Around 98% of the patients were Saudi citizens; the remaining 2% were non-Saudi. The mean oral index (OI) was 3.16 (± 1.53 SD), and the mean medical index (MI) was 0.53 (± 1.006 SD). Most of the patients we examined—265 (67.8%) out of 391—were normal healthy individuals (MI: 0). Twenty-two percent of the patients had mild systemic disease and a medical score of 1. Only one patient, 54 years old, attended the clinic with severe systemic disease that limited her activity. Generally, we found no statistically significant difference between gender and nationality with respect to the MI, whereas we did find a statistically significant difference in oral conditions with all levels of the MI (Table 2). Patients with an MI ≥ 2 (having at least two systemic diseases) showed a statistically significant difference compared to patients with an OI ≤ 2 (3%) and ≥ 3 (35%) (Table 3).
|
Table 2: Medical index |
|||||||
|
Medical index |
No. (%) |
Gender |
Nationality |
Oral index |
|||
|
Male No. (%) |
Female No. (%) |
Saudi No. (%) |
Non-Saudi No. (%) |
OI ≤ 2 No. (%) |
OI ≥ 3 No. (%) |
||
|
0 |
265 (67.8) |
79 (63.7) |
186 (69.6) |
261 (67.6) |
4 (80) |
105 (79.5) |
160 (61.7) |
|
1 |
88 (22.5) |
35 (28.2) |
53 (19.8) |
87 (22.5) |
1 (20) |
24 (18.1) |
64 (24.7) |
|
2 |
13 (3.3) |
5 (4.03) |
8 (2.9) |
13 (3.3) |
0 (0.0) |
1 (0.7) |
12 (4.6) |
|
3 |
6 (1.5) |
2 (1.61) |
4 (1.4) |
6 (1.5) |
0 (0.0) |
0 (0.0) |
6 (2.3) |
|
4 |
18 (4.6) |
3 (2.41) |
15 (5.6) |
18 (4.6) |
0 (0.0) |
2 (1.5) |
16 (6.1) |
|
≥5 |
1 (0.3) |
0 (0.0) |
1 (0.3) |
1 (0.2) |
0 (0.0) |
0 (0.0) |
1 (0.3) |
|
Total |
391 (100.0) |
124 (31.7) |
267 (68.3) |
386 (98.7) |
5 (1.3) |
132 (33.7) |
259 (66.3) |
|
Mean ± SD |
0.5345 ± 1.006 |
0.508 ± 0.850 |
0.546 ± 1.072 |
0.538 ± 1.011 |
0.200 ± 0.447 |
0.257 ± 0.625 |
0.675 ± 1.128 |
|
P value |
0.0001** |
0.724 |
0.455 |
0.0001** |
|||
** Highly statistically Differences at (P < 0.01)
|
Table 3: Description of the Medical Index |
|
|
Score |
Description |
|
1 |
Mild systemic disease. Patient with 1 or 2 of the following well controlled disease states including non-insulin dependent diabetes, hypertension, epilepsy, asthma or thyroid condition otherwise healthy individual with respiratory condition, pregnancy and/or active allergies. |
|
2 |
Moderate systemic disease. Patients with more than two of the above mentioned diseases. |
|
3 |
Severe systemic disease that limits activity but is not incapacitating. History of angina pectoris, myocardial infraction or cerebrovascular accident, cognitive heart failure over the 6 months ago, slight COPD and controlled insulin dependent diabetes or hypertension. |
|
4 |
Severe systemic disease that limits activity and is a constant threat to life. Patient with one or two of the following diseases states including history of unstable angina pectoris, myocardial infraction or cerebrovascular accident within the last 6 months, moderate to severe COPD and uncontrolled diabetes, hypertension, epilepsy, thyroid condition. |
|
5 |
Severe system disease that limits activity and its constant threat to life. Patient with more than two of the above-mentioned disease states. |
|
6 |
Terminally- ill patients. |
Regarding the OI, most participants scored ≥ 4 (40.7%), followed by those scoring 3 (25.6%). Only 14.8 % of the participants had an OI ≤ 1. There is a direct proportional relationship between the number of patients with medical conditions and the OI. The number of patients increases with an increasing OI score. Male Saudis with medical conditions showed the highest percentage with an OI score ≥ 4. Gender and nationality showed no statistically significant difference with respect to the OI. However, medical conditions significantly affect the OI (Table 4).
