Volume 1, Issue 4
July 2021
Awareness Regarding Antibiotic Use Among the Public in Saudi Arabia: A Systematic Review of Cross-Sectional Studies
Marwah Abdullah, Meshary Alshahrani, Nawal Hakami, Ahmed Almalki, Abdulmajeed Hamed, Bayan Betrah, Ahmed Ghazwani, Zain Khayyat, Ameer Saab Qul, Abdulelah Alharbi, Safia Al Abdrabalnabi
DOI: http://dx.doi.org/10.52533/JOHS.2021.1402
Keywords: awareness, knowledge, attitude, antibiotics, systematic review, saudi arabia
Impacting public awareness is an essential part of achieving better use and perception of antibiotics. This systematic review aims to gather the current evidence regarding awareness of the public towards antibiotics use in Saudi Arabia, obtained from cross-sectional investigations. We systematically reviewed cross-sectional studies in Saudi Arabia that include patients from the general population with no background differences in education or occupation. Our final list included 19 cross-sectional investigations that were conducted between 2014 and 2021. All of the studies were prospective surveys and were conducted in different settings, including hospitals or healthcare centers (n= 5), public places (n= 8) and online (n= 6). The sample size was 13,021 participants from different regions across the Kingdom, including various regions, in addition to four nationwide investigations. Most studies reported that the level of knowledge and awareness is insufficient among the included populations regarding the proper use of antibiotics and the awareness of bacterial resistance. Although some studies reported favorable outcomes in their studies, educational campaigns are still encouraged for all the different populations to further enhance the outcomes and increase the levels of knowledge and awareness. Targeting individuals within the demographics that were discussed as significantly correlated with the levels of knowledge and awareness is also advisable. Increasing awareness regarding the use of antibiotics in Saudi Arabia should be further encouraged.
Introduction
Evidence shows that the efficacy of using antimicrobial medications has led to a significant reduction in morbidity and mortality rates from infection-related diseases (1). These drugs are commonly used within the clinical settings of developing countries where infectious diseases are highly prevalent (2). However, many recent reports have indicated that bacterial resistance against many novel antibiotics has increased over the past few years, which poses a significant threat to healthcare systems by increasing the duration of hospital stay, morbidities, and mortalities (1, 3, 4). Projection investigations expect that nearly 10 million cases will experience the consequences of antibiotic resistance each year unless worldwide efforts are introduced to overcome the phenomenon (5). The cost utilization of the healthcare systems was also estimated to be $20-35 billion per year within the United States as a result of the increasing antibiotics resistance (6).
Many factors have been proposed to explain the increasing frequency of antibiotic resistance, including behavioral and cultural factors, reduced educational and socio-economic levels, and reduced quality of healthcare service, in addition to other demographics such as employment, residency, age, and income status (7-10). Therefore, it is essential to screen for these factors and assess the knowledge, awareness, and attitudes of the different populations towards the use of antibiotics and the dangers that may result from misuse and resistance. Many worldwide investigations have been published that report on the knowledge of the different populations regarding antibiotics use and resistance and have suggested that areas with low knowledge and reduced awareness levels should have educational campaigns to improve the attitudes of the corresponding populations. Among these investigations, resistance and use of antibiotics in some diseases such as infective endocarditis and urinary tract infections were specified, while in other studies, absolute reporting of the different types of antibiotics was utilized (11-13). Impacting public awareness is an essential part to achieve a better result of the overuse of non-prescribed antibiotics among them (14).
In Saudi Arabia, many investigations have been published that assess the level of knowledge and awareness among the different populations within different regions (15-22). The levels of knowledge and awareness among these populations are variable, which makes the current evidence about the prevalence of awareness vague and hard to comprehend. Accordingly, the present systematic review aims to gather the current evidence regarding awareness of the public towards antibiotics use in Saudi Arabia that is obtained from cross-sectional investigations.
