Volume 4, Issue 1
January 2024
The Relation Between the Patellar Alignment and the Curvature of Lumbar Lordosis in Patients with Chronic Patellofemoral Pain Syndrome
Nader I. El-Sayed, Mohamed A. Behiry, Ahmed M.Abd Elkhalek, Aya R. Serag, Ranim A. El-Masry, Ahmed E. Hassan, Norah Abdullah M. Alqahtani, Saad S. Abokhdaah, Sarah M. Albejad, Rafeef Hassan M Asiri, Ahmed M.N. Tolba, Menna M. Ghoniem, Muhammad Ahmed Shady
DOI: http://dx.doi.org/10.52533/JOHS.2024.40101
Keywords: Patellofemoral pain syndrome, Anterior knee pain, Chondromalacia patellae, lumbar lordosis, patella femoral index, patellofemoral angle, cobb angle
Background: Patellofemoral Pain Syndrome (PFPS) is characterized by localized anterior knee pain, impacting around 11–17% of patients seeking medical attention. This condition is commonly associated with activities that place heightened stress on the patella, such as ascending and descending stairs, jumping, running, and squatting. The primary objective of the present study is to explore the correlation between patellar alignment and lumbar lordosis curvature in individuals diagnosed with chronic patellofemoral pain syndrome. This investigation aims to provide valuable insights into the intricate relationship between knee and spine conditions, contributing to a better understanding of potential factors influencing PFPS and its management.
Methods: The cross-sectional study was conducted from March 2023 to August 2023 at Mansoura, Dakahleya,Egypt. The target population comprised individuals aged 20 to 45 with chronic patellofemoral pain exhibiting a positive McConnell test. Exclusions encompassed individuals with knee osteoarthritis, ligament, or meniscal injuries, patellar or knee fractures, and those with a history of spinal surgery such as spinal fractures or scoliosis.
Results: The mean values for age, weight, height, and BMI were 26.20 ±6.00 years, 81.94 ±4.37 kg, 170.26 ±3.08 cm, and 28.23 ±1.64 kg/m2, respectively. No significant correlation (r = 0.02; P = 0.922; P > 0.05) was observed between Cobb angle and patella femoral index. However, a significant positive correlation (r = 0.64; P = 0.002; P < 0.05) was identified between the Cobb angle and the lateral patellofemoral angle.
Conclusion: The study disclosed a notable association between the Cobb angle and the lateral patellofemoral angle in patients with chronic patellofemoral pain syndrome. The lateral displacement of the patella observed in these individuals contributes to alterations in patellar-femoral joint dynamics, resulting in decreased patellofemoral contact area and increased pressure on the lateral facets of the patella. Further research and longitudinal studies are imperative to deepen our understanding of causative factors and explore potential interventions for chronic patellofemoral pain syndrome.
Introduction
Patellofemoral Pain Syndrome (PFPS) is characterized by localized anterior knee pain, affecting approximately 11–17% of patients seeking medical attention (1). This condition is commonly associated with activities that impose heightened stress on the patella, such as ascending and descending stairs, jumping, running, and squatting (2, 3). This prevalent syndrome poses considerable challenges due to its intricate interplay of factors impacting the knee joint. Notably, activities that intensify the stress on the patella are pivotal in understanding the etiology of PFPS. Symptoms include crepitus and mild to moderate joint effusion (1). The primary causes of PFPS are related to the alignment and orientation of the patella. Deviations in patellar orientation can lead to excessive pressure on specific areas of the femur, resulting in pain, inflammation, and discomfort around the knee (4, 5). Deviations in patellar alignment not only disrupt the normal biomechanics of the knee but also generate excessive pressure on specific regions of the femur, fostering an environment conducive to pain and inflammation. Chondromalacia patellae, characterized by pathological changes in the articular cartilage of the patella involving softening and fibrillation, is one of the contributors to PFPS (5-7). The involvement of chondromalacia patellae adds another layer of complexity to PFPS. The pathological changes in the articular cartilage of the patella, marked by softening and fibrillation, contribute significantly to the discomfort and joint dysfunction experienced by individuals with PFPS.
