Volume 4, Issue 5
May 2024
Palliative Care Needs and Symptom Burden in Patients Undergoing Maintenance Hemodialysis: A Systematic Review
Sara Haneef, Marwah Abdullah
DOI: http://dx.doi.org/10.52533/JOHS.2024.40502
Keywords: hemodialysis, palliative, care, needs, symptom, burden
While life-sustaining, hemodialysis imposes significant physical, emotional, and psychological burdens on patients. The integration of palliative care into the routine management of hemodialysis patients has shown promising benefits. Studies indicate that early palliative care intervention can significantly improve symptom control, enhance quality of life, and reduce hospital admissions and healthcare costs. By addressing the multifaceted needs of hemodialysis patients through palliative care, it is possible to enhance their quality of life significantly. This systematic review aims to synthesize the existing evidence on palliative care needs and symptom burden in hemodialysis patients, highlighting the critical role of palliative care in this vulnerable population. The inclusion criteria encompass studies focusing on adults undergoing maintenance hemodialysis. A quality assessment was performed using the Newcastle-Ottawa Scale to ensure the reliability and validity of findings. Findings highlight significant palliative care needs among hemodialysis patients and emphasize positive perceptions of palliative care interventions among patients underscoring their value while comfort-focused treatment, was prioritized defining the necessity for improved decision-making and access to palliative care services in dialysis settings. Additionally, research identified varied levels of palliative care needs among patients, with a notable proportion experiencing moderate to severe requirements. Furthermore, results of this study indicate the burden of symptoms among hemodialysis patients is extensive and diverse, encompassing issues like fatigue, pain, and itching, which are particularly pronounced among older individuals. These symptoms significantly impair patients' quality of life. Moreover, symptom severity varies widely among patients, with certain symptoms such as sleep disturbances and itching posing significant challenges to patient comfort and well-being. These findings underscore the complex symptom management needs within the hemodialysis population. Future research should focus on standardizing measures of palliative care needs, evaluating the effectiveness of tailored interventions, and addressing gaps in current evidence to improve palliative care delivery and patient outcomes in hemodialysis settings.
Introduction
End-stage renal disease (ESRD) is a rapidly increasing global health and healthcare burden, necessitating renal replacement therapies such as hemodialysis for survival. The global prevalence of ESRD is rising, with the all-age prevalence of chronic kidney disease (CKD) reported to have increased by a striking 29.3% between 1990 and 2017 (1). This growing prevalence of ESRD has resulted in an increasing number of maintenances for hemodialysis patients, particularly among older individuals with conditions such as diabetic nephropathy and micro vascular disease (2). While life-sustaining, hemodialysis imposes significant physical, emotional, and psychological burdens on patients. The complexity of care required for these patients, coupled with the high symptom burden and reduced quality of life, underscores the need for comprehensive palliative care.
Patients undergoing maintenance hemodialysis experience a broad spectrum of symptoms. Pain, both acute and chronic, is a common and often under-treated issue. Fatigue, reported by over 60-97% of hemodialysis patients, is one of the most debilitating symptoms, impacting daily activities and overall well-being (3, 4). Pruritus, or severe itching, affects approximately 42% of these patients, leading to significant discomfort and sleep disturbances (5). Additionally, sleep disorders, including insomnia and restless legs syndrome, are prevalent, further exacerbating the overall symptom burden. These symptoms not only affect physical health but also contribute to psychological distress, including anxiety and depression (6). The psychological impact of maintenance hemodialysis cannot be overstated. The chronic nature of the disease, coupled with the demanding dialysis schedule, imposes a significant psychological toll. Depression and anxiety are prevalent among hemodialysis patients, with studies reporting rates as high as 85.98% and 84.11%, respectively (7). The prolonged hemodialysis treatment and the burden of illness can lead to significant emotional distress in patients (8).
Palliative care is an approach to improve the health-related quality of life (QoL) of patients and their families in the face of problems associated with life-threatening illnesses, through preventing and alleviating suffering by means of early identification and accurate assessment and treatment of pain and other physical, psychosocial, and spiritual problems (9). In 2015, Kidney Disease: Improving Global Outcomes (KDIGO) emphasized the critical necessity of incorporating palliative care services to enhance the quality of care for patients with ESRD. KDIGO recommended that palliative care should be accessible throughout the entire ESRD treatment journey, regardless of whether patients are undergoing dialysis or not (10). The integration of palliative care into the routine management of hemodialysis patients has shown promising benefits. Studies indicate that early palliative care intervention can significantly improve symptom control, enhance quality of life, and reduce hospital admissions and healthcare costs (11). Palliative care teams, comprising multidisciplinary professionals, offer a holistic approach to patient care, addressing complex symptomatology and providing tailored support to meet individual needs. Furthermore, palliative care fosters better communication between patients, families, and healthcare providers, facilitating shared decision-making and aligning treatment goals with patient preferences.