Methods
Criteria for inclusion and exclusion
The primary outcome of the present study was to assess the level of knowledge and awareness of the Saudi population towards antibiotics use and administration. Accordingly, we formulated our inclusion criteria as follows: 1) studies that were original cross-sectional investigations, 2) studies that investigated the awareness, knowledge, and attitude towards antibiotics use, 3) studies that were conducted in the Kingdom of Saudi Arabia, 4) studies that included Saudi participants mainly from the general population and were not based on foreigners, 5) studies where the population of the study was not confined to a certain disease, 6) human investigations and 7) studies with no language limitations. On the other hand, we excluded studies if: 1) they were non-original, not cross-sectional, or editorial, review, thesis, abstract-only articles, commentaries, or any other study design, 2) they did not report any outcome regarding the level of awareness, knowledge or attitude towards antibiotics use, 3) they were not conducted in Saudi Arabia, 4) the main bulk of the population was not Saudi individuals, such as pilgrims, 5) the population of the study was confined to a certain disease, such as dental patients, infective endocarditis, upper respiratory tract infections, or others, 6) studies that were published before 2010, 7) studies that did not specify the awareness levels for antibiotics only, or used vague terms such as drugs or antimicrobials, and 8) studies that confined their outcomes and populations to a certain group only for assessment of awareness. Accordingly, we identified the general population, which we aimed to include exclusively, as a non-defined sample by the study authors based on the included participants’ positions or educational backgrounds. For instance, assessment of certain groups such as physicians’, students’, teachers’ or even individuals of the general population’s awareness of guidelines of prescription of antibiotics, assessment of knowledge and awareness about resistance or use only, or the effect of a certain educational campaign about awareness, were considered irrelevant to our study outcomes. This may have limited our evidence in reporting due to sample limitations and potentially-different baseline demographics by these studies, which might have influenced their outcomes. All steps of the current study were based on the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (23).
Search strategy
We started our search strategy in PubMed using this search term: (Knowledge OR attitude OR practice OR aware*) AND (antibiotic OR antibiotics) AND ("Saudi Arabia" OR Saudi), which was then modified to suit the search strategy of other databases such as Web of Science, Google Scholar, Embase, Scopus, Virtual Health Library, and Cochrane Library. A manual search of the references of the final list of articles and within the relevant reviews was also conducted to ensure no potentially relevant articles were missed that could help us with our study and formulating solid evidence (24, 25). All of these steps were repeated more than once by the study members to maintain transparency of selection and prevent any potential bias in selection. All search results were exported into one endnote library to detect and exclude the duplicates across the various databases, and the results were then exported into a unified excel sheet for the next step.
Screening and data extraction
This step was also systematically approached to prevent any potential bias in the process of study selection, and so as to not miss any relevant articles, based on our inclusion and exclusion criteria. At least two reviewers and a senior member were involved in this process and all results were blinded until a final discussion between all was conducted to finally agree to all the decisions and justify the excluded citations. Both titles/abstract and full-text screening were undertaken in this study, and were then followed by data extraction. The latter was done in a unified excel sheet that contains all the included articles for easy interpretation of the final results. The sheet mainly consisted of three tabs, including the baseline characteristics, the outcomes, and the quality assessment tabs. Based on these tabs, data was then processed, presented, and interpreted as discussed within the following sections.
Quality assessment tool
The third part of the Excel sheet was filled using the domains of the modified Newcastle-Ottawa scale (mNOS) for cross-sectional studies (26) to assess the risk of bias for the included studies. Studies were classified into good, excellent, satisfactory, or non-satisfactory, based on the cumulative scores that they were given by our reviewers according to the degree of bias among them. The results are presented and interpreted in a following section.