The assessment of the sagittal alignment of the lumbar curve, a procedure commonly conducted through radiological means such as X-rays, holds pivotal significance in the understanding and diagnosis of various conditions affecting the lower back. This radiological evaluation, particularly employed to ascertain lumbar lordosis, provides valuable insights into conditions such as low back pain, lumbar spondylosis, spondylolisthesis, and scoliosis (8). The radiological examination of lumbar lordosis through X-rays proves instrumental in unraveling the complexities of conditions plaguing the lower back. Low back pain, a prevalent and multifaceted issue, often finds its roots in deviations from the normative lumbar lordosis range. Lumbar spondylosis, characterized by degenerative changes in the spine, and spondylolisthesis, involving the forward displacement of vertebrae, both exhibit distinctive signatures in lumbar lordosis configurations, thus necessitating precise radiological assessments. In healthy adults, lumbar lordosis typically ranges from 40 to 50 degrees, measured by the Cobb angle (9). The lumbar spine inherently adopts a lordotic curvature, a key biomechanical feature discerned through its articulation with the sacrum. This lordotic curve serves as a compensatory mechanism to counterbalance the sacral inclination, thereby upholding an upright orientation within the spinal column (10). Moreover, the evaluation of lumbar lordosis is integral in understanding and managing scoliosis, a condition marked by abnormal lateral curvature of the spine. By scrutinizing the sagittal alignment, healthcare professionals can discern the extent and nature of these spinal irregularities, guiding tailored interventions and treatment plans.
Numerous factors contribute to the variability of lumbar lordosis, encompassing elements such as age, gender, pregnancy, obesity, congenital spine deformities, and muscle imbalances (11). Extensive research suggests a noteworthy association between lumbar lordosis and knee joint dysfunction, particularly noting diminished lordosis in individuals with knee extension limitations exceeding 5 degrees (8). Emphasizing the impact of knee flexion contracture on trunk kinematics during both standing and walking, researchers have underscored the potential role of dynamic changes in trunk motion in influencing spinal alignment. This dynamic interplay may contribute to the development of spinal deformities, a phenomenon recognized as "knee-spine syndrome" (12). While prior studies have delved into knee flexion contracture, either in outpatient settings or simulated conditions, there remains a scarcity of research investigating the intricate relationship between knee and spine alignment. Furthermore, several researchers have identified a robust correlation between lumbar lordosis and the orientation of the pelvis and thorax. Notably, greater lordosis angles are associated with a more horizontally inclined sacrum, heightened pelvic incidence, and an increased pelvic tilt (13, 14). This intricate connection underscores the complexity of lumbar lordosis regulation, highlighting how variations in pelvic and thoracic orientation are intertwined with lumbar curvature.
Given this background, the current study aims to investigate the relationship between patellar alignment and lumbar lordosis curvature in patients with chronic patellofemoral pain syndrome. By exploring this connection, we hope to contribute valuable insights into the complex interplay between knee and spine conditions, shedding light on potential factors influencing PFPS and its management. Understanding the intricate relationship between patellar alignment and lumbar lordosis is crucial for comprehending the complexities of chronic patellofemoral pain syndrome. This research may pave the way for more effective diagnostic and therapeutic approaches in managing this prevalent and challenging condition.
Methodology
Study design and settings
The study was conducted as cross-sectional research. The entire research spanned from March, 2023 to August, 2023 and was conducted at Mnsoura, Dakahleya,Egypt. The target population of the study was patients with chronic patellofemoral pain with a positive McConnell test, between the ages of 20 – 45 years. Patients with osteoarthritis of the knee, ligaments and or meniscal injuries, fracture of the patella or around the knee, and previous spinal surgery such as spinal fracture and scoliosis were excluded from the study.
Data Collection
The data was collected through radiological exams of knee and lumbar lordosis. Anger X-ray machine made in India (fixed x-ray system) (RAD/fluoro) mars 15-80Kw (250-1000 mA) was used in the current study for each radiological exam. Three parameters were recorded: Patella femoral index, lateral patellofemoral angle, and Cobb angle. X-ray for the knee was taken in axial (skyline) projection from supine with knee flexion of 30 degrees (Figure 1).

Figure 1: X ray for the knee
On the X-ray film, the radiologist took 3 measurements for the patella with the trochlear groove: medial joint space and lateral joint space to calculate the patella femoral index and lateral patella femoral angle. The patella-femoral index is the ratio between the medial and lateral patellofemoral joint spaces (Figure 2).

Figure 2: Patella femoral index
The lateral patellofemoral angle is formed by a line drawn along the lateral facet of the patella and a line connecting the anterior margins of the medial and lateral femoral condyles (Figure 3). X-rays of the lumbar curve were also taken. Each patient underwent a lumbosacral examination at lateral projection from a side-lying position for measuring the Cobb method for lumbar lordosis (Figure 4). Lumbar lordosis angle (LLA) was measured using the Cobb method, tangent lines are drawn along the superior end plate of L1 to the inferior surface of L5. Perpendicular to each line is added to form the angle (Figure 5).

