Volume 3, Issue 11
November 2023
Advances in Diastema Closure and Tooth Shape Change
Summer Khatib, Abdulaziz Alreshidi, Yasir Altamimi, Firas Alkenani, Obaid Alshammari, Essa Alrashdi, Abdullah Alshammari, Mousa Alshammari, Yazeed Alshammari, Abdalrahman Alshmri, Khalid Alshammari
DOI: http://dx.doi.org/10.52533/JOHS.2023.31112
Keywords: diastema, close, cosmetic, crown, veneer
Diastema is a prevalent condition that causes poor aesthetics and increased self-consciousness among individuals. Diastema is defined as a gap or distance of two or more neighbouring teeth. Many patients desire the closure of diastemas for cosmetic reasons. In the event of normal physiological development, diastemas with widths of less than 2 mm in nine-year-old children frequently close on their own. Although if they fail to close split Essix plates or finger springs on a detachable device, they can be used for closure. However, to control the angulations of the crown and roots in adults with broader diastemas, fixed appliances are required for correction. By using a range of alternative treatment procedures, including all-ceramic crowns, metal-ceramic crowns, porcelain laminate veneers, direct composite veneers, and indirect composite veneers, the diastema closure can be conservatively completed without the need for braces. It has become difficult for endodontists to meet the needs of young people who are used to expecting speedier aesthetic outcomes in a set amount of time. A composite resin buildup provides a solution for all of the patients' vivid needs during this crisis. Various prosthodontic rehabilitation, restorative, and orthodontic procedures and their derivative techniques are employed in dental practice for the closure of diastemas. The availability of diverse procedures and techniques in recent times has allowed the patient to achieve an aesthetically pleasing smile. In this paper, we aim to review the existing evidence from the literature for advances in diastema closure and tooth shape change.
Introduction
In the modern day, aesthetics is a top priority among people, especially the younger generation. Restorations that match the colour of teeth are becoming more and more popular. Disparities in the anterior aesthetic zones might manifest as a high frenal attachment, resulting in midline diastema, mesiodens, fractures, microdontia, and Talon's cusp. Among all these aesthetic issues, public opinion has come to value the management of midline diastema. A diastema is a gap or distance between two or more neighbouring teeth. A midline diastema is the space between the initial incisors of the jaw or maxilla. It has been suggested that there are several different contributing factors to midline diastema, such as lip, tongue, or thumb sucking. dental anomalies such as proclination in the maxillary incisor, a misaligned jaw, and a crooked fusion of the teeth (1). About 98% of six-year-olds, 49% of eleven-year-olds, and 7% of twelve to eighteen-year-olds are affected by midline diastema. According to the linear quantification of a diastema, the prevalence rates in adult populations have varied from 1.6% to 25.4%, and they have been significantly greater in younger groups (2).
For aesthetically pleasing reasons, many patients desire the closure of diastema. Diastemas with diameters of less than 2 mm in nine-year-old children often close on their own in the case of normal physiological development. If they fail to, split Essix plates or finger springs on a detachable device can be used to close small diastemas (less than 2 mm). However, fixed appliances are needed for correction in adults with wider diastemas to control the angulations of the crown and roots (3). For the treatment of midline diastema, there are a number of various treatment options that include prosthodontic rehabilitation, and restorative and orthodontic procedures. Based on time limits, and physical, physiological, and financial challenges, the practitioner can select the most appropriate treatment strategy with the help of a well-developed differential diagnosis. Conservatively closing diastemas can be accomplished with direct composite veneers, indirect composite veneers, porcelain laminate veneers, all-ceramic crowns, and metal-ceramic crowns, among other techniques. Because of its physical and chemical similarities to dentin and enamel, composite resin has been employed more frequently in the closure of midline diastemas in recent times. The patient can achieve an aesthetically pleasant smile because of the availability of numerous tints and opacities (4).
However, fixing anterior diastemas without forming black triangles between teeth is a cause for concern in clinical aesthetic dentistry. The esthetic integration of soft and hard tissues is critical to the success of restorative procedures on anterior teeth. Interdental papilla conditioning is an easy, straightforward, reliable, and inexpensive substitute. Because it restores the harmony of soft and hard tissues in terms of aesthetics, the closure of diastemas in anterior teeth with gingival recontouring and direct adhesive restorations is a practical alternative for dental practitioners (5). The interdisciplinary collaboration in smile enhancement involving periodontists, orthodontists, and restorative dentists has increased significantly over the last ten years. The growing number of interactions within the pseudo specialty of cosmetic dentistry has made dentists more aware of the norms that should direct them as they work to give their patients more aesthetically beautiful smiles. Treating diastemata has three distinct objectives: achieving a stable and effective occlusion; maintaining an environment for optimal gingival health; and sculpting a tooth form that is harmonious with the surrounding teeth, arch, and facial form. The patient should be happy with the ultimate outcome, which should be harmonious. Applying modern smile design ideas can help accomplish these objectives and clinical results (6). In recent times, the demand for aesthetic dentistry has increased significantly, and with the advancements in today’s modern era of technology, patients' need to have aesthetically pleasing smiles has governed dental practice crucially, which has urged dentists to look for more techniques that can provide optimal results, specifically in a shorter time. In this paper, we aim to review the current evidence from the literature for advances in diastema closure and tooth shape change.
