Volume 3, Issue 12
December 2023
Indication and Success Rates of Skeletal Anchorage System in Orthodontics
Hussam E. Najjar, Farah Ghander, Abdulelah Al Almuaysh, Sarah Alzaid, Latifah Almasaud, Fatima Alsobhi, Abdullah Alrashidi, Mahi Khalil, Amal Aljefri, Faisal Alshehri, Majed Alsaif
DOI: http://dx.doi.org/10.52533/JOHS.2023.31202
Keywords: skeletal anchorage system, mini-screws, mini plates, implants, success
Skeletal anchorage systems, a pivotal innovation in orthodontics, involve the use of Temporary Anchorage Devices (TADs) or mini-implants, providing stable anchor points in the bone to facilitate precise tooth movements. This comprehensive review article aims to investigate the indications and success rates of skeletal anchorage systems in orthodontics. The research, initiated on November 2nd, 2023, involved an extensive examination of existing literature, utilizing databases like PubMed, Web of Science, and Cochrane. Various components, including mini-screws, mini plates, palatal, buccal shelf implants, and infrazygomatic implants, have enriched orthodontic diversity. Mini screws have displayed remarkable success rates, with most complications related to manageable soft tissue inflammation. Gingival health and smoking habits have been identified as influential factors in mini screw implant success. Mini plates offer sturdy anchorage with resistance to root damage and fracture, surpassing mini screws in overall success rate. Age, implantation site viability, and soft tissue characteristics influence their success. Palatal and buccal shelf implants provide exceptional stability, enhancing the results of fixed bracket appliances. The anterior palatal region is a preferred site for implantation. Infrazygomatic implants, while offering commendable stability, display failure rates within the range of 21-28%, with compromised oral hygiene, immediate loading, inflammation, tooth mobility, and a high mandibular plane angle as potential failure factor. These anchorage methods have expanded treatment possibilities, offering effective solutions for challenging orthodontic cases and ultimately improving patient outcomes.
Introduction
The most ideal strategy for orthodontists to move teeth to create a desirable arch dynamic is to avoid all unnecessary and reciprocal tooth movement (1). Ideal anchorage is one of the most efficient ways to achieve minimal unwanted tooth movement and hence has been a point of attention for many years (1). Anchorage is commonly defined as resistance to unsolicited tooth movement during orthodontic treatment and is usually a point of concern during the treatment of malocclusions (1). Traditional dental anchorage relies on the stability of the patient's existing teeth. In cases where one group of teeth needs to be moved, other teeth serve as anchors to provide stability (2). The most common issue with dental anchorage is the loss of anchorage. This occurs when the teeth that are supposed to serve as anchors for orthodontic forces are inadvertently moved during treatment. Loss of anchorage can lead to undesirable tooth movements, including space reopening or unwanted rotation (2). Additionally, in some cases, there may not be enough stable teeth available to serve as anchors. This can be a problem in patients with missing teeth or those who require extensive tooth movement. Insufficient anchorage can make it challenging to achieve certain orthodontic goals (3). A higher risk of relapse, the need for additional anchorage in complex malocclusions, and interference from dental restorations are some other complexities associated with dental anchorage in orthodontic treatment (2). Another possible anchorage strategy is to use extraoral anchorage, which involves the use of structures or appliances outside the mouth to provide stability for orthodontic forces such as headgear (3). However, patient compliance, especially in children, is a leading cause of extraoral anchorage failure (4). To achieve absolute or infinite anchorage, it is crucial that zero movement of the anchor or anchorage unit be expected and observed (3, 5), and hence, skeletal anchorage is the best alternative.