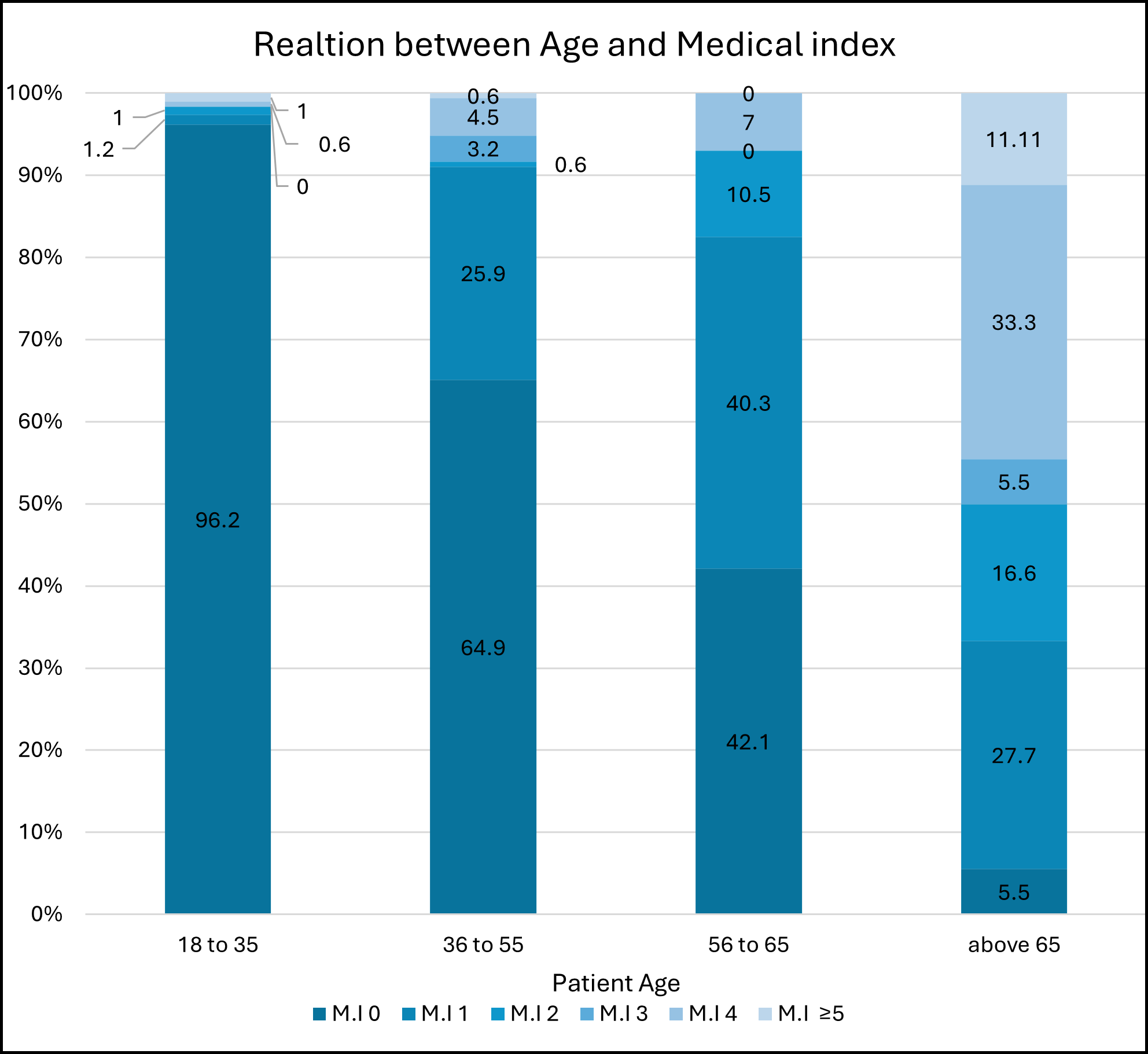
Regarding the MI in relation to patients’ age, there is generally a direct proportional correlation between age and medical score. With increasing age, the percentage of patients with a higher medical score increases. The percentage of patients who were healthy with a medical score of 0 was very high in the age group 13 to 35 years (96%), and those with a medical score of 5 and above were from the age group older than 65 years (11.1%) (Figure 1).