Despite the recognized benefits, several challenges hinder the widespread implementation of palliative care in hemodialysis settings. Limited awareness and understanding of palliative care among patients and healthcare providers, cultural and societal attitudes towards palliative care, and the perceived association of palliative care with terminal illness are significant barriers (12). Research has shown that both cancer and non-cancer patients, including those with ESRD, heart failure, and chronic obstructive pulmonary disease, have significant palliative care needs, particularly in symptom management (13). A systematic review focusing on the palliative care needs of patients with malignant and non-malignant diseases similarly highlighted a broad spectrum of needs. These needs include physical, emotional, informational, relational, practical support, financial, and spiritual aspects (14). One of the critical outcomes of palliative care interventions is the improvement in quality of life for patients undergoing maintenance hemodialysis. Quality of life encompasses various dimensions, including physical well-being, psychological state, social interactions, and overall life satisfaction. By addressing the multifaceted needs of hemodialysis patients through palliative care, it is possible to enhance their quality of life significantly.
This systematic review aims to synthesize the existing evidence on palliative care needs and symptom burden in hemodialysis patients, highlighting the critical role of palliative care in this vulnerable population.
Material and methods
Definition of outcomes and inclusion criteria
The outcomes of this systematic review focused on palliative care needs, symptom burden, QoL, and symptom severity in patients undergoing maintenance hemodialysis. Palliative care needs were assessed through patient and nephrologist satisfaction with interventions, care preferences for comfort and symptom management, and the extent of palliative care service usage. Symptom burden included physical symptoms such as pain, fatigue, pruritus, sleep disturbances, and psychological symptoms like anxiety and depression. Quality of life was measured using validated instruments like the KDQoL, SF-36, and EQ-5D, examining physical, psychological, social, and overall well-being. Symptom severity was evaluated by the intensity of specific symptoms, including pain, mobility issues, gastrointestinal problems, and psychological distress. Inclusion criteria for the review encompassed studies involving adults (≥18 years) with ESRD on maintenance hemodialysis, reporting on at least one of the defined outcomes. The review included observational studies, and other relevant study designs that reported on at least one of the defined outcomes related to symptom burden, or QoL.
To maintain precision and reliability, the exclusion criteria involve the exclusion of animal studies, in vitro investigations, laboratory studies, and research with redundant findings. Additionally, abstract-only presentations, reviews, books, posters, theses, editorials, notes, letters, case reports, case series, and conference papers are excluded. Studies were selected based on the inclusion and exclusion criteria by two independent authors. Any disagreement was settled by consensus among all authors.
Search Strategy
We conducted a comprehensive search across electronic databases, including PubMed, and ScienceDirect for publication. The search strategy employed for this study encompasses a comprehensive approach to identify relevant literature. It involves combining various terms: (“Maintenance Hemodialysis” OR “ESRD” OR “End-stage renal disease” OR “Hemodialysis” OR “Hemodialyses” OR “Hemodialysis patients” OR “Renal Dialyses” AND “Needs assessment” OR “Palliative care” OR “Symptom burden” OR “Symptom Management” OR “Supportive care” AND “Quality of life” OR “Symptom relief” OR “Symptom management” OR “Symptom improvement” OR “Care improvement” OR “Palliative care optimisation”)
Screening and extraction
Articles with irrelevant titles were excluded from consideration. In the subsequent phase, both the full text and abstracts of papers were meticulously reviewed to determine their compliance with the inclusion criteria. To streamline the process, titles and abstracts were organized, assessed, and scrutinized for any duplicate entries using reference management software (Endnote X8). To ensure the highest quality of selection, a dual screening approach was adopted, involving one screening for the evaluation of titles and abstracts, and another for the comprehensive examination of the entire texts. Once all relevant articles were identified, a structured extraction sheet was created to capture pertinent information aligned with our specific objectives.
Two separate researchers conducted the data extraction process independently. The gathered information included various study attributes like the author's name, publication year, country of origin, study design, sample size, duration of follow-up, and sources of funding. Additionally, details regarding participants such as age, gender, and nationality, were also collected.