A skeletal anchorage system is an important innovation in the field of orthodontics. It includes the use of Temporary Anchorage Devices (TADs) or mini-implants, which provide stable and stationary anchor points in the bone to facilitate the movement of teeth or tooth segments (6). Skeletal anchorage is particularly useful in cases where traditional anchorage methods may not be sufficient or may lead to unwanted side effects. Skeletal anchorage systems typically involve the placement of small titanium mini-implants into the bone, usually in the jaw or other suitable locations (7). These mini-implants serve as temporary anchor points for orthodontic forces. The placement of mini-implants is a relatively minor surgical procedure that is minimally invasive and well-tolerated by most patients. Local anesthesia is typically used during the placement process (7). Skeletal anchorage systems are versatile and can be used for various orthodontic movements, such as space closure, intrusion, extrusion, and correction of bite discrepancies (8). They allow for more precise and predictable control of tooth movement. Moreover, these anchorage devices are temporary and are typically removed after they have served their purpose (8), and they can be used in combination with traditional orthodontic appliances such as braces and aligners (3). There are several types of skeletal anchorage systems, or TADs, used in orthodontics, and they can be broadly categorized into two main groups: mini-screws and plates or palatal implants. Mini screws are the most commonly used type of skeletal anchorage device. They are small titanium screws that are typically placed in the bone of the jaw to serve as anchor points for orthodontic forces (9). Mini screws are available in various lengths and diameters to suit different clinical situations. The specific types of minis crews may vary by brand and design, but they all function as temporary anchorage devices (10). In addition to minis crews, there are also skeletal anchorage systems that involve the use of plates or implants placed in the palate (9). These devices can be used for specific orthodontic purposes, such as achieving vertical control over tooth movement or providing anchorage for maxillary expansion (10). Within these two main categories, there may be further variations and designs of skeletal anchorage devices, depending on the specific clinical needs of the patient. Skeletal anchorage systems have a general success rate of approximately 98.6%, with almost 40% of the cases experiencing mild or minimum complications (11). The use of skeletal anchorage systems requires careful planning, precise placement, and ongoing monitoring by a qualified orthodontist or oral surgeon. The choice of the specific device and its placement will depend on the patient's unique orthodontic needs and the goals of the treatment.
The objective of this review article is to comprehensively examine the indications and success rates of skeletal anchorage systems in orthodontics. By analyzing existing literature and clinical studies, this review aims to provide an in-depth understanding of when and how skeletal anchorage systems are employed in orthodontic treatment. Furthermore, it will evaluate the success rates and factors influencing the outcomes of these devices, shedding light on the practical implications and potential limitations of their use in clinical practice. As orthodontics continues to evolve, this review article will contribute valuable insights into the role of skeletal anchorage systems, their impact on treatment outcomes, and the considerations that orthodontists must consider when incorporating these devices into their patient care strategies. Ultimately, the goal is to offer a comprehensive overview that informs both orthodontists and researchers about the best practices, challenges, and prospects associated with the application of skeletal anchorage systems in orthodontic treatment.
Methodology
The research, which commenced on November 2nd, 2023, was initiated following an extensive examination of the existing body of literature. Various databases, including PubMed, Web of Science, and Cochrane, were utilized to conduct this literature review. The search process involved the use of a wide range of combinations of medical terminology. Additionally, manual searches were performed on Google Scholar to identify relevant research terms. The primary objective of this literature review focused on several crucial areas, such as the types of skeletal anchorage systems, their applications, and insertion methods. Furthermore, keywords related to the effectiveness and success of these anchorage systems, as found in the literature, were also incorporated into the search. It's important to mention that the criteria for selecting articles to be included in this study were determined by multiple factors to ensure a comprehensive and robust review process.
Discussion
Skeletal anchorage systems are used in orthodontics for a variety of indications when traditional orthodontic methods may not be sufficient or effective.
Mini screws
They were introduced in 1997 and since then, have been a component of skeletal anchorage systems. These mini screws are usually placed in specific locations in the maxilla and mandible, such as in the palate below the nasal spine, infrazygomatic crest, symphysis or parasymphysis, retromolar area, or maxillary tuberosities (12), as illustrated in Figure 1. The use of local anesthesia for the placement drilling, and insertion of the mini screw is necessary. Mini screws are indicated in those orthodontic cases where skeletal anchorage is required for molar protraction, molar distalization, anterior retraction, molar uprighting, and intrusion and extrusion of the arch (13). The success rate of mini-screws was found to be remarkable in the literature, with only minimal complications arising in the majority of the cases. These complications were mostly related to soft tissue inflammation, which was easily managed by oral hygiene maintenance (11). The overall success rate reported for mini screws in orthodontic procedures was 88.54% (14). Factors associated with the success rate of mini-screws were age, oral hygiene, placement site, and vertical skeletal facial pattern on the cephalography (14). Regarding the ideal length of the mini screw, the highest success rate was found to be associated with mini screw implants with lengths of 10-12mm (15). Moreover, there was no difference in the success rates of self-tapping, and self-drilling mini screws (16). One of the studies dedicated to the failure of mini-screws in orthodontic settings highlighted that none of the mini-screw-related factors was associated with the failure. However, gingival health and smoking habits were the main influences in the failure of mini screw implants (17).
