Volume 4, Issue 5
May 2024
Lifestyle Modification and Medical Treatment of Long QT Syndrome
Mishari Alharbi, Islam Ibrahim, Sultan Alzahrani, Fahad Hamdi, Wesam Dause, Mohammed Alshammakh, Rakan Aun, Mohannad Howladar, Bayan Laban, Abdulrahman Almalki
DOI: http://dx.doi.org/10.52533/JOHS.2024.40501
Keywords: Long QT Syndrome, arrhythmias, lifestyle modifications, pharmacological treatments, genetic testing
Long QT Syndrome (LQTS) is a genetic or acquired cardiac disorder characterized by a prolonged QT interval on an electrocardiogram, predisposing individuals to life-threatening arrhythmias and sudden cardiac death. Management of LQTS involves both lifestyle modifications and pharmacological treatments to mitigate risks and enhance patient outcomes. Lifestyle interventions include avoiding strenuous physical activities, especially swimming, and managing emotional stress to prevent arrhythmic triggers. Dietary modifications, such as maintaining adequate levels of potassium and magnesium, are essential to stabilize the heart's electrical activity. On the pharmacological front, beta-blockers like propranolol and nadolol are the mainstay treatments, effectively reducing heart rate and adrenergic stimulation, thus minimizing arrhythmic events. Sparings where beta-blockers are insufficient, additional medications like mexiletine, and potassium-sparing diuretics are used to manage the condition. High-risk patients benefit from implantable cardioverter-defibrillators (ICDs), which provide immediate intervention during severe arrhythmic episodes. Combining lifestyle changes with pharmacological treatments offers a comprehensive approach to LQTS management, significantly lowering the incidence of arrhythmias and improving overall patient prognosis. Patient education and regular follow-up are crucial to ensure adherence to treatment plans and timely adjustments. Advances in genetic testing facilitate personalized medicine, allowing for tailored treatment strategies based on individual genetic profiles. This integrated approach enhances the effectiveness of LQTS management, providing a holistic solution to a complex cardiac condition.
Introduction
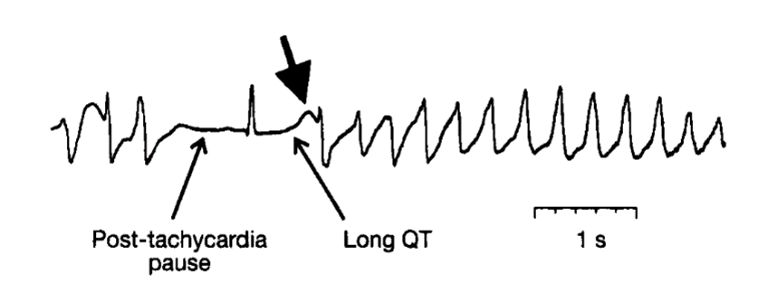
Long QT Syndrome (LQTS) is a cardiac disorder characterized by prolonged repolarization of the heart's electrical cycle, which can be identified by a lengthened QT interval on an electrocardiogram (ECG). This condition predisposes individuals to life-threatening arrhythmias such as torsades de pointes (Figure 1) and sudden cardiac death (SCD) (1). LQTS can be congenital, resulting from genetic mutations affecting cardiac ion channels, or acquired, often due to electrolyte imbalances or medication effects. The management of LQTS is multifaceted, involving lifestyle modifications and medical treatments to reduce the risk of arrhythmias and improve patient outcomes (2).

Figure 1: Cycle length changes at the initiation of a typical episode of torsade de pointes (3).
Lifestyle modifications play a crucial role in managing LQTS, as certain activities and environmental factors can trigger arrhythmic events. For instance, individuals with LQTS are advised to avoid strenuous physical activities, particularly swimming, which has been associated with a higher risk of SCD in LQTS patients (4). Additionally, stress management techniques are recommended since emotional stress and sudden fright can precipitate arrhythmias in susceptible individuals. Dietary adjustments, such as maintaining adequate levels of potassium and magnesium, are also important, as these electrolytes are essential for proper cardiac function and can help stabilize the heart's electrical activity (4).
Medical treatments for LQTS primarily aim to reduce the occurrence of arrhythmias and prevent SCD. Beta-blockers, such as propranolol and nadolol, are the cornerstone of pharmacological management, as they decrease the heart rate and reduce the risk of arrhythmias by minimizing adrenergic stimulation (5). In cases where beta-blockers are insufficient or contraindicated, other antiarrhythmic drugs like mexiletine, or potassium-sparing diuretics may be considered. Additionally, implantable cardioverter-defibrillators (ICDs) are recommended for high-risk patients, particularly those with a history of cardiac arrest or syncope, as they provide immediate defibrillation in the event of life-threatening arrhythmias (5).
