Volume 3, Issue 12
December 2023
Dermatoses of Pregnancy: Overview of Presentation, Treatment and Outcome
Afnan Bokhari, Rania Darwish, Fatimah Bin Dawood, Fatima Mohamed, Omar Alkhaldi, Mazen Alruwaili, Khalid Alhazmi, Taif Tharwat, Fahad Alabbas, Salman Albthali, Ekram Aqel
DOI: http://dx.doi.org/10.52533/JOHS.2023.31205
Keywords: dermatoses of pregnancy, itching, fetal risk, diagnosis, management
Dermatoses of pregnancy encompass a range of skin disorders that manifest uniquely during the gestational period, characterized by significant itching. This review delves into four primary types: polymorphic eruption of pregnancy, pemphigoid gestationis, atopic eruption of pregnancy, and intrahepatic cholestasis of pregnancy. While atopic eruption and polymorphic eruption are generally benign with no fetal impact, pemphigoid gestationis and intrahepatic cholestasis carry risks for the fetus, including prematurity and stillbirth. Key challenges include the difficulty in early diagnosis of pemphigoid gestationis due to its resemblance to polymorphic eruption and the increased risk of complications like gestational diabetes and pre-eclampsia in intrahepatic cholestasis. Understanding these dermatoses is crucial for prompt diagnosis and effective treatment, to prevent adverse outcomes for mothers and babies and improve the overall pregnancy experience. The review focuses on epidemiology, clinical features, diagnostic methods, maternal and fetal outcomes, treatment options, and comprehensive management strategies for these conditions.
Introduction
During pregnancy, alterations occur in the immune, metabolic, endocrine, and vascular systems (1, 2), which can lead to three types of skin changes: physiological skin alterations due to pregnancy, skin conditions and growths that are affected or worsened by pregnancy, and particular skin diseases related to pregnancy (3, 4). These skin changes during pregnancy can significantly affect the patient and their family psychologically.
Physiological change affects various systems of the body, notably the skin, vascular system, glands, connective tissues, hair, and nails. These changes can manifest as increased pigmentation, vascular alterations such as pyogenic granuloma and varicosities, glandular modifications like enhanced sweating and sebum production, and connective tissue adjustments, including the appearance of stretch marks and hirsutism. Hair may undergo a temporary loss phase after childbirth, and nails may become brittle or undergo other structural changes. Although these transformations may cause concern, they are generally temporary and tend to resolve after the baby is born, reflecting the body's remarkable capacity to adapt to the demands of pregnancy (5).
Dermatoses of pregnancy are a diverse group of skin conditions that occur during pregnancy and are often confusingly named. CM Ambros-Rudolph has suggested a new way to classify these diseases (6). The four primary forms are atopic eruption of pregnancy, intrahepatic cholestasis, polymorphic eruption of pregnancy, and pemphigoid gestationis. The most common diseases are atopic and polymorphic eruptions, which do not cause complications for the mother or baby. This group includes a variety of inflammatory skin diseases that occur during pregnancy or the postpartum period. The most common symptom among these conditions is intense itching (7). While pemphigoid gestation can result in underweight newborns, Intrahepatic cholestasis poses a higher risk of fetal distress, premature birth, and stillbirth (8, 9). Understanding the symptoms, progression, and treatment of these skin conditions is crucial for accurate diagnosis and prompt therapy. This knowledge helps prevent negative effects on mothers and babies and, in less severe cases, enhances the overall quality of the pregnancy experience (10). A detailed examination of these aspects is essential for providing comprehensive care to pregnant women experiencing these dermatological challenges. This knowledge not only aids in accurate diagnosis and effective treatment but also helps in counseling patients about the potential implications for their pregnancy and the health of their unborn child (7).