Figure 3: The lateral patellofemoral angle

Figure 4: X ray for the lumbar

Figure 5: lumbar lordosis angle
Statistical Analysis
The statistical analysis was performed using the SPSS Package program version 25 for Windows, developed by SPSS, Inc. in Chicago, IL. Descriptive statistics, such as mean and standard deviation, were employed for quantitative data related to demographic information. Pearson correlation (bi-variate correlation) was utilized to assess the relationship between the Cobb angle and the PatellaFemoral Index. Similarly, the Pearson correlation was employed to examine the association between the Cobb angle and the lateral patellofemoral angle in patients experiencing chronic patellofemoral pain. All statistical analyses were considered significant at a probability level of P ≤ 0.05.
Ethical consideration
The study was approved by the Delta University of Science and Technology, Gamasa-Egypt approval number: F.P.T 2307019.
Results
Table 1 and Figure 6 represent the demographic data mean values in the study group. The mean values of age, weight, height, and BMI were 26.20 ±6.00year, 81.94 ±4.37kg, 170.26 ±3.08cm, and 28.23 ±1.64kg/m2, respectively. Table 2, Figures 7 and 8 show the Pearson correlation coefficient between Cobb angle with patella femoral index and lateral patellofemoral angle. There was no significant correlation (r = 0.02; P= 0.922; P>0.05) between Cobb angle and patella femoral index (Figure 2). While there was a significant positive correlation (r = 0.64; P= 0.002; P<0.05) between cobb angle and lateral patellofemoral angle.
|
Table 1: Demographic data in the study group. |
|
|
Variables |
Mean ± standard deviation (SD) |
|
Age (year) |
26.20 ± 6.00 |
|
Weight (kg) |
81.94 ± 4.37 |
|
Height (cm) |
170.26 ± 3.08 |
|
BMI (kg/m2) |
28.23 ± 1.64 |
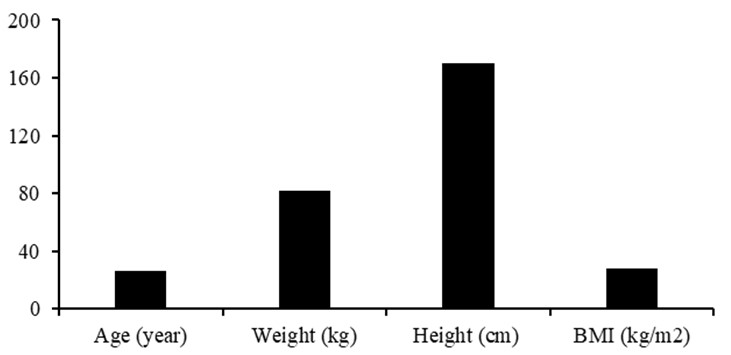
Figure 6: Mean values of demographic data in the study group
|
Table 2: Pearson correlation between cobb angle with patella femoral index and lateral patellofemoral angle |
|||
|
Relations |
Correlation coefficient (r) |
P-value |
Significance (P<0.05) |
|
Cobb angle and patella femoral index |
0.02 |
0.922 |
NS |
|
Cobb and lateral patellofemoral angle |
0.64 |
0.002* |
S |
* p-value < 0.05 is statistically significant, S: Significant, NS: Non-sginficant

Figure 7: Relation between cobb angle and patella femoral index
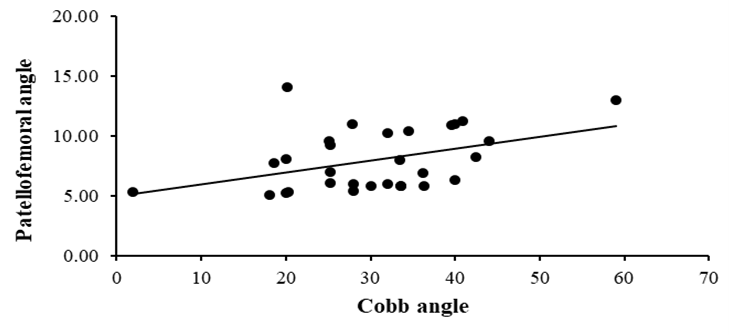
Figure 8: Relation between cobb angle and lateral patellofemoral angle
Discussion
This study represents the inaugural population-based exploration into the correlation between patellofemoral alignment and the lumbar lordosis curve among individuals experiencing chronic anterior knee pain. Our discussion endeavors to establish connections between the patellofemoral joint, knee, hip, sacroiliac joint, and lumbar spine, aiming to elucidate and substantiate the observed relationship.
Patients experiencing chronic anterior knee pain exhibited a lateral displacement of the patella, a finding consistent with previous studies (15, 16).This displacement consequently altered the alignment of the patella to the femoral trochlea. However, these observations contrast with other studies that reported no significant differences in radiographic measurements of patellar alignment concerning patellofemoral pain syndrome (17, 18).