(Figure 2) shows the correlation between patients’ age and OI. With increasing age, the percentage of patients with an OI of 2 and above increases. The percentage of subjects from the age group 13 to 35 years with a medical score ≥ 4 was 21.6%. It then increases to 42.2%, 64.9, and finally 88.2% in the age group 65 years and older. All patients from this age group recorded an OI of 3 and above.
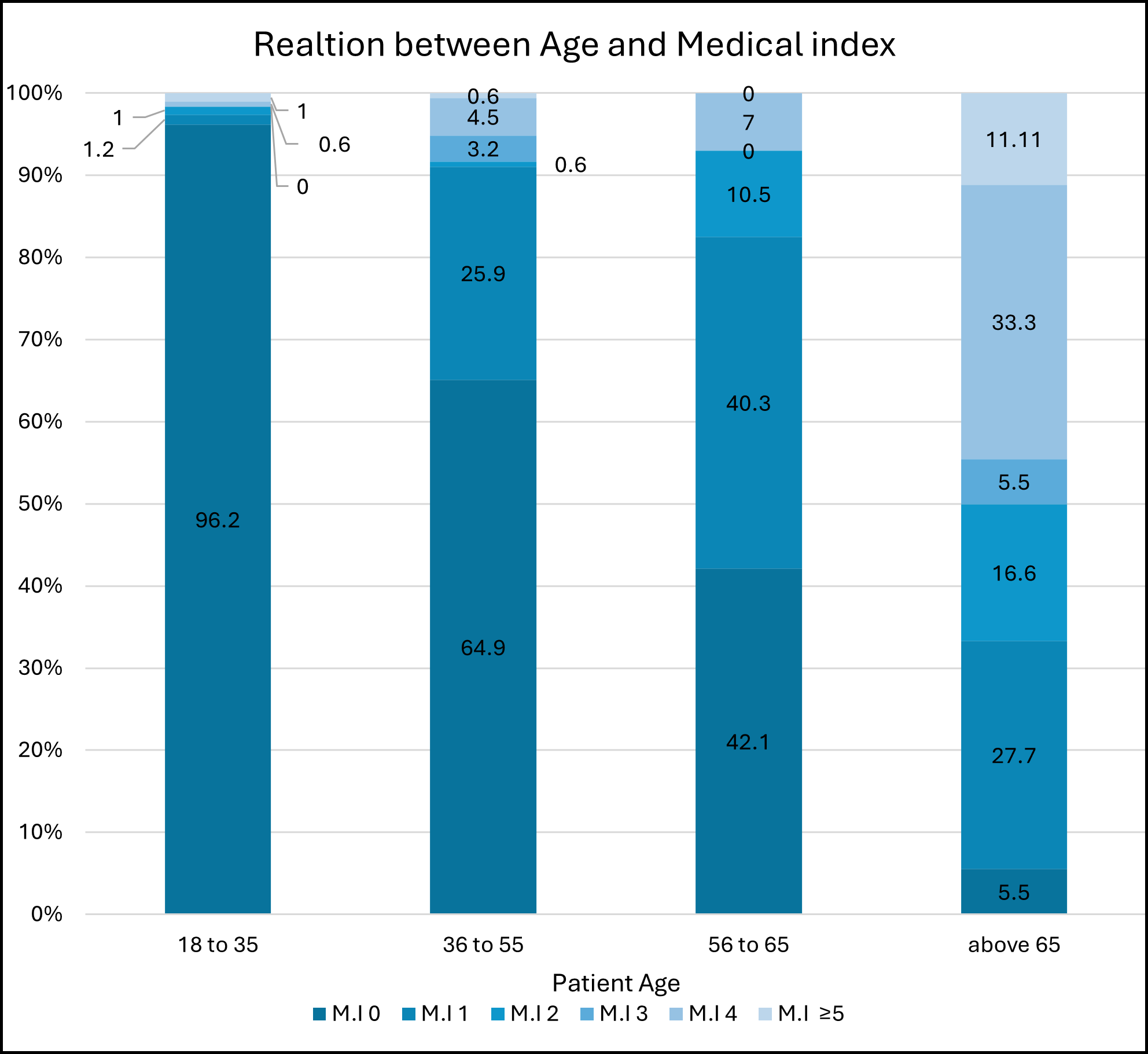
Figure 1: Showing relation between different patient age group and medical score index
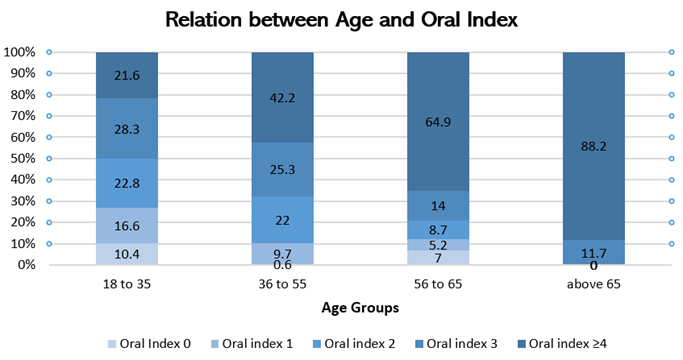
Figure 2: Relation between age and Oral index
|
Table 4: Oral index |
||||||||
|
Oral index |
No. (%) |
Gender |
Nationality |
Medical Condition |
||||
|
Male No. (%) |
Female No. (%) |
Saudi No. (%) |
Non-Saudi No. (%) |
With No. (%) |
Without No. (%) |
|||
|
0 |
11 (2.8) |
3 (2.4) |
8 (2.9) |
11 (2.8) |
0 (0.0) |
2 (1.5) |
9 (3.3) |
|
|
1 |
47 (12.0) |
15 (12.0) |
32 (11.9) |
46 (11.9) |
1 (20) |
11 (8.7) |
36 (13.5) |
|
|
2 |
74 (18.9) |
20 (16.1) |
54 (20.2) |
72 (18.6) |
2 (40) |
14 (11.1) |
60 (22.6) |
|
|
3 |
100 (25.6) |
30 (24.1) |
70 (26.2) |
99 (25.6) |
1 (20) |
26 (20.6) |
74 (27.9) |
|
|
≥4 |
159 (40.7) |
56 (45.1) |
103 (38.5) |
158 (40.9) |
1 (20 |
73 (57.9) |
86 (32.4) |
|
|
Total |
391 (100.0) |
124 (31.7) |
267 (68.3) |
386 (98.7) |
5 (1.3) |
126 (32.2) |
265 (67.8) |
|
|
Mean ± SD |
3.163 ± 1.530 |
3.387 ± 1.714 |
3.059 ± 1.428 |
3.171 ± 1.531 |
2.600 ± 1.516 |
3.642 ± 1.499 |
2.935 ± 1.494 |
|
|
P value |
0.0001** |
0.049* |
0.408 |
0.0001** |
||||
* Statistically Significant Differences at (P < 0.05)
