Volume 3, Issue 12
December 2023
An Overview of Gingival Diseases in Childhood
Droub Kushari, Rawan Srbland, Rinad Nawab, Entesar Alharabi, Maram Al Mutairi, Abdullah Koshak, Mohammed Alassaf, Maha Aldahami, Haifa Alahmari, Imtenan Alnasser, Abdulrahman Obaid
DOI: http://dx.doi.org/10.52533/JOHS.2023.31221
Keywords: Gingival diseases, childhood, dental-plaque, periodontium
The restoration of GH post-treatment for gingivitis or periodontitis is critical, and specific diagnostic criteria are outlined for these conditions. Importantly, even patients with a history of well-managed periodontitis remain at risk for recurrence, necessitating vigilant monitoring and management. Gingivitis, commonly observed in children and teenagers, is a reversible inflammatory condition of the gingival tissue (GT) that does not involve clinical attachment loss (CAL). It serves as a precursor to more severe periodontal diseases characterized by the loss of connective tissue attachment and bone. Controlling gingival inflammation is key to preventing periodontitis and its recurrence. The etiology of childhood gingival diseases is multifactorial, with factors like poor oral hygiene, sugary diets, limited dental care access, and systemic conditions such as diabetes and immunodeficiency playing significant roles. Clinicians must effectively manage gingivitis across all age groups, recognizing the broad categories of gingival diseases: dental plaque biofilm-induced gingivitis and non-dental-plaque-induced gingival diseases.
Introduction
Numerous gingival diseases can affect children, potentially progressing to impact their adult periodontium. The consequences of periodontal diseases often originate during childhood. Gingival health (GH) is typically characterized by an inflammatory presence and the host's response in a relatively balanced state (1). Restoration of GH can occur after the treatment of both gingivitis and periodontitis. The diagnostic criteria for identifying GH in a patient who has received treatment for gingivitis are the same as those mentioned earlier. These specific clinical signs also apply to individuals with a diminished periodontium after successful treatment for periodontitis. A patient who currently shows signs of gingival health but has a history of well-managed and stable periodontitis is still at a heightened risk of facing recurrent periodontitis. Hence, it is crucial to closely observe and monitor these patients to ensure the best possible management of their condition.
Gingivitis is a temporary inflammatory condition that impacts the gingival tissue (GT) and does not lead to clinical attachment loss (CAL) (2). Gingivitis is commonly found in children and teenagers and acts as an early stage that precedes more serious periodontal diseases marked by the loss of connective tissue attachment and bone (1, 3). Effective control of gingival inflammation is crucial for preventing periodontitis and its recurrence.
The etiology of gingival diseases in childhood is multifactorial, with numerous factors contributing to their development. Poor oral hygiene practices, dietary choices rich in sugary foods, and inadequate access to dental care are common risk factors associated with gingival diseases in children (4). Additionally, systemic conditions like diabetes and immunodeficiency disorders can increase a child's susceptibility to severe forms of gingival disease.
Clinicians have a crucial role in the management of gingivitis in patients of all age groups, whether or not they have a history of periodontal disease. Gingival diseases can be broadly classified into two categories: dental plaque biofilm-induced gingivitis and non-dental-plaque-induced gingival diseases (5). To provide optimal care, dental professionals must be aware of diagnosing and treating gingival diseases, understand their underlying causes, and recognising the diverse aetiologies that contribute to these conditions. Effective collaboration between dental and medical providers is essential, especially in cases of non-dental-plaque-induced gingival diseases with potential systemic implications.
Review
GH can be diagnosed in a patient with a healthy periodontium using specific criteria, which include: the absence of attachment loss upon probing, no observable radiographic bone loss (RBL), pocket probing depths (PPD) measuring less than three millimeters, and bleeding on probing (BoP) occurring in less than ten percent of cases (Table 1) (5).
|
Table 1. Summary of the diagnostic look-up for gingival health or dental plaque-induced gingivitis in clinical practice (5) |
||||
|
Category |
Probing Attachment Loss |
Probing Pocket Depths |
Bleeding on Probing |
Radiological Bone Loss |
|
Intact Periodontium (Healthy Gums) |
No |
≤ 3 mm |
No |
< 10% |
|
Health |
Yes |
≤ 3 mm |
< 10% |
Possible |
|
Gingivitis (No history of periodontitis) |
No |
≤ 3 mm |
≥ 10% |
No |
|
Gingivitis (No history of periodontitis) |
Yes |
≤ 3 mm |
≥ 10% |
Possible |
|
Gingivitis in a patient with a history of periodontitis |
Yes ≤ 4 mm (no site ≥ 4 mm with BoP) |
< 10% |
Yes (≤ 3 mm) |
≥ 10% |
Significant disparities exist in periodontal structures between childhood and adulthood (6). The width of the attached gingiva varies, with greater width in the incisor region, a reduction over cuspids, and an increase over primary and permanent molars. The attached gingiva width also tends to increase with age.