Quality Assessment
In our systematic review, we employed the Newcastle-Ottawa Scale (NOS) as a critical tool for assessing the quality of non-randomized studies included in our analysis. The NOS is widely recognized for its utility in evaluating the methodological quality and risk of bias in observational studies, including cohort and case-control studies. It provides a structured framework for evaluating key aspects of study design, including selection of study groups, comparability, and ascertainment of outcomes. By using the NOS, we were able to systematically appraise the included studies and ensure that only high-quality evidence contributed to our analysis, thereby enhancing the robustness and reliability of our findings.
Results
Search Results
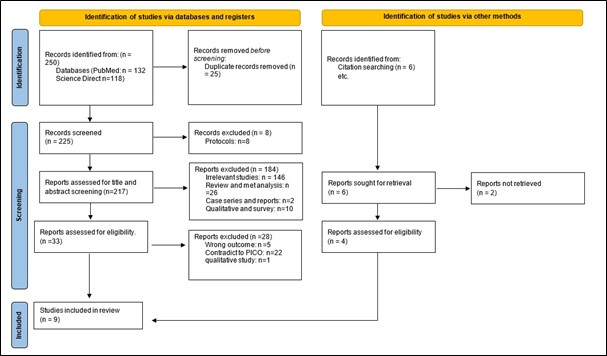
We executed the search methodologies outlined previously, resulting in the identification of a total of 250 citations, subsequently reduced to 225 following the removal of duplicates. Upon screening titles and abstracts, only 39 citations met the eligibility criteria for further consideration. Through full-text screening, this number was further refined to 9 articles aligning with our inclusion and exclusion criteria (15-23). Figure 1 provides an in-depth depiction of the search strategy and screening process.
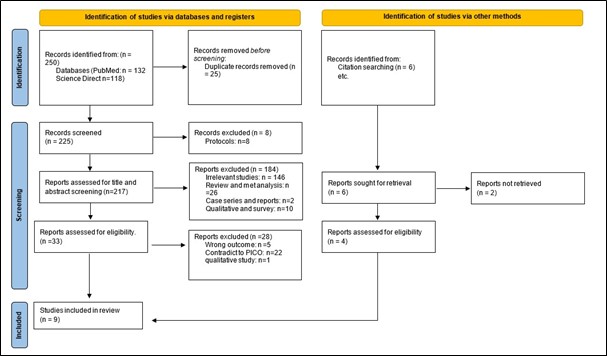
Figure 1: PRISMA flow chart
Results of Quality Assessment
The NOS assessment of the included studies in our systematic review and meta-analysis reveals a range of methodological qualities across the selected literature. The studies reviewed demonstrated varying quality in assessing palliative care needs and symptom burden in hemodialysis patients. Three studies (Lowney et al.; Chen et al.; Gunarathne et al.; Wang et al.,) achieved a "Good" quality score of 7-8 (16, 17, 19, 22). The remaining studies were rated as "Satisfactory" with scores ranging from 6-7 (Table 1).
|
Table 1. Quality assessment of Newcastle–Ottawa scale (NOS) for included studies. |
|||||
|
Study |
Selection |
Comparability |
Outcome |
Total Score |
Quality |
|
Weisbord et al., (2003) (15) |
3 |
0 |
3 |
6 |
Satisfactory |
|
Lowney et al., (2015) (16) |
3 |
2 |
2 |
7 |
Good |
|
Chen et al., (17) |
3 |
2 |
3 |
8 |
Good |
|
Saeed F, et al., (2020) (18) |
4 |
0 |
2 |
6 |
Satisfactory |
|
Gunarathne et al., (2022) (19) |
4 |
2 |
2 |
8 |
Good |
|
Liem et al., (2022) (20) |
4 |
0 |
2 |
6 |
Satisfactory |
|
Wang et al., (2022) (21) |
4 |
0 |
2 |
6 |
Satisfactory |
|
Wang et al., (2023) (22) |
4 |
2 |
2 |
8 |
Good |
|
Zhou MG et al., (2023) (23) |
4 |
0 |
2 |
6 |
Satisfactory |
Characteristics of the included studies
The baseline characteristics of the included studies on palliative care needs and symptom burden among hemodialysis patients exhibited a wide range of study designs, participant demographics, and dialysis durations across various countries. The total participant numbers varied significantly, from small pilot surveys like those by Weisbord et al. in Pakistan with 19 participants to larger cross-sectional studies like Lowney et al. in Ireland and England with 893 participants (15, 16). The mean age of participants ranged from 49.61 years in Saeed et al. to 72 years in Chen et al., with a consistent male predominance in all studies (17, 18). Dialysis vintage, where reported, also varied, highlighting differences in patient experiences and healthcare settings (Table 2).