Methodology
This study is based on a comprehensive literature search conducted on November 1, 2023, in the PubMed, Web of Science, Science Direct, and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed advances in diastema closure and tooth shape change. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Diastema diagnosis requires a complete medical/dental history, clinical examination, and radiographic assessment due to the possibility of several etiologies. In cases where the diastema could be caused by malocclusion or a discrepancy in the size of the teeth or arch, diagnostic study models might also be required for analysis and measurement. Any relevant medical diseases (such as hormone imbalances), oral habits, prior dental treatment and/or surgical procedures, and a family history of diastemas or other associated dental issues should all be looked into throughout the medical and dental history. Evaluation of potentially harmful oral habits, soft tissue imbalances (such as macroglossia), incorrect dental alignment (rotated teeth, extreme overbite or overjet), missing teeth, or other dental anomalies should additionally be part of the clinical examination. The frenal attachments can be assessed using the blanching test. To assess the patient's dental age and any physical constraints and anomalies in their teeth, panoramic and periapical radiographs are required. In certain cases, a Bolton's analysis and comprehensive orthodontic records may be required to rule out skeletal or dental malocclusions as well as any disparities in jaw size and/or dental size (3).
Inappropriate space distribution or disparities in tooth sizes in the anterior part of the mouth pose a serious aesthetic concern for patients. Proximally applied resin composite appears to be a more sensible and practical choice for diastema closure than other recommended treatments, which include orthodontic, restorative, and prosthodontic treatment. The preservation of tooth structure, reversibility of the process, decreased cost to the patient, and relative ease of adding or removing materials when necessary are just a few of the many advantages of direct composite restoration. Nevertheless, the restorative strategy alone is insufficient to sustain or repair a number of clinical situations. Better results might therefore necessitate an interdisciplinary strategy that incorporates two or more therapeutic modalities (7). Various strategies and practices for diastema closure are available; we discuss these approaches and techniques by classifying them into orthodontic and restorative treatments, respectively.
Aided orthodontic treatments
To close diastemata and change the shape of teeth, orthodontic therapy combined with direct composite resin veneers is a practical solution. However, when determining the course of treatment, the diastemata's etiology and extent must be carefully taken into account (8). Carruitero et al. described that extractions performed as part of orthodontic therapy are still a common course of action. Among other considerations, the decision about extraction is primarily based on the patient's initial facial profile traits. However, following orthodontic treatment, the stability of maxillary diastema closure has been extensively investigated. Relapse rates have been observed to range from 60% to 84%. While further demonstrating their findings, the authors reported that following orthodontic treatment with premolar extractions, there was no statistically significant relapse in maxillary interincisor diastema closure. For the closure of the maxillary interincisor diastema, the clinically significant stability was 72.22%; more precisely, it was 91.67% for the closure of the interincisor midline diastema (9).
Kumar et al. reported a case of a 24-year-old female who, after having a tooth between her upper central incisors removed, underwent treatment for a 4-mm maxillary midline diastema. A minimal orthodontic treatment index (grade 2) was observed. McLaughlin-Bennett-Trevisi 0.018" bonded brackets were used to suit the maxillary central incisors. Following the circular archwire, a rectangular archwire was utilized to ligate and activate the M spring. After receiving treatment for a total of four months, the diastema was successfully closed. This strategy employs the least amount of inventory and is both efficient and effective. Additionally, by doing so, the orthodontic treatment is completed faster, and more chairside time is saved (2). Figure 1 illustrates pre- and post-treatment intraoral images showing the orthodontic treatment of a median diastema with pre-adjusted Roth type (018 slot) brackets (10).