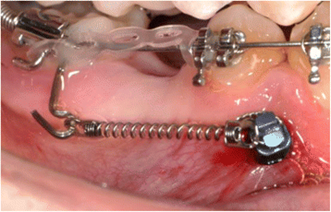
Figure 1: Orthodontic mini screw implant (36)
Mini plates
Mini plates are sturdy and more impervious to root damage and fracture as compared to mini screws. As shown in Figure 2, they are usually divided into three parts: head, arm, and body, and can be placed at a few viable locations within the oral cavity, such as the zygomatic buttress, piriform rim, and lateral cortex in the mandible (18). The insertion process is similar to the mini screws, with the required use of local anesthetic. One of the most significant advantages of mini plates is that these devices can produce desired movements in both the vertical and sagittal planes. In the vertical plane, complete arch intrusion and individual tooth intrusion are possible indications (18, 19). On the other hand, in the sagittal plane mini plates can be used for complete arch distalization, and molar protraction (18, 19). The overall success rate for mini plates in orthodontics was reported to be 96.8%, which was significantly higher than the mini-screws (20). Commonly associated risk factors with the failure of mini plates were age, viability of the implantation site, and soft tissue characteristics (21). Additionally, the instability of the mini-plates used in skeletal anchorage was found to be higher in isolated mini-implants positioned in the mandibular region (22). The development of granulation tissue and a higher rate of inflammation were reported in the mini plate insertion cases; however, the difference was not statistically significant when compared with the mini screw cases (23).

Figure 2: Maxillary and mandibular mini plates (37)
Palatal and buccal shelf implants
To achieve absolute orthodontic anchorage, palatal and buccal shelf implants are used. The palatal implants function by osteointegrating and connecting the transpalatal arch (Figure 3), however, the buccal shelf implants are placed in the buccal alveolar bone of the mandible (24). The stability of these implants is commendable and is known to significantly improve the results of the fixed bracket appliance (25). The best site for the insertion of palatal implants is an anterior palatal region, and for buccal shelf implant is buccal to the distobuccal cusp of the 2nd mandibular molar (24). Ideally, palatal implants are indicated in cases where opening and closing the maxillary arch is essential (25). Additionally, mesial or distal movements of maxillary segments, midline shifts, correction of intercuspation, and canine or molar stabilization can also be achieved with palatal implants (26). On the other hand, buccal shelf implants are preferred for molar mesial movement, posterior teeth intrusion, occlusal plane correction, midline deviation, mandibular canine traction, retraction or distalization of canine for excessive mandibular crowding correction, and class II orthognathic surgery preparation (24). As reported in the evidence, the overall success rate of palatal implants is 91.5% (27) with significantly low failure rates (28, 29). The success rate of buccal shelf implants was also similar, at 91.3% (30). On the contrary, the 12-month survival rates of palatal and buccal shelf implants were considerably different: 90.9% for palatal and 31.3% for buccal shelf implants (27). Moreover, this finding was also supported by another study which compared the orthodontic implant insertion site. It was reported that the anterior palatal region was a better and more viable location for the insertion of orthodontic implants as compared to the buccal alveolar bone (31).

Figure 3: Trans-palatal arch and palatal implant (38)
Infrazygomatic implants
The infrazygomatic implants are preferably placed in the 1st and 2nd maxillary molar region, corresponding to the zygomatic process of the maxilla (32). A few clinicians also reported finding further anterior placement to be more suitable, according to the literature (24). Major indications for the use of infrazygomatic implants are maxillary dentition retraction in class II malocclusion, correction of the high smile line, improvement of skeletal symmetry, correction of scissor bite, posterior intrusion, maxillary dental arch distalization, molar distalization, and maxillary canine transposition (32, 33). Studies highlighting the success rate of infrazygomatic implants were scarce; however, failure rates were estimated to fall between 21-28% (34, 35). Factors which largely influenced the failure of the implant were compromised oral hygiene, immediate loading of the implant, inflammation of the implant site, clinical mobility of the tooth, and a high mandibular plane angle in the patients (35).
Conclusion
In orthodontics, skeletal anchorage systems have revolutionized the field by offering precise and effective methods for addressing a wide range of complex cases. Various components of skeletal anchorage systems, including mini-screws, mini plates, palatal, buccal shelf implants, and infrazygomatic implants, have been introduced and have significantly contributed to the diversity and effectiveness of orthodontic treatment. These anchorage methods offer effective solutions for even the most challenging orthodontic cases, greatly enhancing treatment possibilities and patient outcomes.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