|
Table 2. Baseline characteristics of included studies |
||||||||
|
Author |
Country |
Year |
Study Design |
Study Period |
Total Participants |
Mean Age of total participants |
Gender(M/F) |
Dialysis vintage/ duration |
|
Weisbord et al., (15) |
Pakistan |
2003 |
Pilot |
NR |
19 |
67±9.6 |
63.16%/36.84% |
NR |
|
Lowney et al., (16) |
Ireland and England |
2015 |
Prospective cross-sectional |
2011-2012 |
893 |
64.5 ±16.4 |
61%/39% |
4 years |
|
Chen et al., (17) |
US |
2018 |
Observational cohort |
2001-2015 |
536 |
72±13 |
60%/40% |
median 23 months |
|
Saeed et al., (18) |
Pakistan |
2020 |
Pilot survey |
2015 |
522 |
49.61 ±13.94 |
56.5%/43.5% |
NR |
|
Gunarathne et al., (19) |
Sri Lanka |
2022 |
Cross-sectional |
2019 |
118 |
40–55 Years and >55 years |
63.6%/36.4% |
NR |
|
Liem et al., (20) |
Den mark |
2022 |
Cross-sectional |
2019 |
131 |
61.3 ±14.7 |
70.2%/29.8% |
5.6 years |
|
Wang et al., (21) |
China |
2022 |
Cross-sectional |
2021-2022 |
236 |
Median 64.5 years |
63.6%/36.4% |
NR |
|
Wang et al., (22) |
China |
2023 |
Cross-sectional |
2022 |
305 |
≥ 18 years old |
63%/37.1% |
2-5 years |
|
Zhou MG et al., (23) |
China |
2023 |
Cross-sectional |
2022 |
167 |
60 years and above |
66.47%/33.53% |
Mean: 56.25 months |
NR: Not reported
Study outcome measures
Palliative Care Needs: The studies reviewed highlight significant palliative care needs among hemodialysis patients. Weisbord et al. found that both patients and nephrologists rated palliative care interventions favorably, with 68% of patients and 76% of nephrologists considering them worthwhile (15). Saeed et al. reported that 46% of Pakistani patients preferred treatment focused on comfort and symptom management over life extension, emphasizing the need for better-informed dialysis decision-making and access to palliative care services (18). Liem et al. also observed a clear need for palliative care provision, while Wang et al. categorized patients into three classes based on the severity of their palliative care needs, with nearly half having moderate to severe needs (20, 22) (Table 3).
Symptom Burden: Symptom burden among hemodialysis patients is substantial and varied. Weisbord et al. identified the most frequently reported symptoms as lack of energy (74%), drowsiness (63%), and numbness/tingling (63%) (15). Lowney et al. reported high prevalence of weakness (78%), pain (64%), and poor mobility (66%) (16). Wang et al. noted that older patients experienced higher symptom burdens, including dry mouth (91.5%) and itching (83.1%) (21). Zhou MG et al. highlighted dry skin, dry mouth, and itching as the most common symptoms, with dry skin being particularly severe (23) (Table 3).