The integration of lifestyle modifications and medical treatments is essential for the comprehensive management of LQTS. This combined approach helps to mitigate the risk factors associated with the condition while providing effective therapeutic interventions to maintain cardiac stability. Moreover, patient education and regular follow-up are critical components in ensuring adherence to treatment plans and promptly addressing any emerging issues. Continued research and advancements in genetic testing are also enhancing our understanding of LQTS, allowing for more personalized and effective management strategies. This review aims to discuss Lifestyle modification and medical treatment of LQTS.
Review
The management of LQTS through lifestyle modification and medical treatment remains critical in reducing the risk of arrhythmias and sudden cardiac death. Lifestyle modifications, such as avoiding strenuous physical activities and stress management, are essential preventative measures for patients with LQTS (6). These modifications help to minimize the triggers that can precipitate life-threatening arrhythmias. In addition to lifestyle changes, the use of beta-blockers has proven to be a cornerstone in the pharmacological management of LQTS. Beta-blockers, including propranolol and nadolol, are effective in decreasing the heart rate and reducing the risk of arrhythmic events by limiting adrenergic stimulation (7). The integration of lifestyle modifications with pharmacological treatments offers a comprehensive approach to managing LQTS. This dual strategy not only helps in preventing arrhythmias but also enhances the overall quality of life for patients. ICDs provide an additional layer of protection for high-risk patients, ensuring immediate intervention during severe arrhythmic events. Patient education and regular follow-up are paramount to ensure adherence to treatment plans and to address any emerging issues promptly. Ongoing research and advancements in genetic testing are further improving the personalization and effectiveness of LQTS management strategies (7).
Lifestyle Modifications for Long QT Syndrome
Lifestyle modifications are a crucial component in the management of LQTS. These non-pharmacological strategies are designed to minimize the risk of arrhythmias and sudden cardiac death by addressing various triggers and environmental factors. The role of lifestyle changes in managing LQTS cannot be overstated, as they complement medical treatments and enhance overall patient outcomes (8).
One of the primary lifestyle modifications for individuals with LQTS is the avoidance of strenuous physical activities, particularly competitive sports. Physical exertion can significantly increase the risk of arrhythmic events, especially in genetically predisposed individuals. Activities such as swimming are particularly risky due to the potential for sudden immersion-related arrhythmias. Patients are advised to engage in moderate physical activity, which has been shown to be safer and beneficial for overall cardiovascular health (9). Emotional stress and sudden fright are also known to precipitate arrhythmias in individuals with LQTS. Therefore, stress management techniques are highly recommended. These may include practices such as mindfulness meditation, yoga, and other relaxation techniques that help to reduce sympathetic nervous system activation. By managing stress effectively, patients can lower their overall risk of arrhythmic episodes (10).
Dietary adjustments play a significant role in the lifestyle management of LQTS. Maintaining adequate levels of electrolytes, particularly potassium and magnesium, is essential for stabilizing the heart's electrical activity. These electrolytes are crucial in maintaining proper cardiac function and preventing the prolongation of the QT interval. Patients are encouraged to consume a balanced diet rich in fruits, vegetables, and whole grains, and to avoid excessive intake of processed foods and caffeinated beverages, which can exacerbate arrhythmic tendencies (11). Another important lifestyle consideration is the use of medications and substances that can prolong the QT interval. Patients with LQTS should be educated about the potential dangers of certain prescription medications, over-the-counter drugs, and herbal supplements that can interfere with cardiac repolarization. Healthcare providers should regularly review all medications taken by LQTS patients to ensure they do not pose additional risks. Additionally, the avoidance of recreational drugs and excessive alcohol consumption is strongly advised (12).
Finally, ensuring a safe environment is vital for patients with LQTS. This includes educating family members and close contacts about the condition and the appropriate steps to take in the event of a cardiac emergency. Access to automated external defibrillators (AEDs) at home and in community settings can provide an added layer of safety, particularly for high-risk individuals. Lifestyle modifications are an integral part of managing LQTS. By avoiding physical and emotional stressors, maintaining a balanced diet, carefully managing medication use, and ensuring a safe environment, patients with LQTS can significantly reduce their risk of life-threatening arrhythmias. These strategies, when combined with medical treatments, offer a comprehensive approach to managing this complex cardiac condition.
Pharmacological Interventions and Their Efficacy
Pharmacological interventions play a pivotal role in the management of LQTS, aiming to reduce the risk of arrhythmias and sudden cardiac death. These treatments primarily involve the use of beta-blockers, antiarrhythmic drugs, and other supportive medications that help stabilize cardiac electrical activity and prevent the occurrence of life-threatening arrhythmias (13). Beta-blockers are considered the cornerstone of pharmacological therapy for LQTS. These medications, such as propranolol and nadolol, function by inhibiting the effects of adrenaline on the heart, thereby reducing heart rate and mitigating the risk of arrhythmic events. Beta-blockers have been shown to be particularly effective in patients with congenital LQTS, significantly decreasing the incidence of syncope, torsades de pointes, and sudden cardiac death. The efficacy of beta-blockers has been well-documented in various studies, which highlight their ability to provide substantial protection against arrhythmias when taken consistently and as prescribed (7).