Results
Search results
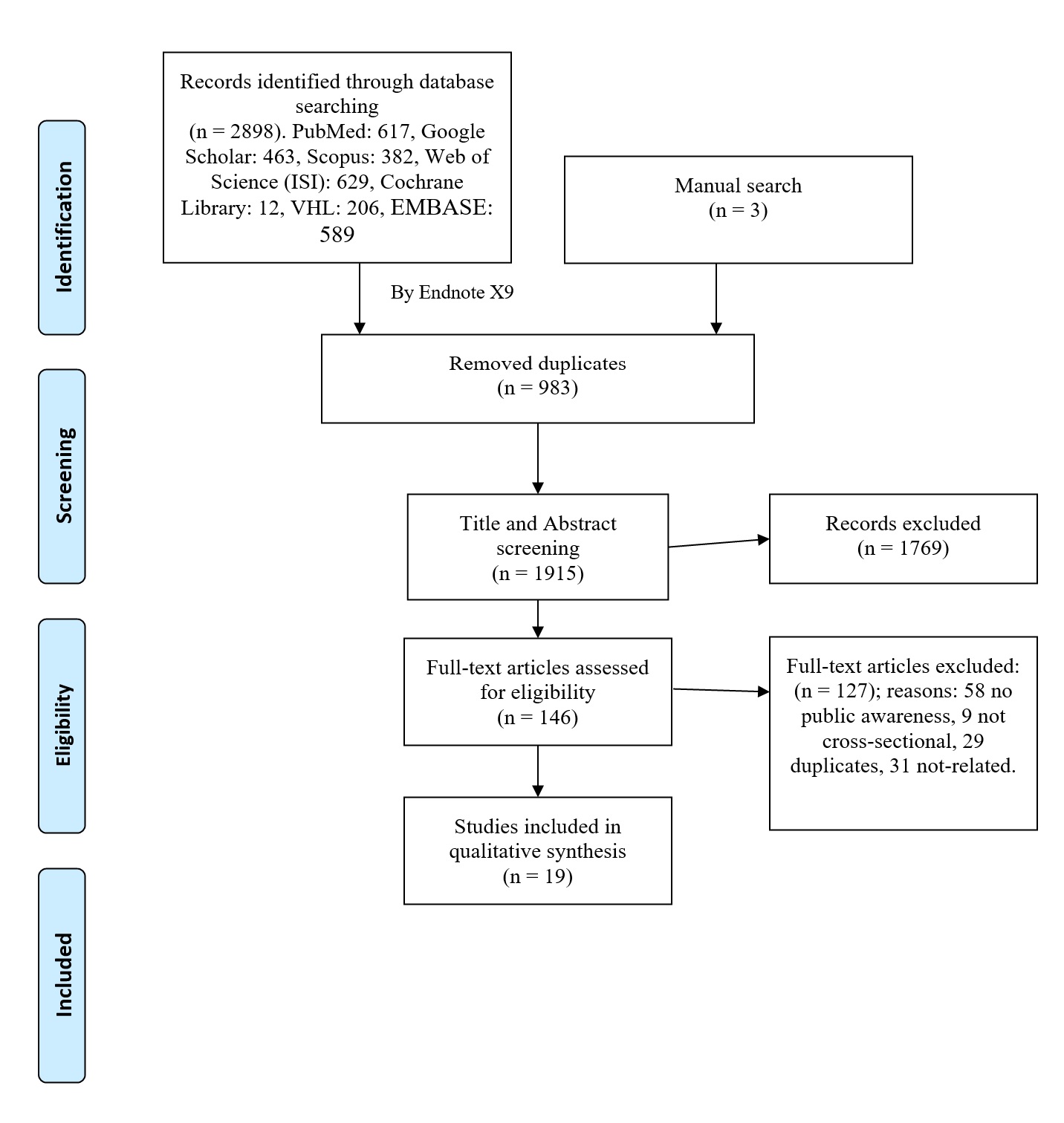
A summary of the search screening methodology and search results passed by the screening steps are presented in Figure 1. Among the screened databases, a total of 2,898 relevant citations were identified, all of which were exported into one endnote library sheet to exclude all the potential duplicates across the different searched databases. In the end, we managed to find a total of 16 articles through these databases, and by manual searching of the references of these cross-sectional studies and the previous systematic reviews, we were able to add another 3 articles to the final list of our included articles, based on our inclusion and exclusion criteria that were previously detailed in another section of the manuscript. The baseline characteristics and the findings of these studies are fully discussed in another section of this report.