|
Table 3. Comprehensive outcomes of palliative care needs and symptom burden management in patients undergoing maintenance hemodialysis |
||||
|
Author |
Palliative care needs |
Symptom burden |
Quality of life |
Symptom severity |
|
Weisbord et al., (15) |
- Patient satisfaction: 68% rated the intervention as worthwhile. - Nephrologist satisfaction: 76% rated the intervention as worthwhile. - Both patient and Nephrologist perceive palliative care favorably. |
Most frequently reported: lack of energy (74%) Drowsiness (63%) Numbness/tingling (63%) Dry mouth (58%) Pain (53%) Itching (53%) Most prevalent: Pain and numbness/tingling (79%) Phycological: worrying (32%) Feeling and sad (26%) Feeling irritable (26%) Feeling nervous (26%) Severe: constipation, pain, difficulty sleeping, itching, dry mouth
|
- Significantly impaired among patients. - Lower HRQOL scores were correlated with increased symptom prevalence for all FACIT SP domains except emotional well-being. |
NR |
|
Lowney et al., (16) |
NR |
Weakness: 78% (95%CI: 75%-81%) Pain: 64% (95%CI: 61%-67%) Poor mobility: 66% (95%CI:63%-69%)
|
Poor HRQOL in the hemodialysis population. Significantly and independently associated with poor mobility and pain. Providing physiotherapy and occupational therapy can help improve their quality of life. |
-Severe/overwhelming weakness: 20% (95% CI 18%-23%), -Severe/overwhelming pain: 16% (95% CI 14%-18%), - Severe/overwhelming mobility issues: 19% (95% CI 16%-22%) -Gastrointestinal issues: (mouth problems, diarrhea, vomiting, constipation, nausea: 20%-40%) -depression: 44% (95%CI:40%-47%) -anxiety: 40% (95%CI:37%-44%) |
|
Chen et al., (17) |
palliative care services were used in only a minority of patients (34.35%). hemodialysis duration (OR: 1.19 per year; 95% CI:1.10- 1.3; P<0.001), hospitalization within 30 days of death (OR: 5.78; 95% CI: 2.62 - 12.73; P<0.001), and death in hospital (OR: 1.92; 95% CI:1.13 -3.27; P=0.02). |
NR |
NR |
NR |
|
Saeed et al., (18) |
46% preferred treatment focused on comfort and symptom management over life extension. Pakistani patients need better informed dialysis decision making, EOL care and access to palliative care services. |
NR |
More patients preferred a treatment plan focusing on improving QOL (47%) rather than prolonging life extension. |
NR |
|
Gunarathne et al., (19) |
NR |
Using regression analysis: - - At baseline: elevated stress (β = 0.65, p= <0.005) and illness perception level (β = 0.21, p = 0.02) -At 6 months: high stress (β = 0.28, p = 0.003) and illness perception level (β = 0.2, p = 0.03), poor social support (β = −0.22, p = 0.01) and low body weight (post dialysis weight) (β = −0.2, p = 0.03). |
NR |
NR |
|
Liem et al., (20) |
A clear need for palliative care provision was observed |
MFI-20 mean (SD) General fatigue 14.5 (4.2) |
SF 36: - Physical functioning: 53.2 (28.1), p=0.958 Role physical: 27.8 (36.9), p=0.296, general health (P ≤ 0.000), vitality (P = 0.009), social functioning (P = 0.001), mental health (P = 0.007), and mental component (P = 0.005) |
NR |
|
Wang et al., (21) |
POS score: median (IQR)=16(12-23) Older patients had higher median POS scores than younger patients (P < 0.01). POS items: Pain(p=0.009), family anxiety(p=0.009), information needs(p=0.081), support(p<0.001), practical matters(p<0.001), other symptoms, (p=0.001) and wasted time(p=0.850). |
older patients vs. younger patients (16.02 ± 5.10 vs. 14.07 ± 4.86, P < 0.01) Dry mouth (91.5%), itching (83.1%), dry skin (82.2%), feeling tired or lacking energy (86.4%) |
HRQOL: Median (IQR): 0.78(0.61-0.78) older patients vs. younger patients: (0.71vs.0.78, p<0.01) POS scores positively correlated with overall symptom burden and severity (p,0.05 and p<0.01) POS scores negatively correlated with HRQOL(P,0.01) |
Median (IQR):59(52-71) Age: older patients vs. younger patients (61 vs. 55.5 P < 0.01) Dry mouth(p=0.017), itching (p=0.043) and dry skin(p>0.05), feeling tired or lack of energy(p=0.005), Trouble staying asleep(p=0.025)
|
|
Wang et al., (22) |
Class 1: mild palliative care needs (n = 154, 50.5%). Mean POS score:11.77±3.98. Class 2, moderate palliative care needs (n = 89, 29.2%); Mean POS score:19.67±3.52, Class 3, severe palliative care needs (n = 62, 20.3%). Mean POS score: 28.60±3.3 |
Class1: 12.27 ± 4.55 Class2: 15.73 ± 4.11 Class3: 20.45 ± 3.07 |
The study found that nearly half of ESRD patients on MHD have moderate to severe palliative care needs, which negatively impact their QOL. |
Class1: 23.19 ± 9.10 Class2: 32.88 ± 10.17 Class3: 49.19 ± 10.0 |
|
Zhou MG et al., (23) |
NR |
The symptom burdens with the highest scores were dry skin (2.47±1.61), dry mouth (2.18±1.60), itching (2.14±1.58), and trouble staying asleep (1.90±1.67). |
NR |
The symptom severity with the highest scores were trouble staying asleep (1.47±1.41), dry skin (1.38±1.08), itching (1.37±1.17), trouble falling asleep (1.34±1.47), dry mouth (1.28±1.05) greatest distress was itching (2.83±1.99) |
POS: Palliative outcome scale, OBS: Overall, Burden of Symptoms, Overall Symptoms Severity Score: OSSS, NR: Not reported, QOL: quality of life, MHD: Maintenance Hemodialysis, ESRD: end stage renal disease, HRQOL: health related quality of life, IQR: Inter quartile range
Quality of Life: QoL is significantly impaired among hemodialysis patients due to the high symptom burden. Weisbord et al. found that lower health related quality of life (HRQoL) scores was correlated with increased symptom prevalence in all domains except emotional well-being (15). Lowney et al. indicated that poor mobility and pain were significantly associated with poor HRQoL, suggesting that interventions like physiotherapy and occupational therapy could improve QoL (16). Wang et al. observed that older patients had lower HRQoL scores compared to younger patients, and that higher POS scores were negatively correlated with HRQoL, indicating a direct relationship between symptom burden and QoL (21) (Table 3).