** Highly statistically Significant Differences at (P < 0.01)
Upon examining the correlation between the oral and medical indexes in (Table 5), we found that there was a positive correlation (ρ) between the two, indicating that there was a significant association between age and both oral and medical indexes.
Regarding the medical conditions in patients with an OI ≥ 4, we found that 33% had more than one disease, 28% had diabetes, 21% had hypothyroidism, 16% had hypertension, and 2% suffered from arthritis, anemia, and cholecystitis. We found diabetes and hypertension in 82.7% of those cases who had more than one condition. Regarding tooth loss, about 80% of the cases who scored 2 (10 or more missing teeth) were patients who had both diabetes and hypertension.
|
Table 5: Correlation between oral index and medical index |
||||
|
Variable |
Oral index |
Medical index |
||
|
Correlation |
P value |
Correlation |
P value |
|
|
Medical index |
0.258 |
0.0001** |
||
|
Controlling factors Gender Nationality Age |
-0.077 -0.047 0.416 |
0.128 0.356 0.0001** |
-0.043 -0.034 0.449 |
0.402 0.503 0.0001** |
** Highly statistically Significant Differences at (P < 0.01)
Discussion
Our main aim in this study was to investigate the correlation between systemic health and oral health in a single center in Saudi Arabia, that provided treatment to Saudis and non-Saudis. We based our assessment method on Joseph et al.’s study (9). They investigated the correlation between oral health and systemic health based on patients’ medical history and dental radiograph.