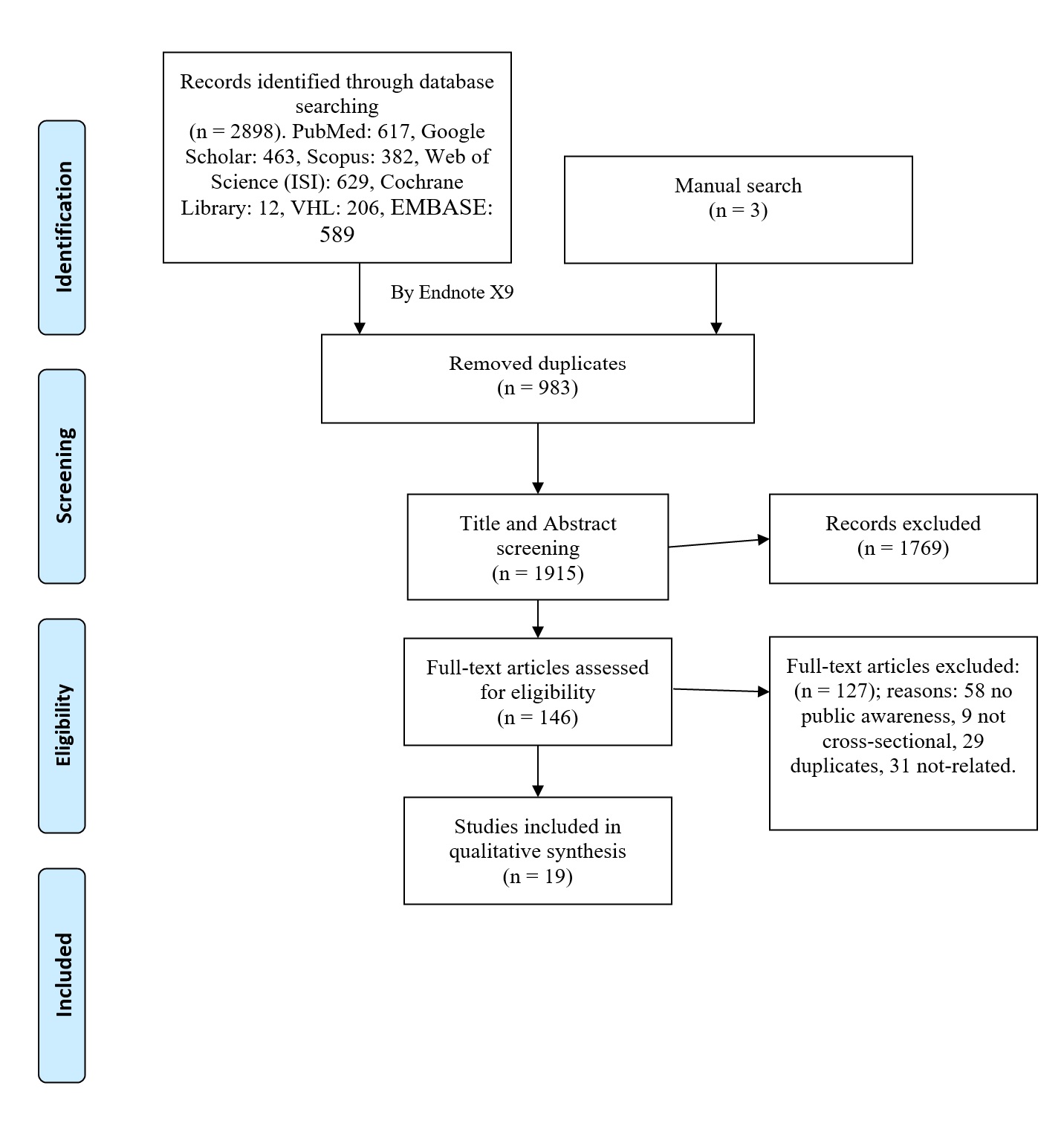
Figure 1. PRISMA flow diagram for study selection and search strategy.
Results of quality assessment
The results of the quality assessment and risk of bias details are fully presented in Table 1, together with the different domains of the used mNOS tool. Briefly, six studies were marked as good quality (indicating the low risk of bias), while the majority of studies (n= 11) were of satisfactory quality (indicating acceptable risk of bias), and the rest (n= 2) had a high degree of bias.