Symptom Severity: The severity of symptoms further impacts the lives of hemodialysis patients. Weisbord et al. reported severe symptoms such as constipation, pain, difficulty sleeping, and itching (15). Lowney et al. highlighted that severe or overwhelming symptoms, including weakness (20%) and pain (16%), were prevalent (16). Wang et al. detailed varying symptom severity among different classes of patients, with those having severe palliative care needs experiencing significantly higher symptom severity scores (22). Zhou MG et al. found that the symptoms causing the greatest distress were trouble staying asleep and itching, which significantly affect patient comfort and well-being (23) (Table 3).
Discussion
This study evaluated the need for palliative care and assessed the symptom burden among patients receiving hemodialysis. Findings highlight significant palliative care needs among hemodialysis patients and emphasize positive perceptions of palliative care interventions among patients and nephrologists, underscoring their value while comfort-focused treatment, was prioritized defining the necessity for improved decision-making and access to palliative care services in dialysis settings. Additionally, research identified varied levels of palliative care needs among patients, with a notable proportion experiencing moderate to severe requirements.
Need for palliative care
As our results demonstrate and highlight, there is a significant need for palliative care for patients receiving hemodialysis. Grubbs et al. highlighted instances of specific clinical situations involving maintenance dialysis patients with limited life expectancy where a palliative approach to dialysis care could be appropriate, including: (1) a patient on maintenance dialysis who experiences a sudden severe illness leading to a significant decline in life expectancy, (2) a patient initiated on dialysis due to acute kidney injury with uncertain life expectancy and unclear goals of care, and (3) a maintenance dialysis patient experiencing progressive decline in physical or cognitive function. In adopting a palliative approach to dialysis care in these cases, the transition would typically begin with discussions focused on clarifying and aligning with the patient's goals of care (24). Moreover, in their review authors further emphasized that to demonstrate the necessity for a palliative approach to dialysis treatment, it is critical to highlight the significant morbidity and mortality among maintenance dialysis patients. The dialysis population has an adjusted 1-year survival rate of 76%, but only 36% over 5 years. Maintenance dialysis patients had an adjusted mortality rate that is approximately double that of adults with cancer and more than double that of individuals with congestive heart failure or stroke. Given the high incidence of advanced age, severe comorbid diseases, and the high death rate among the ESKD population, a significant proportion of patients undergoing maintenance dialysis may be nearing the end of life and could be candidates for a palliative approach to dialysis care (24).
Likewise, Sturgill et al. narrated patients with advanced CKD, especially ESKD, have a life-threatening condition characterized by high morbidity and mortality, and consequently should be considered for early management by palliative care experts. However, the average CKD patient lacks an advanced care plan, experiences several disabling symptoms, and does not seek hospice care at the end of life (25). Another review by Kurella et al. also indicated that palliative care should be better integrated into advanced CKD and dialysis care to meet the needs of these patients who have many comorbidities, a high symptom burden, and a limited life expectancy. However, most ESKD patients who get continuous dialysis do not have access to specialized palliative care services (12). The studies from the literature align well with our findings of a significant need for palliative care among hemodialysis patients; however, it is noteworthy that studies in the current literature further demonstrated the inadequate provision and utilization of palliative care in this vulnerable cohort due to various barriers and challenges. One study included in our review indicated that palliative care was utilized by only a minority of patients (17), although we did not specifically evaluate the barriers and challenges as it was considered beyond the scope of this review. Therefore, further research should address these factors comprehensively to ensure optimal care through effective implementation and utilization of palliative care services.