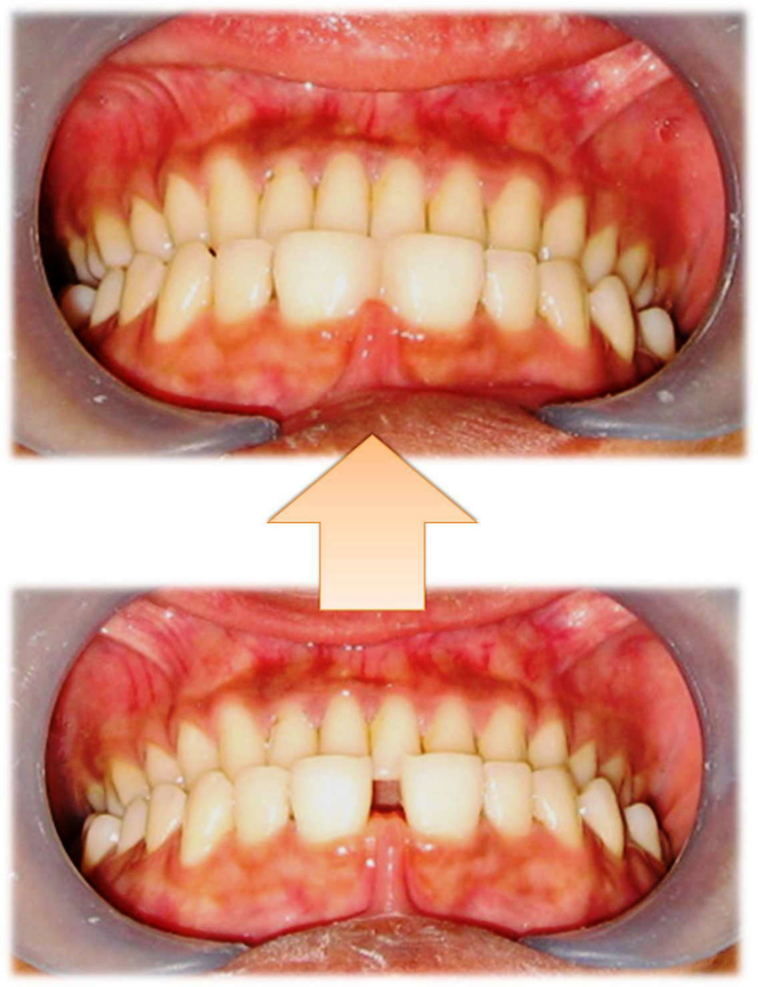
Figure 1: Pre- and post-treatment intraoral images showing the orthodontic treatment of a median diastema with pre adjusted Roth type (018 slot) brackets (10)
De Oliveria reported a case where peg-shaped lateral incisors, dental crowding, and multiple diastemata in the maxillary anterior teeth were all treated with orthodontic therapy and direct composite resin veneers. After etching, an etch-and-rinse adhesive technique was used. The composite resin veneer was built using a polychromatic layering process under rubber dam isolation. Polishing discs and abrasive materials were used to accomplish finishing and polishing procedures. Hence, patients can be satisfied with an alternative like direct composite resin since it offers predictability, aesthetics, and the opportunity to make modifications (8). Using a fully bonded and bracketed orthodontic arch device, the majority of diastema cases can be treated optimally by physiologically approximating the front tooth. The sectional arch wire approach, however, might be helpful in specific circumstances. The midline should be aligned with consideration. In most cases, permanent retention is necessary because, even with the best-managed treatment, diastema closure recurs frequently. Retention therapy recommendations include ligature wire, straight section wire, and lingual bonded fixed retainers (11).
Restorative techniques
Following the determination of the etiology, a decision must be made about the use of a multidisciplinary strategy or the simple closure of the spaces through direct and/or indirect restorative treatment. The dentist must decide which restorative therapy is ideal if the teeth are correctly positioned and aligned, but the problem is with the size of the teeth. The advancement of composite resins with exceptional polishability and mechanical qualities enables the dentist to replicate the patient's original teeth and provide a long-lasting replacement. Composite resins also allow for cautious treatment while providing faster results (12). Figure 2 shows intraoral images before and after the light-cure composite resin therapy for the median diastema closure (10). The development of an accurate contact point and emergence profile at the cervical level remains an important concern for physicians when it comes to closing a diastema with a direct composite restoration. The Front Wing Technique (FWT) is the suggested method that replaces the conventional silicone index-based and wax-up techniques. Until now, there hasn't been a practical method for moving the wax-modelled anatomy to the interproximal cervical region of anterior restorations each time these areas require restoration or correction. As a result, the FWT offers a fresh method for modelling the emergence profile freehand without creating gaps. This method can be used as a substitute for direct composite restoration of anterior teeth, which will reduce chair time and cost (13).