In addition to beta-blockers, other antiarrhythmic medications may be employed to manage LQTS, especially in cases where beta-blockers are either insufficient or contraindicated. Mexiletine, a sodium channel blocker, is one such drug that has demonstrated efficacy in shortening the QT interval and reducing arrhythmia risk in LQTS patients. By modulating the sodium channels in the heart, mexiletine helps stabilize the cardiac repolarization process, thereby minimizing the likelihood of arrhythmic episodes. Potassium-sparing diuretics, such as spironolactone and eplerenone, are also utilized to maintain optimal electrolyte levels and prevent hypokalemia, which can exacerbate QT prolongation and arrhythmic risk (11). ICDs represent another critical component of the pharmacological management strategy for LQTS, particularly for high-risk patients who have experienced cardiac arrest or recurrent syncope despite optimal medical therapy. ICDs provide immediate defibrillation in the event of a severe arrhythmic episode, thereby offering a lifesaving intervention for those at greatest risk of sudden cardiac death. The combination of pharmacological treatments and ICDs has been shown to improve survival rates and quality of life for LQTS patients, underscoring the importance of a comprehensive treatment approach (2).
Moreover, ongoing research continues to explore novel pharmacological strategies for LQTS. Genetic insights into the specific ion channel mutations associated with different types of LQTS have paved the way for targeted therapies that aim to correct the underlying genetic defects. Such advancements hold promise for more personalized and effective treatment regimens, tailored to the individual genetic profiles of patients with LQTS. Pharmacological interventions are integral to the effective management of Long QT Syndrome. Beta-blockers, antiarrhythmic drugs, and supportive medications collectively help to stabilize cardiac function and reduce the risk of life-threatening arrhythmias. The addition of ICDs further enhances patient safety, particularly for those at high risk of sudden cardiac death. As research progresses, the potential for targeted pharmacological therapies offers hope for even more precise and effective management of this complex condition.
Combining Lifestyle and Medical Treatments for Optimal Management
The optimal management of LQTS requires a holistic approach that integrates both lifestyle modifications and medical treatments. This dual strategy ensures that patients receive comprehensive care, addressing both the triggers of arrhythmic events and the underlying cardiac instability. The synergy between lifestyle changes and pharmacological interventions is vital for reducing the risk of life-threatening arrhythmias and improving patient outcomes (14).
Lifestyle modifications play a foundational role in the management of LQTS. Avoiding triggers such as strenuous physical activity and emotional stress is crucial for minimizing the risk of arrhythmias. Patients are advised to engage in moderate physical exercise, which can be safely incorporated into their daily routines. Additionally, dietary adjustments that ensure adequate levels of potassium and magnesium help maintain cardiac electrical stability. These modifications, when adhered to consistently, can significantly lower the incidence of arrhythmic events (15). Medical treatments, particularly the use of beta-blockers, are essential for managing LQTS. Beta-blockers, such as propranolol and nadolol, effectively reduce heart rate and adrenergic stimulation, thus decreasing the likelihood of arrhythmias. For patients who do not respond adequately to beta-blockers, other medications like mexiletine and potassium-sparing diuretics can be considered. These drugs help to stabilize cardiac ion channels and prevent electrolyte imbalances, further reducing arrhythmic risk (15).
The integration of lifestyle modifications with pharmacological treatments offers a robust management strategy for LQTS. This combined approach ensures that patients are not solely reliant on medications but also actively participate in their own care through lifestyle adjustments. The effectiveness of this integrated strategy is well-documented, with studies showing that patients who adhere to both lifestyle changes and medical treatments experience fewer arrhythmic events and have better overall outcomes (16). Patient education is a critical component of this comprehensive management plan. Educating patients about the importance of lifestyle modifications and medication adherence empowers them to take an active role in managing their condition. Regular follow-up appointments with healthcare providers are necessary to monitor patient progress, adjust treatment plans as needed, and address any emerging issues. These follow-ups also provide an opportunity to reinforce the importance of adherence to both lifestyle and medical recommendations.
Advancements in genetic testing and personalized medicine are further enhancing the management of LQTS. By identifying specific genetic mutations responsible for the condition, healthcare providers can tailor treatments to the individual needs of each patient. This personalized approach ensures that patients receive the most effective combination of lifestyle and medical interventions, maximizing their chances of long-term success and improved quality of life (17). The combination of lifestyle modifications and medical treatments is essential for the optimal management of Long QT Syndrome. This integrated approach addresses the multifaceted nature of the condition, providing patients with a comprehensive strategy to reduce arrhythmic risk and enhance cardiac stability. Ongoing patient education, regular follow-up, and advancements in personalized medicine are key to achieving the best possible outcomes for individuals with LQTS.
Conclusion
The optimal management of LQTS requires a comprehensive approach that integrates lifestyle modifications and medical treatments to effectively reduce arrhythmic risk and improve patient outcomes. Ongoing patient education and advancements in personalized medicine are essential for achieving long-term success. This combined strategy ensures holistic care for individuals with LQTS.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.