Similarly, findings from a qualitative study described that palliative care have been insufficient for patients with ESKD on dialysis, and they have a high rate of hospitalization and intensive care demands near the end of life. Even if death is inevitable, patients have unmet palliative care requirements. Furthermore, family members regarded these patients' end-of-life care as substantially poorer than that of individuals with cancer or dementia. Dialysis experts have also noted a lack of quality care, citing unmet needs such as end-of-life care talks and grief assistance. The impediments to the start of palliative care may be the unknown prognosis of chronic diseases, lack of practical expertise, and difficult decision-making (26). Imamah et al. reported in their meta-synthesis that palliative care for patients with ESKD consists of advance care planning, pain and symptom treatment, and grief support. The majority of ESKD patients understand the need to be prepared for death. Few patients initiate the end-of-life conversation at the outset of dialysis. Most of them begin during dialysis or when individuals become unwell (27).
While further analyzing various barriers for the effective implementation and practice of palliative care from literature, Chu et al. defined several barriers hindering the provision of effective palliative care, including prognostic issues, delayed referrals, cultural misconceptions, a lack of physician trust, and poor coordination among healthcare specialists. Integrating palliative care into routine renal treatment, as well as promoting open communication among healthcare personnel, are critical strategies for improving the quality of life and end-of-life care for hemodialysis patients. By embracing novel solutions and encouraging collaboration, healthcare practitioners can provide better patient-centered, holistic care that addresses the complicated demands of seriously ill patients in an aging population receiving hemodialysis (28). Additionally, Lanini et al. suggested early palliative treatment can improve quality of life while additionally supporting families. Renal patients often have a shorter life expectancy; thus, they can benefit from palliative care, which is a well-defined concept, particularly for CKD rather than acute kidney injury. Indeed, several therapeutic techniques can be used to improve the quality of life in CKD patients such as palliative dialysis and conservative care. All of these procedures necessitate close coordination among healthcare providers, patients, and families. Everyone involved must agree on the prognosis, reasonable treatment goals, and therapeutic decisions. The literature contains limited and insufficient data on the effects of palliative and hospice care on acute kidney injury patients. Hence, methodological, ethical, and clinical efforts are required to implement knowledge and awareness (29).
Evaluation of symptom burden and quality of life
Furthermore, results of this study indicate the burden of symptoms among hemodialysis patients is extensive and diverse, encompassing issues like fatigue, pain, and itching, which are particularly pronounced among older individuals. These symptoms significantly impair patients' quality of life, with lower scores in HRQoL associated with higher symptom prevalence, especially affecting mobility and emotional well-being. Older patients generally report poorer quality of life, indicating age-related differences in their experience. Moreover, symptom severity varies widely among patients, with certain symptoms such as sleep disturbances and itching posing significant challenges to patient comfort and well-being. These findings underscore the complex symptom management needs within the hemodialysis population. Similarly, another review by Bonillia-Sierra et al. highlighted that the most prevalent symptoms that disturb individuals and cause them distress in their daily lives are those linked to well-being, difficulties falling asleep, and itching. Hence, health professionals must modify care measures and assist patients undergoing renal treatment, particularly those who have had the condition for a longer period of time, in order to lessen their suffering and thereby enhance their daily quality of life. To this goal, an early palliative care plan could be developed (30). Results of another meta-synthesis showed deterioration caused changes in physical, emotional, and social status. Most studies indicated that functional status modifications included discomfort and insomnia, shortness of breath, nausea and vomiting, and fatigue (27).
Additionally, a survey by Lykke et al. reported the prevalence rates were 24.8% moderate to severe fatigue, 38.0% pain, 32.6% anxiety, and 29.5% depression. The incidence of coexisting moderate to severe symptoms ranged between 15.5% and 25.6% (31). A qualitative study also revealed that participants reported cramps, fatigue, depression, and itching as the most common symptoms. Negotiating fluid withdrawal with dialysis personnel helps to alleviate cramps. To reduce fatigue, some participants tried adjusting their dialysis days and shifts. The majority of individuals reported experiencing depression early in their dialysis treatment; for some, it was a continuous or recurring condition. Few individuals reported taking antidepressants or seeking counseling to cope with depression. Itching was quite unpleasant for individuals who experienced it regularly. Some participants suggested that topical therapies, antihistamines, dietary adjustments, and phosphate binders could be beneficial (32). Another cross-sectional study also demonstrated that fatigue, cold aversion, pruritus, lower torso weakness, and difficulties sleeping were both groups' most common and severe symptoms. Both groups had considerable reductions in their quality of life. All quality-of-life domain scores showed a negative correlation with the number of symptoms (P < 0.001). ESRD patients receiving palliative care and dialysis had similar symptom prevalence and intensity, a significant symptom burden, and a lower quality of life (33). Our findings are in context with these findings, typically reflecting an increased prevalence of fatigue, pain, and itching in this cohort of patients; furthermore, it is observed that increased symptomatic burden significantly affects and impairs the QoL of patients receiving hemodialysis, as indicated by almost all of the included studies in this review.