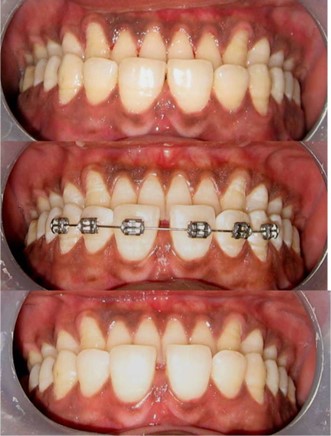
Figure 2: Intraoral images before and after the light-cure composite resin therapy for the median diastema closure (10)
Direct composite resin offers several advantages in terms of technology, such as the ability to complete the restorative process in a single appointment at a reasonable cost and without removing a healthy tooth structure. When using composite resin to close diastemas, it is crucial to utilize a rubber dam because it prevents gingiva from becoming contaminated with moisture and guarantees more gingival retraction than other methods. Better access to the tooth's cervical region is made possible by this, making it easier to properly place/fill resin to replicate the anatomical shapes and contact points. As a result, the restoration fits the gingival tissue more naturally and does not create a space between the papilla and the rebuilt tooth (14). Prabhu et al. reported that following an average of six months with the restorations in place, clinical evaluations were conducted. The findings indicate that neither of the restorations was completely lost, translating into an overall retention rate of 91% throughout the course of the 60 months. The colour of about 62% of the restored teeth did not change noticeably from the neighbouring tooth, and 73% of the sample's gingival health showed no evidence of inflammation. When composites repaired for diastemas are positioned according to suggested placement protocols and without occlusal loading, they show satisfactory survival rates (15).
Novelli et al. described that prefabricated sectional veneers are highly aesthetic restorations that do not require tooth preparation for diastema restorations. They also require a less time-consuming and technically complex clinical procedure, and the restorations are less delicate with a lower chance of breakage and post-bonding crack formation. This method presents a novel treatment option to close anterior spacing with a highly aesthetic sectional veneer in a predictable and timely manner, bridging the gap between a direct and indirect procedure for diastema repair (16). Results of a study by Chen et al. showed that for the closure of maxillary midline diastemas, sectional feldspathic porcelain veneers offered a satisfactory clinical result with a possible long-term aesthetic risk (17). Kabbach et al. reported that when applied over a modified wax up, a silicone index composed of putty polyvinyl siloxane material and another index made of putty and light polyvinyl siloxane materials helped to achieve an aesthetically pleasing diastema closure with proportionate widths that respected the gingival tissue (18).
Maluly-Proni et al. stated that a cordless displacement system and laminate veneers were used to perform a midline diastema closure therapy with minimum intervention management. In tissue displacement, it is critical to have a displacement substance that is easy to apply and rapidly activates since this lowers the duration of clinical therapy, patient discomfort, and the possibility of tissue damage (19). Naorungroj et al. narrated that aesthetic reconstruction of the diastema and open gingival embrasure can be achieved without the need for orthodontic retreatment. Injecting hyaluronic acid filler and using tooth-coloured restorations seem to be a potential way to help patients with their aesthetic concerns (20). Korkut and Turkmen reported that even more straightforward restorative methods can be used to achieve monochromatic direct composite restorations that satisfy both functional and aesthetic requirements. The longevity of various restoration types and composites was found to be comparable. Clinically, monochromatic anterior composite restorations performed well over the long term. For restorations including recontouring and diastema closure, composite repair can be appropriate (21).
Vasques et al. narrated that although direct composite resins are frequently used to close diastemas, it can be difficult to get an emergence profile without generating a step near the gingival margin and the material may not be color stable. Therefore, using a composite resin produced through computer-aided design and computer-aided manufacturing (CAD-CAM) is a great choice because it has benefits over direct restorations and even partial ceramic veneers. While dental ceramics are easily etched, predictably bonded, color stable, and wear-resistant, CAD-CAM composite resins' features allow for thinner designs that require less milling time and less chance of margin chipping than those of ceramics. Furthermore, they are easily described and repairable (22). However, more clinical research studies are needed to back the efficacy of this technique in the literature. Our review paper provides an insight into the recent techniques and their derivatives employed for the closure of diastema among patients and is supported from the findings of recent times which are the strengths of the paper however all techniques utilized for diastema closure could not be elaborately explained and some techniques may also have been overlooked during literature search which are the limitations of this study since it is beyond the scope of this paper to describe all techniques.
Conclusion
For dentists, a diastema, especially in the front region, presents an aesthetic challenge since it alters an attractive smile. The prognosis includes several critical factors, including the idea of offering minimally intrusive therapy and recognizing the possibilities for tooth preservation. Various techniques and their derivatives are employed by dentists in this current advanced era of dental practice to ensure optimal outcomes for patients in a minimum period, with each technique having its own set of advantages and disadvantages.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