Table 1. Quality assessment and domains of the modified Newcastle-Ottawa scale (mNOS) for cross-sectional studies.
|
Author |
Year |
Selection |
Comparability |
Outcome |
Total score |
Quality |
||||
|
Representativeness of the Sample |
Sample size |
Non Respondents |
Ascertainment of the Exposure |
The Subjects in Different Outcome Groups are Comparable |
Assessment of outcome |
Statistical analysis |
||||
|
Abdelrahman et al.(27) |
2017 |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
7 |
Good |
|
Ajwah et al. (28) |
2014 |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
7 |
Good |
|
Saleh et al. (29) |
2021 |
+ |
+ |
+ |
+ |
+ |
+ |
6 |
Satisfactory |
|
|
Alanazi et al.(30) |
2021 |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
7 |
Good |
|
Al-Ayed(15) |
2019 |
+ |
+ |
+ |
+ |
+ |
5 |
Satisfactory |
||
|
Aldhafar et al.(16) |
2017 |
+ |
+ |
+ |
+ |
+ |
+ |
6 |
Satisfactory |
|
|
Alenazi et al.(17) |
2020 |
+ |
+ |
+ |
+ |
+ |
5 |
Satisfactory |
||
|
Alfalah et al.(31) |
2020 |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
7 |
Good |
|
Alotaibi et al.(18) |
2019 |
+ |
+ |
+ |
+ |
+ |
+ |
+ |
7 |
Good |
|
Alqarni et al.(19) |
2018 |
+ |
+ |
+ |
+ |
++ |
+ |
+ |
8 |
Good |
|
Alsaleh et al.(32) |
2019 |
+ |
+ |
+ |
+ |
4 |
Non-satisfactory |
|||
|
Al-Shibani et al. (20) |
2017 |
+ |
+ |
+ |
+ |
+ |
+ |
6 |
Satisfactory |
|
|
Awadh et al.(21) |
2017 |
+ |
+ |
+ |
+ |
+ |
+ |
6 |
Satisfactory |
|
|
Aziz et al.(33) |
2018 |
+ |
+ |
+ |
+ |
+ |
+ |
6 |
Satisfactory |
|
|
Bahlas et al.(22) |
2016 |
+ |
+ |
+ |
+ |
+ |
5 |
Satisfactory |
||
|
Benmerzouga et al.(34) |
2019 |
+ |
+ |
+ |
+ |
+ |
+ |
6 |
Satisfactory |
|
|
El Zowalaty et al. (35) |
2016 |
+ |
+ |
+ |
+ |
+ |
+ |
5 |
Satisfactory |
|
|
Emeka et al.(36) |
2014 |
+ |
+ |
+ |
+ |
+ |
5 |
Satisfactory |
||
|
Zaidi et al. (37) |
2021 |
+ |
+ |
+ |
+ |
4 |
Non-satisfactory |
|||
Summarizing the baseline characteristics
Our final list included 19 cross-sectional investigations that were conducted between 2014 and 2021. All of the studies were prospective surveys and were conducted in different settings, including hospitals or healthcare centers (n= 5), public places (n= 8), or online (n= 6). The sample size was 13,021 participants from different regions across the Kingdom, including 4 nationwide investigations and additional various regions . Detailed information about these characteristics, in addition to some of the reported findings, are presented in Table 2.