Studies have indicated that individuals with patellofemoral pain syndrome experience alterations in the lower extremity kinematics (19, 20). There is a mechanical connection between the knee and hip regions, suggesting that during activities like squatting, the femur undergoes internal rotation (21). Consequently, the patella shifts laterally, reducing the contact area in the patellofemoral joint (19, 22, 23). This lateral movement places increased pressure on the lateral facets of the patella. The recurring abnormal movements and elevated patellofemoral contact pressure can lead to overloading of the patellar structures, potentially resulting in pain (23-26). Additionally, patients with patellofemoral pain syndrome often display increased lateral translation, spin, and a propensity for greater lateral tilt of the patella (15).
According to Fulkerson and Hungerford (1990), the natural valgus alignment of the knee, coupled with the lateral pull of the quadriceps, tends to increase the likelihood of lateral tracking of the patella (27). These factors collectively contribute to a reduction in the lateral patellofemoral angle, as well as the narrowing of both the medial and lateral patellofemoral joint spaces. Consequently, the patellofemoral index, representing the ratio between these two spaces, remains unaltered. The weakness of the quadriceps, particularly the vastus medialis, is noteworthy in individuals with patellofemoral pain syndrome. This weakness is often attributed to neuromuscular inhibition due to knee pain and an imbalance between the vastus medialis and lateralis, both of which contribute to the malalignment of the patella (28-30).
Several studies have explored the relationship between hip muscle strength and patellofemoral pain. These studies consistently indicated a reduction in muscle strength across various hip muscles, although not all findings reached statistical significance (25, 26, 31-33). Specific declines were noted in abduction and external rotation strength. Furthermore, decreases were observed in abduction, external rotation, and extension strength. The findings suggest that individuals with patellofemoral pain syndrome may engage in fewer daily activities to minimize knee discomfort, leading to a deficit in muscle strength in both hips (25, 26, 31-33).
Studies have highlighted that individuals with PFPS often exhibit weaknesses in the gluteus maximus muscle, leading to notable limitations in passive hip extension and potential shortening of hip flexors (34). Furthermore, research suggests that deficiencies in the gluteus medius and minimus, coupled with susceptibility to fatigue, can contribute to PFPS (35-38). Such weaknesses may influence hip movements, gait alterations, and running mechanics (39, 40). Additionally, there's evidence indicating a connection between hip and spinal issues, often referred to as hip-spine syndrome (41). Specifically, variations in lumbar lordosis and sacral inclination have been linked to hip extension degrees. Moreover, impairments in hip mobility across multiple planes can potentially disrupt mechanical loading patterns on adjacent joint segments (21).
Studies have shown that manipulating the sacroiliac joint can result in a notable reduction in quadriceps inhibition and an enhancement in quadriceps strength among individuals with PFPS (42). These outcomes are believed to stem from an indirect connection between the lumbar paraspinal and quadriceps muscles. Such a relationship could be influenced by alterations in sensory information due to the stimulation of sacroiliac joint receptors through manipulation. This stimulation may heighten excitability in the motor neurons of the lower extremities. Essentially, sensory inputs from the lumbar vertebrae, muscles, and joints enter the spinal cord via nerve roots that also contribute to the femoral nerve from the lumbar plexus. Consequently, these sensory inputs might interact with quadriceps motor neurons or other interneurons in the spinal cord responsible for regulating the quadriceps (42, 43). There exists a biomechanical connection, known as a closed kinetic relationship, between knee pain and the lumbar spine. Any dysfunction within this relationship can lead to altered movements and compensatory joint issues (44).
Studies have indicated a correlation between spinal alignment factors, such as lumbar lordosis and sacral inclination, and knee flexion angles, particularly among elderly patients, a phenomenon termed "knee spine syndrome" (45, 46). As knee flexion increases, there's a notable reduction in lumbar lordosis and sacral inclination. This change can elevate tension in thigh muscles while diminishing spinal flexibility (47). Furthermore, research suggests that knee flexion contracture plays a pivotal role in influencing three-dimensional trunk movements during both relaxed standing and level walking. Such alterations in spinal alignment may contribute to the onset of spinal deformities (12).
Conclusion
In conclusion, the study revealed a noteworthy association between patellar alignment deviations and lumbar lordosis curvature in individuals grappling with chronic anterior knee pain. The observed lateral displacement of the patella in these patients contributes to alterations in patellar-femoral joint dynamics, leading to decreased patellofemoral contact area and increased pressure on the lateral facets of the patella. Further research and longitudinal studies are warranted to delve deeper into the causative factors and potential interventions for chronic patellofemoral pain syndrome, to improve diagnostic accuracy and treatment efficacy for individuals grappling with this challenging condition.
Disclosure
Statement
There is no conflict of interest.
Funding
No funding
Ethical consideration
The study was approved by the Delta University of Science and Technology, Gamasa-Egypt approval number: F.P.T 2307019.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection, analysis, and final writing of the manuscript.