During the transitional phase of tooth development, there are observable changes in the gingiva that are associated with the eruption of teeth. Before the tooth's crown emerges, GT swells and takes on a slightly pale appearance, conforming to the shape of the underlying crown. As the crown is exposed through the oral mucosa, the gingival margin and a sulcus cause the gingival edge to become swollen, rounded, and slightly reddish during the eruption process. In the mixed dentition phase, particularly in the front upper teeth area, it is considered normal for GT around permanent teeth to appear more prominent. This prominence is due to the gingiva staying attached to the crown, making it look raised compared to the enamel below it (7).
Epidemiology
Several important points should be taken into account. In developed nations, the incidence of gingivitis stands at roughly 73% among children aged 6 to 11, and this occurrence tends to increase as children get older within this age group (8). Notably, there is a marked increase in gingivitis prevalence during puberty, with estimates ranging from 50% to 99% during adolescence (6). Furthermore, it is interesting to observe that gingivitis prevalence is lower among girls compared to boys, which is likely attributed to differences in oral hygiene practices among these groups.
Classification of gingival diseases
Gingival conditions related to dental plaque: Without local contributing factors
Plaque-induced gingivitis is primarily triggered by the formation of dental plaque. Interestingly, in children between 8 and 12 years old, dental plaque tends to accumulate more rapidly than in adults (6). The clinical signs of this condition typically begin at the edges of GT and then slowly spread to affect other parts of the supporting structures around the teeth. Often, there is a bright red surface discoloration that overlays preexisting chronic alterations. In children, gingivitis is more frequently characterized by changes in gingival color and swelling than by bleeding or increased pocket depth (9). Prolonged exposure can also result in plaque-induced gingival enlargement (10). Notably, the oral granulocyte migration rate (OMR) is lower in children compared to adults, with reduced tendencies for gingival bleeding, crevicular fluid production, and leukocyte activity (11).
Gingival conditions related to dental plaque: With local contributing factors
Eruption cyst and hematoma
Erupting teeth often lead to the occurrence of a dentigerous cyst known as an eruption cyst. These cysts are usually translucent, yielding a soft, circumscribed swelling (Figure 1 A) (6). When the cystic cavity contains blood, the swelling appears as a purple or deep-blue, soft, circumscribed swelling, referred to as an eruption hematoma. Although gingivitis is frequently linked to tooth eruption, it is important to note that tooth eruption itself does not cause gingivitis. Instead, it may occur due to a higher likelihood of plaque buildup in regions where primary teeth are falling out and adult teeth are emerging. Maintaining good oral hygiene can be challenging or uncomfortable during this transition (6). The inflammation linked to this condition shows the natural prominence of the gum line, giving the appearance of significant gingival enlargement.
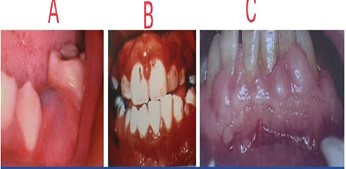
Figure 1: A) Eruption hematoma, B) Leukemia - associated gingivitis, C) Drug influenced gingival enlargement1 (6).
Gingivitis associated with orthodontic appliances
The use of fixed orthodontic appliances makes it considerably more difficult to reach and brush the spaces between teeth. Tipping movements can shift supragingival plaque deposits into subgingival locations, leading to gingival changes that can manifest within one or two months of appliance placement. However, these alterations are typically temporary (12).
Other contributing factors
Gingivitis frequently arises due to a combination of factors, such as an excessive protrusion of upper and lower teeth, blockage of nasal passages, habitual breathing through the mouth, primary teeth that are partially shed or loose, teeth misalignment, worn tooth edges, partially absorbed teeth, and the existence of dental cavities (6).