Table 2. Baseline characteristics and authors’ conclusions for the included investigations
| Reference |
Year |
Setting |
Region |
Sample size |
Male (n) |
Mean age |
Targeted populations |
Conclusion |
|
Alqarni et al. (19) |
2018 |
Public places |
Alkharj |
387 |
68.20% |
18->50 |
General population |
Good knowledge scores, 46.8% thought that antibiotics can be effective against viral infections, Good attitude scores. Associated factors included Employment, marriage, being a healthcare worker, educational level, and monthly incomes |
|
Al-Shibani et al. (20) |
2017 |
Hospital |
Riyadh |
1966 |
885 |
18->65 |
Adult general population |
Inadequate knowledge scores, 64.9% were not aware of the adverse events, poor attitude, 42% stopped antibiotics on symptoms relief. Associated factors included the reason, source, and discontinuing the use of antibiotics |
|
Benmerzouga et al. (34) |
2019 |
Public places |
Hail |
500 |
215 |
- |
General population |
Poor knowledge, 26% administered non-prescribed antibiotics, 46.6% were aware of antibiotic resistance, poor attitude, 66% did not complete the antibiotic course. |
|
Al-Ayed (15) |
2019 |
Online forms |
Nationwide |
544 |
75% |
49.9 |
Parents of children |
Poor awareness, 68.6% used antibiotics without a prescription, poor attitude, only 1.3% followed the instructions of using antibiotics. Associated factors included all demographics, but not residency and gender |
|
Emeka et al.(36) |
2014 |
Public places |
Al Ahsa |
489 |
364 |
18-59 |
General population |
Poor awareness, 43.6% are not aware of the adverse events, poor attitude, 19.4% used non-prescribed antibiotics. |
|
Alsaleh et al.(32) |
2019 |
Hospital |
Nationwide |
253 |
0 |
15-50 |
Pregnant general population |
Good knowledge, 85.4% were aware that antibiotics should not be used without a prescription, Good attitude scores. Associated factors included educational and economic levels. |
|
El Zowalaty et al. (35) |
2016 |
Public places |
Nationwide |
1149 |
41% |
26.8 (8.8) |
General population |
Low awareness levels, poor attitudes; 63.6% used non-prescribed antibiotics, 71.1% did not finish the course of the antibiotic. Associated factors included gender, nationality, using leftovers, no medical advice, source of information, and completing the course of the antibiotic |
|
Abdelrahman et al.(27) |
2017 |
Online forms |
Taif |
1028 |
71.50% |
General population |
Moderate knowledge, poor attitude, 23.1% will read and follow the instructions. Associated factors included age, income, education |
|
|
Ajwah et al.(28) |
2014 |
Public places |
Tabuk |
211 |
37.80% |
19-30 |
General population |
Poor awareness and knowledge scores, poor attitude, 61% used antibiotics without prescription, and only 39.2% would complete the antibiotic course. |
|
Zaidi et al. (37) |
2021 |
Public places |
Jeddah |
429 |
298 |
18->60 |
General population |
30.5% had poor levels of knowledge, 54.6% believed that antibiotics can manage viral infections. poor attitude, 51% took non-prescribed antibiotics, 55.1% stopped administration on symptoms relief. Associated factors included education, age, income. |
|
Awadh et al.(21) |
2017 |
Hospital |
Al Madinah |
721 |
55% |
16->50 |
Adult general population |
Around 60% had insufficient knowledge levels. The poor attitude among most participants. Associated factors included age, gender, educational level. |
|
Aldhafar et al.(16) |
2017 |
Public places |
Al Ahsa |
420 |
185 |
31.1 |
General population |
Poor awareness, 61.5% believed that antibiotics were used to treat viral infections. Poor attitude, 28.8% used non-prescribed antibiotics, 28.6% did not continue the course |
|
Alotaibi et al.(18) |
2019 |
Online forms |
Riyadh |
920 |
290 |
18-60 |
General population |
Good awareness levels, most of the population were aware of the adverse events. Poor attitude, 37.4% used non-prescribed antibiotics |
|
Alanazi et al.(30) |
2021 |
Hospital |
Arar |
479 |
170 |
18-65 |
General population |
Good knowledge scores, 56.6% knew about the adverse events, 59.3% knew about antibiotic resistance. Good attitude, only 18.2% used non-prescribed antibiotics. Associated factors include marital status and educational levels. |
|
Saleh et al.(29) |
2021 |
Online forms |
Aseer |
843 |
29.50% |
34.3 (11.3) |
General population |
Good awareness levels, 89% knew about the potential adverse events. Good attitude, 94.4% read the full instructions of using the antibiotics. Associated factors include age, employment, education. |
|
Alenazi et al.(17) |
2020 |
Public places |
Northen border |
1095 |
398 |
16->65 |
General population |
Poor awareness levels, two-thirds knew about resistance, 47% thought that antibiotics can treat influenza. Poor attitude, 42% stopped antibiotics on symptoms relief. |
|
Aziz et al.(33) |
2018 |
Online forms |
Jeddah |
345 |
27.50% |
General population |
Poor awareness, 54.5% knew about resistance, only 38.3% believed antibiotics were used for bacterial infections. Poor attitude, more than half used non-prescribed antibiotics, while 74% reported completing the course of the antibiotic. |
|
|
Bahlas et al.(22) |
2016 |
Hospital |
Jeddah |
479 |
205 |
37.24 (12.17) |
General population |
Poor knowledge, 24.4% knew about indications, 52.8% knew about resistance. Poor attitude. Associated factors include gender, nationality, marital status, monthly income, physicians' advice, proper administration of antibiotics, presence of comorbidities, type of antibiotic |
|
Alfalah et al.(31) |
2020 |
Online forms |
Nationwide |
763 |
39.60% |
- |
General population |
Poor knowledge scores for 48.9% of the study participants. Associaed factors include age, residency. |
n= numbers
Discussion
In the present study, we aimed to discuss the level of knowledge and awareness among the Saudi population, in addition to addressing the attitudes towards the use of antibiotics and the potential associated factors with the levels of awareness and attitudes. In this section of the article, we will discuss the findings from our included studies based on the region within Saudi Arabia.