The results of this study showed a correlation between OI score and medical condition. Patients with poor medical condition had at least 2 systemic diseases and showed poor oral health condition (≥ 3). The number of patients with medical conditions increases as the OI score increases. Our results are similar to those that Alnafisah et al. found in Qassim, Saudi Arabia, where they correlated the medical history of patients’ dental health using the following parameters: decayed, missing, or filled teeth and modified decayed, missing, or filled teeth indices; the Silness and Loe Plaque Index, and the bleeding index (10).
In our study, gender did not significantly affect the medical and oral health score, which is similar to a study conducted in Kuwait (9). In addition, nationality did not significantly influence the medical or dental score. We could attribute this to the small number (only 5) of non-Saudi participants.
Regarding the age factor, we found that age affected both the medical and dental score. This is similar to a study conducted in 2009, where the authors found individuals, who tended to be older adults with chronic conditions such as diabetes and rheumatoid arthritis, are at higher risk of having oral conditions (11). Other studies have also proved the effect of the age factor on systemic health. Thorstensson and Johansson investigated the correlation between oral health indicators regarding patient demographic data on subsequent survival in the Swedish population. They found the prevalence of systemic diseases increases as age increases (12). In older patients, biofilm accumulation, decreased salivary flow, multiple medication (13), poor oral hygiene, and decreased dental care may coexist with major or minor physical disabilities. Mental problems can lead to poor oral condition. In addition, older patients may view dental treatment as less important, which exacerbates their oral health.
Confounding factors in our investigation were patients’ age, gender, and nationality. The main limitations were small sample size, low number of non-Saudi patients and a single investigation center.
Research suggests that both hypertension and diabetes can individually contribute to oral health problems, including periodontal disease and tooth loss. Several physiological processes can account for this. Both diabetes and hypertension, and tooth loss showed a bidirectional relationship. The following are mechanisms discussed in the literature that prove this relationship. Endothelial dysfunction can arise from increased systemic inflammation after the onset of hypertension that can cause periodontitis (14). Conversely, periodontal pathogens have the ability to intensify the inflammatory cascade through the activation of Th1 and Th17 lymphocytes, which in turn triggers an inflammatory mechanism that leads to hypertension (15). Diabetes causes periodontal disease, which in turn causes tooth loss. Several physiological processes, including cytokines, microbiota, immunological responses, and glycosylation products, can explain this (16). In contrast, diabetic patients create more glycosylation products, which cause collagen cross-linking. This decreases the soluble amount of collagen and reduces the possibility of collagen regeneration and repair. These processes all result in gingivitis, which spreads to the periodontal tissue and increases the risk of tooth loss by damaging the bone, cement, and ligaments (15). A recent systematic review and meta-analysis proved the correlation between diabetes and tooth loss (17). Regarding hypertension and tooth loss, Tada et al. conducted a meta-analysis in 2022 and showed a correlation between hypertension and tooth loss (18). In our study we noticed 80% of the cases who had 10 or more missing teeth were diagnosed with hypertension and diabetes. However, no specific recent studies directly link the synergistic effect of both hypertension and diabetes to tooth loss. The confounding factors in our investigation were patients’ age, gender, nationality and the main limitations were small sample size, low number of non-Saudi patients and a single investigation center. Therefore, future researchers should conduct studies with larger sample sizes and control for other risk factors to investigate the synergistic effect of hypertension and diabetes on tooth loss.
Conclusion
Our main aim in this study was to investigate the correlation between oral health and overall health. With increasing age, patients’ systemic and oral health deteriorated. Future studies with a larger sample size in multiple centers across Saudi Arabia and a correlation between disease type and patients’ oral condition will significantly aid in improving knowledge of the correlation between patient oral and systemic health in the country. In addition, studying the synergistic effect of hypertension and diabetes would help to identify the combined impact of these conditions on oral health outcomes compared to either condition alone. It would contribute to a better understanding of how health-care professionals can more effectively address the oral health needs of patients with both hypertension and diabetes.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
All authors have declared that no financial support was received from any organization for the submitted work.
Ethical consideration
Ethical approval for this research was received from the Medical Services General Directorate Research & Ethics Committee Western Region, where the research was conducted, with approval number REC.2023-676, February 1, 2023
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, and final writing of the manuscript.