Methodology
This study is based on a comprehensive literature search conducted on November 16, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the dermatoses of pregnancy, particularly presentation, treatment, and outcome. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Pregnancy dermatoses include a group of skin disorders characterized by significant itchiness, unique to the gestational period. These include polymorphic eruption of pregnancy, pemphigoid gestationis, atopic eruption of pregnancy, and intrahepatic cholestasis of pregnancy. While pemphigoid gestationis and intrahepatic cholestasis of pregnancy are linked to fetal risks and unfavourable pregnancy outcomes, atopic eruptions of pregnancy and polymorphic eruptions of pregnancy are often benign and have no effect on fetal health (10). The challenge in early pemphigoid gestationis diagnosis, due to its similarity to polymorphic eruption of pregnancy, underscores the need for careful evaluation to ensure timely and appropriate intervention. Intrahepatic cholestasis of pregnancy not only poses risks to the fetus but also increases the likelihood of other pregnancy complications like gestational diabetes and pre-eclampsia. Therefore, a thorough understanding of these conditions, their manifestations, progression, and treatment is crucial. With this information, medical professionals may improve the entire pregnancy experience for patients with benign dermatoses while also making accurate diagnoses, administering efficient treatment, and ultimately ensuring the health of both mother and child.
Polymorphic eruption of pregnancy (PEP)
PEP is a benign, temporary disease with an unknown aetiology that usually manifests in the latter stages of pregnancy, notably between weeks 36 and 39, and sometimes shortly after deliveries (11). The term PEP is now preferred over previous names like toxemic rash of pregnancy and several others due to its comprehensive coverage of the dermatosis' clinical and morphological features (12-14). It is the most common specific dermatosis of pregnancy, with an incidence rate of 1 in every 200 pregnancies, predominantly affecting women in their first pregnancy with the cause still being unknown (15). The pathophysiology is thought to be related to an inflammation caused by the rapid expansion of the abdomen, which might be linked to factors such as excessive weight gain, twin pregnancies, or a larger than average fetus for the gestational age (4, 6, 16). Clinically, PEP starts with urticarial papules on the abdominal stretch marks, avoiding the area around the navel, an important distinguishing factor from PG (17, 18). These papules can merge into plaques and spread to the limbs, trunk, and buttocks, but do not affect mucous membranes or the face (Figure 1) (5). They might display small blisters, target-like lesions, and polycyclic papules (11, 19). This condition usually lasts 4–6 weeks (4). The diagnosis is clinical, supported by non-specific histopathology and negative immunofluorescence tests (15). Treatment includes psychological support, informative reassurance, and symptom management using comfortable clothing, moisturizers, mild to moderate corticosteroid creams, and topical anti-itch treatments. Severe cases may require low-dose oral corticosteroids. Typically, symptoms regress a few weeks post-delivery, with notable improvement often seen hours after childbirth (15). PEP does not impact the prognosis for mother and child and is not known to recur in subsequent pregnancies (4).

Figure 1: Polymorphic eruption of pregnancy (5).
Pemphigoid gestationis (PG)
PG was initially identified by Bunel in 1811 and later reported by Milton in 1872 as Herpes gestationis (1), a rare autoimmune blistering skin condition resembling bullous pemphigoid (BP). Its occurrence is estimated at 1 in every 50,000 to 60,000 pregnancies, more frequently observed in women with multiple past pregnancies (20, 21). PG is commonly observed in the second and third trimesters (21-28 weeks). It can also sometimes manifest postpartum (17, 18, 21, 22). The condition often recurs in subsequent pregnancies, sometimes earlier and more severely, and can also flare up during menstruation or when using oral contraceptives (15). PG has been linked to trophoblastic tumors such as the hydatidiform mole and choriocarcinoma. Fetal risks include prematurity, low birth weight, and occasionally a bullous eruption due to maternal antibodies, which usually resolve quickly and spontaneously. Clinically, PG begins with erythematous and urticarial papules and plaques, progressing to vesicles and blisters, often accompanied by severe itching (20) (Figure 2) (5). In 90% of cases, lesions first appear around the navel and spread to the abdomen and limbs, with occasional involvement of the oral mucosa (15-20%) (23). PEP and PG must be distinguished from each other, as PEP often skips the periumbilical area and exhibits negative immunofluorescence tests (15). Histopathologically, initial lesions show papillary edema with lymphocyte infiltration and variable eosinophils in the dermis (21, 22). Direct immunofluorescence (DIF) of perilesional skin biopsies often shows linear C3 and IgG deposition along the basement membrane zone (15). Indirect immunofluorescence (IIF) in patient serum is mostly positive, with immunoblotting revealing that 90% of serum from PG patients recognizes collagen XVII. Treatment for mild PG involves low to medium-potency topical corticosteroids and skin care, while severe cases require systemic corticosteroids. Severity is assessed based on the affected body surface area (less than or more than 10%). Postpartum worsening may necessitate increased medication, which should be tapered off two weeks after delivery and gradually withdrawn over 3–6 months depending on lesion severity and progression (21, 23). A multidisciplinary approach is recommended for diagnosing and managing PG (15).