In Riyadh, Al-Shibani et al. (20) reported that among their adult population, 67% were not aware of the meaning of antibiotic resistance. The same percentage of their population was not also aware of the harmful effects of antibiotics on teeth and around 65% were not aware that antibiotics may be associated with many adverse events such as allergy and death. Moreover, the authors also reported that 31%, 24%, and 21% believed that antibiotics can be used to treated colds, viral infections, and coughs, respectively. A huge percentage also used antibiotics without a prescription and stopped administration when the symptoms were relieved. Knowledge levels differed significantly based on the source of antibiotics, discontinued antibiotics use, and the primary purpose for use. On the other hand, more favorable outcomes were reported by Alotaibi et al. (18), indicating that only 37.4% of their population administered non-prescribed antibiotics, while around two-thirds used antibiotics based on previous experience. In Hail region, Benmerzouga et al. (34) reported that among their 500 participants from the public population, 36.2% were not aware of the meaning of antibiotic resistance, 27% did not identify the etiology for the administration of antibiotics, 26% administered antibiotics without a prescription, and only 34% completed the course of the administered antibiotic. In Arar city, Alanazi et al. (30) reported that their adult population had good knowledge scores, however, only 56.6% of the participants were aware of the severe adverse events that could be associated with the administration of some antibiotics. Around 60% knew about bacterial resistance, and only 18.2% used non-prescribed antibiotics and only 10.9% reported the actual administration of non-prescribed antibiotics. In Aseer region, Saleh et al. (29) reported that most of the study participants believed that antibiotics should not be used without a medical prescription, were aware of the potential adverse events, believed that the full course of the antibiotics should be administered and not only until relief of symptoms, and adequately read and practiced the safe terms of antibiotics use, indicating adequate and acceptable levels of awareness and attittudes in this region.
In Alkharj, an investigation by Alqarni et al. (19) estimated that 46.8% of the study participants believed that antibiotics were effective against viral infections, while 64.3% believed that they were effective against bacterial infections. Being a healthcare worker, employed, married, having a high educational level, and a high income was significantly associated with higher scores. The authors also reported that high awareness scores were significantly associated with high attitude scores. The latter was significantly associated with being a female, healthcare worker, having a higher educational level, and a high income. In Al-Ahsa region, Emeka et al. (36) reported that 13% and 18.8% reported using non-prescribed antibiotics for sore throats and colds, with no evidence of bacterial infection. 4.5% of the population used antibiotics for prevention while 72.8% used them for treatment purposes. They also reported that 43.6% were not aware of the adverse events of antibiotics, and 19.4% administered antibiotics with no prescriptions. Similar findings within the same region were also reported by Aldhafar et al. (16) indicating that 28.8% used nonprescribed antibiotics, 61.5% believed that antibiotic use could treat viral infections, and 28.6% stopped the administration of antibiotics on relief of symptoms. In Al Taif, Abdelrahman et al. (27) reported that approximately 50% of their population were assessed as having moderate knowledge about the use of antibiotics, and the knowledge was significantly affected by the participants’ age, economic status, and educational level. There was a significant correlation between the level of knowledge and the attitude towards antibiotics use and administration. The level of knowledge and awareness was also low in Tabuke as indicated by Ajwah et al. (28) who showed that 61% used non-prescribed antibiotics, and 60.8% finished the course of the administered antibiotics when symptoms were relieved. Furthermore, 20.5% of the study population reported that they changed the regimen by themselves while 79.2% indicated that adherence to the prescribed medical regimen was best for them.
