Volume 3, Issue 12
December 2023
Chronic Obstructive Pulmonary Disease and Telehealth: Remote Monitoring and Patient Outcomes
Marwah Abdullah, Elaf Fardus, Nada Mahdi, Bashayr Alsaeed, Fatimah Alfahid, Hussain Al zamanan, Badriah Mulayhi, Abdulaziz Almuntashiri, Yusra Alarbash, Musab Alsharif, Mohammed Al Hutaylah
DOI: http://dx.doi.org/10.52533/JOHS.2023.31217
Keywords: COPD, telehealth, remote monitoring, chronic obstructive pulmonary disease, telemedicine, patient outcomes
The integration of telehealth interventions into the management of Chronic Obstructive Pulmonary Disease (COPD) represents a transformative approach to improving patient outcomes and reducing the burden on healthcare systems. With the global prevalence of COPD on the rise, innovative care models, including remote monitoring and teleconsultation, have emerged as essential tools in the early detection and management of COPD exacerbations. These interventions not only lead to a significant reduction in exacerbation frequency and severity but also enhance patients' quality of life by empowering them to take an active role in their healthcare. Improved pulmonary function, medication adherence, and cost-effectiveness further underscore the value of telehealth in COPD care. The high levels of patient satisfaction and the potential for reduced mortality rates emphasize the promising future of telehealth in COPD management. As we continue to advance in technology and healthcare delivery, the comprehensive and personalized care offered by telehealth is poised to make a lasting impact on the lives of COPD patients worldwide.
Introduction
Chronic Obstructive Pulmonary Disease (COPD) is a major global health issue that impacts millions of people around the world and places a substantial financial strain on healthcare systems. With more than 250 million individuals worldwide affected by COPD, it has established itself as a prominent contributor to illness and death, becoming one of the most prevalent causes of morbidity in this decade (1). In 2005, COPD caused the deaths of three million individuals, accounting for 5% of all fatalities during that year (2).
The economic consequences of COPD are immense. The National Health Service in the UK dedicates more than £800 million (equivalent to approximately US$1.42 billion) each year to address this condition (3), whereas, in the United States, the economic impact in 2005 reached a staggering US$39 billion (4). The expenses related to COPD exacerbations, which greatly contribute to the utilization of acute care hospital beds, varied between C$646 million and C$736 million in Canada (equivalent to US$622 million to US$708 million) (5). These statistics highlight the significant social and economic expenses associated with COPD, requiring the implementation of creative strategies for its treatment.
Given these difficulties, telehealth has emerged as a promising remedy. Telehealth, which includes a range of technologies and approaches, provides remote monitoring and delivery of care for patients with COPD. Home telehealth is a specialized form of telehealth that focuses on providing patient care in the home setting (6). This approach can be classified into two categories: remote monitoring and telephone support. Remote monitoring facilitates the provision of healthcare services and monitoring from a distance, effectively connecting patients in their residences with healthcare providers, thereby overcoming the geographical barrier. On the other hand, telephone support or teleconsultation refers to the provision of patient or caregiver assistance through telephone communication, without the electronic transfer of patient information.
Emerging evidence suggests that implementing home telehealth programs can effectively reduce hospital admissions and emergency visits, thereby alleviating the economic burden associated with COPD (7). Furthermore, telehealth interventions have demonstrated the ability to enhance the autonomy of patients, especially among the elderly population who are facing significant symptoms (2). Telehealth utilizes technology to enable real-time monitoring, immediate feedback, and access to information and support, thereby facilitating the early identification and management of exacerbations.
This literature review focuses on the intersection of COPD and telehealth, with a specific emphasis on remote monitoring and its implications for patient outcomes. By examining the available evidence, this review aims to provide an overview of the multifaceted relationship between COPD and telehealth.
Methodology
This study is based on a comprehensive literature search conducted on November 30, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed chronic obstructive pulmonary disease and telehealth, with a focus on remote monitoring and patient outcomes. There were no restrictions on date, language, participant age, or type of publication.
Discussion
A successful remote monitoring setup for COPD hinges on a well-structured technical framework. COPD patients routinely employ wearable devices and sensors, such as smart spirometers and pulse oximeters, to collect crucial health data like oxygen saturation levels, respiratory rate, and peak flow (Figure 1) (8). These devices are equipped with Bluetooth or cellular connectivity for secure data transmission.
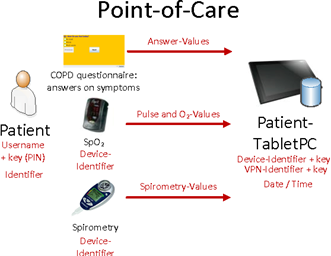
Figure 1: Information Flow in the Point-of-Care (9).