Gingival diseases modified by systemic factors: Blood dyscrasia-associated conditions
Leukemia
Leukemia is a malignancy characterized by the excessive proliferation of white blood cell-forming tissues, particularly in the bone marrow. Gingivitis can appear in either an acute or chronic form and may affect different types of white blood cells, including granulocytes (myeloid), lymphocytes, or monocytes. Acute forms of leukemia are particularly common among individuals under 20 years old, with acute lymphoblastic leukemia predominantly affecting children under the age of ten. Etiological factors linked to leukemia include radiation and chemical injuries, genetic factors like Down's syndrome, immune deficiencies, and viral infections (Figure 1 B) (6). Clinically, GT presents as swollen, shiny, and spongy with a reddish to deep purple hue, often accompanied by gingival bleeding. Patients may also exhibit symptoms such as fatigue, malaise, sore throat, fever, non-healing skin infections, purpura, cervical lymph node enlargement, spleen and liver enlargement, and petechiae (13).
Gingival diseases modified by systemic factors: Conditions associated with the endocrine system
Puberty gingivitis
During puberty, children often experience heightened levels of gingival inflammation, even when there is not an increase in the accumulation of dental plaque. Gingival cells have specific receptors for sex hormones like estrogen and testosterone. Estrogen receptors can be found in the epithelial layers, fibroblasts, and the endothelial cells of small blood vessels within the connective tissue of the gingiva. This indicates that the gingiva is responsive to specific steroid hormones. The link between increased levels of sex hormones in the bloodstream and the occurrence of gingivitis during puberty is reinforced by the observation that gingivitis typically reaches its highest point at an earlier age in girls (around 11-13 years) compared to boys (around 13-14 years) (14). Moreover, there is a correlation between the levels of P. intermedius bacteria and the concentrations of estrogen and progesterone in the bloodstream. As a result, gingivitis during puberty is marked by significant inflammation, a bluish-red discoloration of the gingiva, swelling, and enlargement of GT. These changes occur due to local irritants that would typically cause a less severe gingival reaction (6).
Gingival diseases modified by systemic factors: Conditions associated with nutritional deficiency
Scorbutic gingivitis
Scorbutic gingivitis is a consequence of vitamin C deficiency, leading to hemorrhaging, collagen deterioration, and edema in the gingival connective tissue. Typically, this condition primarily affects the marginal gingival tissues and papillae (15). The gingiva takes on a bluish color and exhibits a soft, friable texture with a smooth, shiny surface. Hemorrhaging can occur spontaneously or with minimal provocation. Additionally, surface necrosis may develop, accompanied by the formation of pseudomembranes, as a result of capillary infarcts within the gingiva's blood supply (11).
Gingival diseases modified by medication: Drug-induced gingival enlargement
The enlargement of the gingiva is a well-recognized adverse effect associated with certain medications. Among the drugs most commonly implicated in this condition are phenytoin, cyclosporine, and nifedipine (16). Initially, the interdental papillae may develop nodular growths before progressively enlarging and expanding upon the labial tissues. This enlargement is most severe and frequent in the anterior region of the mouth. In individuals with a good standard of oral hygiene, the enlarged gingiva appears pink, firm and stippled. When this condition proves resistant to long-term treatment, it may be necessary to involve the patient's physician to consider modifying or changing the anticonvulsant therapy (Figure 1 C) (6).
Non-plaque-induced gingival diseases: Viral diseases
Acute herpetic gingivostomatitis
This condition predominantly impacts infants and children under the age of six, but it can also manifest in adolescents and adults. The causative agent responsible for this condition is the herpes simplex virus (HSV) type 1. It manifests with widespread redness and a shiny
appearance in the gingiva and nearby oral mucosa, often accompanied by varying degrees of swelling, gingival bleeding, and the development of small grey vesicles that eventually rupture into painful ulcers with a red margin and a yellowish or greyish central area. In certain cases, the formation of vesicles may not be visibly evident. Furthermore, recurrences can happen when individuals are exposed to triggers such as sunlight, fever, colds, or the stretching of the lip due to mechanical forces (6).
Gingival lesions linked to chickenpox
The varicella virus predominantly affects individuals below the age of 15, causing small ulcers in the mouth, commonly located on the palate, gums, and buccal mucosa (Figure 2 B) (17, 19).

Figure 2: A) Hereditary gingival fibromatosis, B) Ulcers associated with chicken pox (6).