Rao et al. explained the increased prevalence of insomnia/sleeplessness among these patients. Sleep difficulties appear at an early stage of CKD, impacting both the duration and quality of sleep. In terms of intensity and severity, insomnia ranks among the top five most problematic symptoms reported. The prevalence ranges from 20% to 83% in CKD patients and 50% to 75% in ESRD patients, with daytime drowsiness being the most concerning. Sleep problems reduce quality of life, exacerbate health risks such as immune system degradation and cardiovascular disease, and increase mortality. It can also cause impaired neurocognition, including difficulty paying attention and poor work performance. Insomnia in CKD has both physical and psychological reasons, and it can be treated pharmacologically as well as non-pharmacologically (34).
This study stands out due to its comprehensive and rigorous approach to synthesizing existing research. By systematically evaluating a broad range of studies, it provides a thorough assessment of the palliative care needs and symptom burden experienced by hemodialysis patients. This methodical process ensures high-quality evidence is included and analyzed, revealing important patterns and trends that might not be apparent in individual studies. The review identifies key gaps in the current literature, offering valuable insights that can guide future research and improve clinical practice. Its transparency and reproducibility ensure the reliability and credibility of its findings and defines the strengths of this paper.
Limitations and future research directions
However, despite its strengths, this study has several limitations. Firstly, the inclusion of the study by Saeed et al. may restrict the generalizability of our findings because it involved a mixed population. Nevertheless, this study was included in our review since 98% of its participants were on hemodialysis, and we aimed to ensure that no potentially relevant research was overlooked (18). The quality of the included studies also varies which can affect the reliability of the review’s conclusions. Other limitations include potential language bias, as studies published only in English are included, and the possible exclusion of recent research due to publication delays. Variability in definitions and measures of palliative care needs and symptom burden across studies can lead to inconsistencies in findings. Lastly, confounding factors such as differences in patient characteristics among studies can influence the interpretation of results and limit their generalizability. Despite these limitations, the review provides valuable insights into palliative care needs and symptom burden for hemodialysis patients. Its comprehensive synthesis of existing evidence and identification of key trends and gaps make it a significant contribution to the field, justifying its publication and offering important guidance for future research and clinical practice.
Future research should focus on conducting high-quality, prospective studies specifically targeting hemodialysis patients to better understand their palliative care needs and symptom burden. Research should aim to standardize definitions and measurement tools for symptoms and palliative care needs to improve comparability across studies. Additionally, investigating the effectiveness of various palliative care interventions tailored to this population could provide insights into effective strategies for symptom management and quality of life improvement. Future studies should also consider diverse patient demographics and settings to enhance the generalizability of findings. Addressing the current gaps in the literature, such as the need for updated evidence and inclusion of recent research, will also be crucial. Furthermore, exploring patient and caregiver perspectives on palliative care can provide a more comprehensive understanding of the needs and challenges faced by hemodialysis patients.
Conclusion
This systematic review underscores the significant palliative care needs of hemodialysis patients, highlighting a strong preference for palliative care interventions among these patients. The review also identifies that many patients experience a moderate to severe burden of symptoms, including fatigue, pain, and insomnia and itching, and these symptoms markedly impact patients' quality of life, with reduced HRQoL scores linked to higher symptom prevalence, affecting mobility and emotional well-being. Future research should focus on standardizing measures of palliative care needs, evaluating the effectiveness of tailored interventions, and addressing gaps in current evidence to improve palliative care delivery and patient outcomes in hemodialysis settings.
Disclosures
Author Contributions
The author has reviewed the final version to be published and agreed to be accountable for all aspects of the work.
Ethics Statement
Not applicable
Consent for publications
Not applicable
Data Availability
All data is provided within the manuscript.
Conflict of interest
The authors declare no competing interest.
Funding
The author has declared that no financial support was received from any organization for the submitted work.
Acknowledgements
Not Applicable