The data is then securely transmitted to a central cloud-based platform accessible by healthcare providers (10). Data is collected at specific intervals, with some patients monitored hourly and others daily. This data is securely transmitted, utilizing encryption protocols, to a cloud server, ensuring patient privacy and data integrity. Once data reaches the cloud server, it is integrated into electronic health records (EHRs) or dedicated monitoring platforms (Figure 2). This consolidated data provides healthcare providers with a comprehensive view of a patient's health over time. Advanced analytics and machine learning algorithms scrutinize this data, uncovering patterns, trends, and irregularities (11). These insights empower healthcare teams to make well-informed decisions about a patient's care plan. Remote monitoring systems are customizable, allowing healthcare providers to set specific thresholds for vital signs and symptoms. For instance, they can establish a threshold for oxygen saturation below which alert triggers. COPD exacerbations can occur suddenly and worsen rapidly (12). Remote monitoring helps in the early detection of exacerbations by identifying subtle changes in vital signs or symptoms.
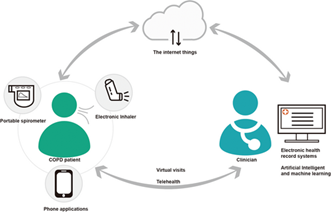
Figure 2: Integrated digital health in a possible future COPD clinic (13).
Healthcare providers can intervene promptly, potentially preventing hospitalizations. When a patient's data crosses these thresholds, the system promptly generates real-time alerts (14). These alerts are transmitted to the patient's healthcare team, signaling them to review the data and take immediate action—an essential element for early intervention in COPD exacerbations. Further, by closely monitoring COPD patients remotely, healthcare providers can identify signs of deterioration before they become severe. This proactive approach can lead to fewer hospital readmissions, as exacerbations are addressed early in the home setting (15). Remote monitoring seamlessly integrates with teleconsultation platforms. Alerts or concerning data points automatically initiate virtual teleconsultations between patients and their healthcare providers. Video calls facilitate visual assessment, symptom discussion, and treatment plan adjustments (16). This real-time interaction enhances patient-provider communication and coordinated care. When concerning data points are detected, patients can have virtual consultations with their healthcare providers, ensuring timely medical advice. As an integral component of COPD remote monitoring, it relies on a robust telecommunication infrastructure, demanding high-speed internet access and stable connections to ensure uninterrupted video conferencing. User-friendly interfaces facilitate navigation for both patients and healthcare providers, allowing for easy initiation of consultations and access to virtual waiting rooms where patients can prepare for their appointments. The adaptability of teleconsultation technology across various devices, including smartphones, tablets, laptops, and desktop computers, enhances accessibility for COPD patients. Security measures, such as encryption and compliance with healthcare privacy regulations, safeguard patient data during virtual consultations.
Further, telehealth facilitates seamless care coordination among various members of the healthcare team. Specialists, primary care physicians, respiratory therapists, and nurses can collaborate through virtual meetings. Many remote monitoring systems incorporate patient-facing mobile apps or web portals. These user-friendly interfaces allow patients to access their health data, track their progress, and access educational materials related to COPD management (17). Patients can input symptoms or subjective data, offering a more holistic view of their health. Through secure video conferencing, patients and providers can engage in face-to-face consultations without the need for physical presence. This virtual interaction allows for visual assessment and personalized care planning. Teleconsultations provide an opportunity for healthcare providers to assess patients' current symptoms and overall well-being remotely. Patients can describe their symptoms, such as increased dyspnea (shortness of breath), changes in sputum production, or cough severity (16). Providers can ask questions to gather detailed information about symptom progression and severity. Patient and provider portals within teleconsultation systems offer comprehensive data management and record-keeping capabilities, ensuring that patients can access their medical records, test results, and appointment history while providers can efficiently update patient information and document consultations. Integration with EHRs ensures that teleconsultation data becomes an integral part of patients' comprehensive health records. Robust technical support is essential, providing assistance with troubleshooting, device setup, and connectivity issues to prevent technical barriers from obstructing teleconsultations. Cross-platform compatibility guarantees that patients and providers can connect effortlessly regardless of their preferred operating systems.
Additionally, accessibility features, such as closed captioning and language translation services, cater to diverse patient needs, including individuals with disabilities. Some remote monitoring systems can track medication adherence (18). Patients are reminded to take their prescribed medications at the correct times, and their adherence is recorded. This helps healthcare providers assess the effectiveness of treatment plans. Remote monitoring prioritizes data security and compliance with healthcare regulations. Adherence to strict data protection standards, such as the Health Insurance Portability and Accountability Act (HIPAA) in the United States, is crucial (19). Patient consent and robust data encryption are central to preserving patient privacy and complying with legal requirements. Patients often appreciate the peace of mind that comes with remote monitoring. Knowing that their healthcare team is monitoring their condition provides reassurance and reduces anxiety, leading to an improved quality of life. Moreover, remote monitoring empowers COPD patients to take an active role in managing their condition. They become more engaged in their healthcare by regularly tracking their vital signs and symptoms. This involvement can lead to better self-management and adherence to treatment plans. Further, timely interventions and fewer exacerbations can result in cost savings for both patients and healthcare systems. Remote monitoring helps reduce the financial burden associated with frequent hospital visits (15). In sum, these technical components collectively contribute to the effective delivery of care in a remote setting, ensuring that COPD patients receive the necessary support and monitoring through teleconsultation.