Figure 2: Classically PG presents during late pregnancy (5).
Atopic eruption of pregnancy (AEP)
AEP, a term introduced by Ambros-Rudolph et al. in 2006 (6), encompasses a range of dermatological conditions related to atopic dermatitis that either worsen or first appear during pregnancy. Its pathogenesis remains largely unexplained (3). AEP typically presents earlier in pregnancy, during the first and second trimesters, in contrast to other specific dermatoses of pregnancy (4). However, patients without a history of atopic conditions are more prone to developing AEP later in their pregnancy (24). Ambros-Rudolph et al. have identified two primary clinical forms of AEP: the eczematous type (E-type) and the prurigo type (P-type). The E-type is characterized by eczematous eruptions on the face, neck, pre-sternal area, and flexural regions, while the P-type presents as small, itchy, erythematous papules, often clustered and predominantly located on the extensor surfaces of the limbs and trunk (15). There are ongoing debates regarding the inclusion of pruritic folliculitis of pregnancy (PFP) and prurigo of pregnancy (PP) in the categorization of AEP. Some experts view them as distinct entities (24, 25). PFP was initially identified in 1981 by Zoberman and Farmer (26). Usually manifesting as a monomorphic, erythematous papular eruption in the second and third trimesters of pregnancy, the condition usually goes away after delivery (Figure 3) (5). It is characterized by itchy, erythematous papules and nodules primarily affecting the extensor regions of the limbs and trunk (15). The management of these specific dermatoses of pregnancy, regardless of its specific classification, focuses on symptomatic relief. They generally resolve after childbirth without posing significant risks to maternal-fetal health.
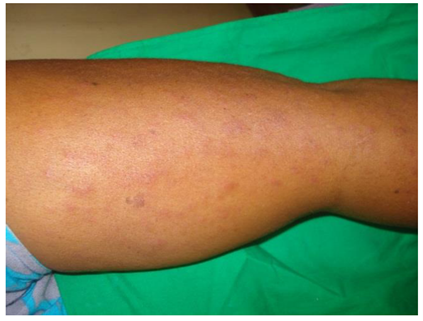
Figure 3: Atopic eruption of pregnancy (5).
Intrahepatic cholestasis of pregnancy (IHCP)
IHCP, first described by Kehrer in 1907 as recurrent jaundice of pregnancy (1), is also known as cholestasis of pregnancy, prurigo gravidarum, and pruritus of pregnancy (15). Unique among specific dermatoses of pregnancy, IHCP initially presents with pruritus without primary cutaneous lesions (Figure 4) (5). Its prevalence varies between 0.3% and 5.6%, influenced by geographic and ethnic factors, with a study in Australia reporting a prevalence of 0.7% (11, 27). Positive family history contributes to almost half of IHCP instances, and twin pregnancies are more common than single pregnancies. Although IHCP usually manifests in the second or third trimester, it can sometimes begin as early as the eighth week of pregnancy. It recurs in around 70% of future pregnancies and conjunction with the use of oral contraceptives (11, 16, 28). IHCP's pathogenesis is complex and not entirely understood. It likely involves genetic, hormonal, immunological, and environmental factors, with the estrogen-bile acid axis playing a significant role. Additional factors might include deregulation of the extracellular matrix and oxygen supply, organelle dysfunction, and epigenetic changes (29). Clinically, IHCP is marked by intense, persistent, and generalized itching, often worsening at night, initially affecting the palms and soles. Scratching can lead to excoriations, erosions, and small papules (11). Jaundice is less common, seen in fewer than 20% of cases, while choluria and acholic stools may occur in half of the cases, typically 2–4 weeks after pruritus onset (15). Diagnostic criteria for IHCP are not universally agreed upon but often include persistent pruritus resolving after childbirth and bile acid concentrations exceeding 10 μmol/L (29). The primary treatment for IHCP is ursodeoxycholic acid (UDCA) at 10–15 mg/kg/day, which helps control itching and reduce bile acid