Gingival lesions associated with mononucleosis
Mononucleosis, caused by the Epstein-Barr virus, primarily affects children and young adults. Oral signs may include gum bleeding, small red spots (petechiae) on the soft palate, sores on the gums and buccal mucosa, and palatal petechiae. These oral symptoms may appear before the systemic symptoms become noticeable (20).
Soft tissue lesions associated with herpangina
Herpangina is typically caused by Coxsackie group A viruses and is frequently observed in young children. Clinically, it manifests as numerous small fluid-filled vesicles that develop into small ulcers with a greyish center and an inflamed border. These ulcers can appear in different areas including the hard and soft palate, the back of the throat, the buccal mucosa, or the tongue. They usually cause mild discomfort and tend to heal within a few days to a week (6).
Soft tissue lesions associated with hand, foot, and mouth disease
This condition primarily affects children aged between six months and five years. It can be caused by coxsackie group A and B viruses. Clinically, it shares similarities with herpangina but can result in eating difficulties due to mouth sores. However, the disease is typically self-limiting and tends to resolve within one or two weeks (6).
Non-plaque-induced gingival diseases: Fungal diseases
Linear gingival erythema
Linear gingival erythema is defined by a two- or three-mm strip of intense redness in GT at the edge, which then extends into the attached GT as either concentrated or scattered redness. It may even reach beyond the boundary between the gums and the oral lining into the mucous membrane covering the tooth sockets. Although this condition can occasionally be confined to one or two teeth, it usually impacts the gingiva more extensively and is classified as a widespread gingival problem (17).
Candidiasis
Candidiasis is a medical condition that develops due to an overgrowth of Candida albicans, frequently occurring in individuals who have taken antibiotics or those with congenital or acquired immunodeficiencies (6).
Non-plaque-induced gingival diseases: Bacterial diseases
Acute Necrotizing Ulcerative Gingivitis (ANUG)
More prevalent in developing countries and frequently seen in children, with a significant occurrence in India among children below ten years of age. Poor oral hygiene is usually associated with these patients (6).
Non-plaque-induced gingival diseases: Traumatic lesions
Several traumatic factors can contribute to changes in the gingiva, including external tissue injuries, bites, abrasion from toothbrushes, unexplained or idiopathic trauma, habits such as nail biting, and the consumption of abrasive foods (6).
Non-plaque-induced gingival diseases: Congenital anomalies
Congenital epulis
Congenital epulis is an infrequent gingival tumor that appears along the alveolar ridge. Typically, it occurs without any associated tooth abnormalities or additional congenital malformations. Clinically, it manifests as a smooth, well-defined reddish mass emerging from the gum pad. In some instances, it can be sizable enough to push up the upper lip, and it generally does not impact teeth that have not yet erupted, which can be visualized through MRI scans.
Congenital gum synechiae
Congenital gum synechiae is defined by natural adhesions that occur between various parts of the oral cavity. This is an uncommon condition that can result in breathing challenges and respiratory issues shortly after a baby is born (18).
Non-plaque-induced gingival diseases: Gingival diseases associated with heredity
Non-inflammatory, benign familial fibrotic enlargements, like hereditary gingival fibromatosis, usually appear as non-bleeding, gradually advancing enlargements of the gingiva. Nevertheless, in some cases, these enlargements may be accompanied by gingival inflammation (Figure 2 A) (6).
Non-plaque-induced gingival diseases: Foreign body reaction
While not common, foreign body reactions can occur, for example, during amalgam tattooing (6).
Non-plaque-induced gingival diseases: Gingival manifestations of immunological conditions
Wegener's granulomatosis
Although it is a systemic disease, wegener's granulomatosis initially manifests with gingival alterations, characterized by erythema and enlargement, and often referred to as strawberry gums.
Kindler's syndrome
Kindler's syndrome is a rare genetic disorder characterized by several distinctive features. These include the presence of skin blisters (bullae) in neonates, poikiloderma (skin changes with areas of pigmentation, atrophy, and telangiectasia), heightened sensitivity to sunlight (photosensitivity), and atrophy of the extremities (acral atrophy). Furthermore, individuals with Kindler's syndrome may display oral lesions that resemble desquamative gingivitis, a condition characterized by inflammation and peeling of GT (6).
Conclusion
There are a wide variety of gingival diseases that affect children and can potentially impact the oral health of adults later in life. Successful management relies heavily on early diagnosis, so routine dental check-ups should include thorough examinations of the gingiva and supporting structures. Furthermore, severe gingival diseases can sometimes serve as an early warning sign of underlying systemic health issues.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