Telehealth interventions have become an increasingly significant aspect of COPD management, driven by advancements in technology and a growing need for accessible and efficient healthcare delivery. Scientific evaluations of these interventions have shed light on several crucial patient outcomes in the context of COPD and telehealth. One of the most prominent impacts of telehealth in COPD care is the substantial reduction in exacerbation frequency and severity (20). COPD exacerbations often lead to hospitalizations, posing a significant burden on healthcare systems and patients alike. Studies have consistently shown that telehealth interventions can effectively detect early signs of exacerbations through remote monitoring of symptoms, vital signs, and pulmonary function. This timely detection allows for prompt intervention, often resulting in the mitigation of exacerbations and a decreased need for hospital admissions. This not only enhances patients' quality of life but also alleviates the strain on healthcare resources.
Quality of life is a critical aspect of COPD management, as the disease can significantly impact a patient's daily functioning and overall well-being (21). Scientific assessments using tools like the St. George's Respiratory Questionnaire (SGRQ) have revealed that telehealth interventions lead to improvements in various domains of patients' lives (22). These improvements encompass symptom management, physical activity, and emotional well-being. Patients who participate in telehealth programs report a heightened sense of control over their condition, reduced anxiety related to exacerbations, and enhanced confidence in their ability to manage their COPD effectively.
Pulmonary function parameters, including forced expiratory volume in one second (FEV1) and arterial oxygen saturation (SaO2), have also displayed positive changes due to remote monitoring (23). Telehealth platforms equipped with spirometers and pulse oximeters enable regular assessments of these crucial parameters. The data collected allows healthcare providers to make informed decisions regarding treatment adjustments, ensuring that patients receive optimal care tailored to their specific needs. Improved pulmonary function directly contributes to enhanced exercise tolerance and reduced breathlessness, further boosting patients' overall quality of life.
Medication adherence is a cornerstone of COPD management, as consistent use of prescribed medications can prevent exacerbations and slow disease progression (18). Telehealth interventions have played a pivotal role in improving medication adherence rates among COPD patients. Through reminders, education, and real-time feedback, telehealth platforms encourage patients to adhere to their treatment plans diligently. This not only leads to better symptom control but also reduces the risk of exacerbations, hospitalizations, and disease-related complications (24).
Healthcare utilization and cost-effectiveness are essential considerations in the evaluation of COPD telehealth programs (25). Scientific assessments have shown that telehealth interventions optimize healthcare resource allocation by minimizing unnecessary clinic visits and hospital admissions. Remote monitoring allows for the early detection of potential issues, enabling healthcare providers to intervene promptly when necessary. This proactive approach not only enhances patient outcomes but also reduces healthcare costs associated with emergency care and hospitalizations.
Patient satisfaction with telehealth interventions is a key indicator of their success. High levels of patient satisfaction have been consistently reported in scientific studies (2). Patients appreciate the convenience and accessibility of remote consultations, which reduce the need for travel and waiting times. Moreover, the continuous support and education provided through telehealth platforms empower patients to actively engage in their care, fostering a sense of partnership with their healthcare providers.
While not all studies report significant impacts on mortality rates, some evidence suggests that telehealth may contribute to reduced mortality among COPD patients, especially when combined with other improvements in disease management (26). This aspect underscores the potential life-saving benefits of telehealth interventions in the context of COPD.
Although telehealth shows potential in managing COPD, additional research is necessary to fully comprehend its effects on healthcare utilization, cost-effectiveness, and clinical outcomes. Telehealth is a crucial tool in combating the debilitating disease of COPD, as it continues to have a significant impact on both global health systems and individuals. Gaining insight into the perspectives and encounters of users, which encompass individuals with COPD, their caretakers, and healthcare practitioners, is crucial for the seamless incorporation of this into regular healthcare practices.
Conclusion
Telehealth integration in the management of COPD represents a fundamental shift with far-reaching implications. Current literature highlights telehealth's ability to significantly reduce exacerbation rates, enhance patients' overall quality of life, and improve critical markers of pulmonary function and medication adherence. These findings hold the promise of a paradigmatic evolution in the care of COPD patients. Beyond its immediate clinical benefits, telehealth challenges the conventional healthcare framework, offering a blueprint for more personalized, accessible, and cost-effective solutions.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