levels (28). While UDCA is also considered for improving fetal outcomes, its efficacy in this regard remains a subject of debate (29, 30). Emollients and topical antipruritics are generally ineffective. In prolonged cholestasis, vitamin K administration may be necessary (15). Pruritus usually resolves within 48 hours after delivery, with laboratory abnormalities normalizing within 2–4 weeks. While the maternal prognosis is often favorable, fetal risks include prematurity, perinatal mortality, and distress. A significant study by Ovadia et al. highlighted that IHCP with total serum bile acids of 100 μmol/L or higher significantly increases stillbirth risk, underscoring the importance of serum bile acid measurement in IHCP diagnosis and monitoring during pregnancy (31). Recent advances in understanding IHCP's pathogenesis may reveal new drug targets. Intensive maternal and fetal monitoring, along with care from an experienced multidisciplinary team, is crucial to determining the safest timing for delivery (15).

Figure 4: Intrahepatic cholestasis of pregnancy (5).
General considerations
In the dermatoses of pregnancy, diagnosis primarily relies on clinical observations. Except for conditions like PG and IHCP, laboratory methods are generally insufficient for distinguishing between different types of SDPs. This underscores the importance of clinical evaluation, with laboratory tests primarily used for differential diagnosis. As such, the symptoms of itching, particularly in the second and third trimesters of pregnancy, should never be overlooked. It is not only impacting the quality of life of the pregnant woman but can also be indicative of various medical conditions. Understanding the etiology and pathophysiology of dermatoses in pregnancy remains a significant area for future research, which may lead to new therapeutic approaches. In the meantime, the management of these conditions benefits greatly from a multidisciplinary approach. This involves obstetricians, dermatologists, and other healthcare professionals working together to diagnose and treat these dermatoses. The primary objective in managing dermatoses of pregnancy is to provide optimal prenatal care that prioritizes the health and well-being of both the mother and the fetus. This involves careful clinical monitoring and a thorough risk-benefit assessment tailored to each case (15). (Table 1) concludes the dermatoses of pregnancy.
|
Table 1. A summary of pregnancy dermatoses (5). |
||||
|
PG |
PEP |
ICP |
AEP |
|
|
Incidence |
1/3000-50000 |
1/250 |
2/1000 |
1/120-240 |
|
Onset |
2nd & 3rd trimester, post-partum |
3rd trimester |
2nd & 3rd trimester |
1st & 2nd trimester |
|
Skin lesions |
Vesicles/bullae |
Red papules/plaques |
Excoriation/papules |
Exc. papules |
|
Pruritus |
Yes |
Yes |
Yes |
Yes |
|
Resolution |
Few weeks to 1 year |
Within 2 weeks |
Few weeks |
Several months |
|
Histology |
Subepidermal blisters |
Epidermal edema |
Non specific |
Perivascular infiltration |
|
Immunofluorescence |
Yes |
No |
No |
No |
|
Management |
Steroids, Antihistamines |
Calamine, Antihistamine |
Ursodeoxy cholic acid |
Aqueous cream |
|
Fetal effect |
Prematurity, Neonatal blisters |
None |
Premature birth, Still birth |
None |
|
Recurrence |
Yes |
No |
Yes |
Yes |
Conclusion
Clinicians should have a comprehensive understanding of the dermatoses of pregnancy. Accurate diagnosis and effective treatment of these conditions are essential to mitigate risks to both mother and child and to enhance the overall quality of the pregnancy experience. A multidisciplinary approach involving obstetricians, dermatologists, and other healthcare professionals is crucial in managing these dermatoses, underscoring the importance of individualized care and risk assessment in prenatal care.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