Similar findings were also reported in Jeddah, as Zaidi et al. (37) reported that 30.5% of their study population did not have adequate knowledge about antibiotics use, and approximately half of the population used antibiotics without a medical prescription, thought that they could treat viral infections, or stopped administration when the symptoms were relieved. 49% of the study population believed that antibiotics helped them feel better after the common cold. Educational level and age were significantly associated with the level of knowledge, while monthly income was also significantly associated with the level of knowledge and attitude towards antibiotics use. In the same region, Aziz et al. (33) also reported that more than half of the study participants were aware that excessive and improper administration of antibiotics can lead to the development of bacterial resistance, 12.8% believed that antibiotics can be used to eliminate viral infections, and 23.5% believed that they could eliminate both viral and bacterial infections. Surprisingly, most of the study population was aware that antibiotics should be used until the prescribed course has ended. Bahlas et al. (22) also reported that in Jeddah most of the study participants had inadequate knowledge and attitudes regarding the administration of antibiotics, and both were significantly directly correlated. Marital status, gender, monthly income, number of family members, nationality, the method by which antibiotics were prescribed are all significant factors that are associated with the level of knowledge about antibiotic use in this population. In Al-Madinah, Awadh et al. (21) reported that approximately 60% of their study participants did not have an adequate knowledge about the use of antibiotics, which was associated with a negative attitude among most. The authors reported that around two-thirds of the study participants indicated that they had recently administered antibiotics, and approximately half of them reported using antibiotics five times per year. Age, gender, and educational level were significantly associated with the level of knowledge about the proper use of antibiotics.
A nationwide investigation by Al-Ayed et al. (15) was conducted to assess the awareness of antibiotics use among Saudi children, and included 544 parents. Most of the participants reported that antibiotics were prescribed for their children and around 69% reported that antibiotics administration was done without a prescription. In the same context, only 1.3% of the participants followed the guidelines for antibiotics use. All the demographics of the included parents, except for residency and gender, were found to be significantly associated with the awareness and knowledge regarding the proper use of antibiotics. Similarly, El Zowalaty et al. (35) indicated that approximately 64% of their population used non-prescribed antibiotics, and 71% stopped the administration on relief of symptoms. However, the authors reported that 62% of the participants believed that antibiotics should not be administered without a prescription, which indicates the low levels of awareness among the Saudi population, as suggested by the study authors. A similar investigation by Alfalah et al. (31) also reported that only 10.4% had good knowledge scores regarding the use of antibiotics, and 48.9% had poor knowledge levels. Age and residency were significantly associated with the levels and awareness. On the other hand, Alsaleh et al. (32) reported that their population of pregnant females had good knowledge about antibiotics. They also indicated that the socioeconomic status and the educational level of these participants were significantly associated with the level of knowledge regarding the reason for using antibiotics and whether they were administered with or without prescriptions. Another investigation by Alenazi et al. (17) reported that approximately two-thirds of their study subjects were aware of antibiotics use and resistance. 47% of the study participants used antibiotics for treating the common cold and influenza and 42% discontinued the administration of antibiotics when symptoms were relieved.
Although we have included many studies from different regions across the Kingdom, to generalize our findings, further studies from additional regions are still needed to validate thorough nationwide evidence. The sample size in some of the included studies, in addition to the use of online surveys and cross-sectional designs, may have also limited the transparency of reporting the actual findings across the included populations in our studies.
Conclusion
Most of the included studies reported that the level of knowledge and awareness is insufficient among the included populations regarding the proper use of antibiotics and the awareness of bacterial resistance. Although some studies reported favorable outcomes in their studies, educational campaigns are still encouraged for all the different populations to further enhance the outcomes and increase the levels of knowledge and awareness. Targeting individuals within the demographics that were discussed as significantly correlated with the levels of knowledge and awareness is also advisable.
Declaration
Statement:
The authors declare no conflict of interest.
Funding:
None.
Ethical Consideration:
None applicable.
Data Availability:
All data is available withing the article.