Volume 3, Issue 11
November 2023
Enhancing Tibial and Fibular Fracture Healing: A Case Report on the Value of Dynamization
Osman M. Abdulla, Firas H. Aboushaar, Naif M. Alshaeri
DOI: http://dx.doi.org/10.52533/JOHS.2023.31107
Keywords: Non-union, Delayed union, Dynamization, Tibial fracture, Intramedullary nail fixation
Background:
Tibial and fibular fractures, commonly resulting from high-energy traumas such as road traffic accidents, present difficulties in their management due to displacement, instability, and the requirement for surgical intervention.
Case presentation:
We present a 27-year-old male patient with a tibial and fibular fracture managed with intramedullary nail fixation and subsequent dynamization. The aim is to highlight the clinical significance of dynamization in addressing delayed healing and non-union in fractures. Clinical assessment and radiographic evaluation were performed to diagnose the tibial and fibular fractures. The patient underwent intramedullary nail fixation followed by dynamization. The utilization of intramedullary nail fixation demonstrated consistent outcomes with established literature. However, delayed healing and non-union were observed. The introduction of dynamization after failed healing attempts led to significant improvements in callus formation and fracture healing.
Conclusions:
This case emphasizes the value of dynamization as a strategy to enhance fracture healing, particularly in cases of delayed union or non-union. Dynamization represents a promising adjunctive approach in orthopedic fracture management.
Introduction
Tibial and fibular fractures are common orthopedic injuries that often result from high-energy traumas such as road traffic accidents (1, 2). These fractures can be challenging to manage due to their potential for displacement, instability, and the need for appropriate surgical intervention (3). The treatment approach for these fractures has evolved over the years, with the aim of achieving stable fixation, promoting bone healing, and optimizing functional outcomes for patients (3). One crucial aspect of this evolution has been the utilization of intramedullary nail fixation, which has become a standard of care for many tibial fractures (4, 5). Furthermore, the concept of dynamization, which involves controlled axial loading of the fracture site, has gained increasing recognition for its role in promoting bone healing in cases where primary fracture fixation alone may not suffice (6, 7).
While intramedullary nailing offers many advantages in the management of tibial fractures, there are instances where fracture healing may be delayed or impaired (7). Delayed union or non-union can occur for various reasons, including inadequate blood supply, excessive gap at the fracture site, or insufficient biomechanical stimulation. It is in cases like these that the concept of dynamization becomes relevant (6).
Dynamization involves the modification of the fracture fixation construct to encourage load-sharing between the implant and the healing bone (6). This controlled axial loading stimulates callus formation and enhances the bone healing process. The rationale behind dynamization is to mimic the physiological conditions required for effective fracture healing (6, 7). By allowing micromotion at the fracture site, dynamization can promote secondary bone formation and accelerate the union process (8, 9).
The use of dynamization in orthopedics has gained attention for its potential to enhance healing in cases of delayed union or non-union. This technique is especially valuable when standard fracture fixation alone has not yielded the desired results. By introducing controlled micromotion, dynamization promotes the biological response of the bone, leading to increased callus formation and ultimately, fracture union (9, 10).
Dynamization is typically achieved through various means, including the removal of blocking screws, the conversion of a statically locked nail to a dynamically locked nail, or the application of specialized dynamization devices. The decision to employ dynamization is based on clinical and radiographic assessments, and it is crucial to strike a balance between providing adequate stability and allowing controlled movement (6-8).
Case Presentation
On January 10, 2023, a 27-year-old male with no significant medical history presented to our emergency department after a road traffic accident. The patient was transported to the hospital by a relative, complaining of severe left leg pain, swelling, an obvious deformity, and abrasions over the left leg. A comprehensive examination, including inspection and palpation, revealed tenderness, swelling, and an apparent deformity of the left leg. No signs of open wounds were observed during the examination.
Clinical examination findings indicated intact distal neurovascular status, including dorsalis pedis and posterior tibialis arteries. The oxygen saturation of the left leg remained consistently at 100%, as measured by pulse oximetry. Vital signs, including blood pressure, heart rate, respiratory rate, and temperature, were within normal ranges and consistent with the expected findings in tibial fractures.
Despite the absence of significant medical comorbidities, routine blood work was performed to rule out any potential metabolic or infectious causes contributing to the fracture. Results indicated non-significant findings, eliminating concerns related to underlying systemic issues.
The patient, a non-smoker, was not on any medications that might impede fracture healing, such as NSAIDs or fluoroquinolones. The prescribed common management did not include any medications with known adverse effects on bone healing.
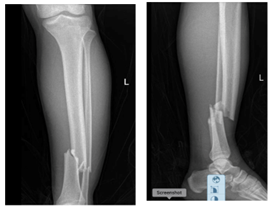
Upon consultation with the orthopedic team, it was determined that surgical intervention was necessary. Before the procedure, the fractures underwent reduction, and an above-knee back slab was applied under intravenous pethidine 50 mg. Following the reduction, the patient underwent an X-ray of the left leg, confirming the fractures of the left tibia and fibula (Figure 1).
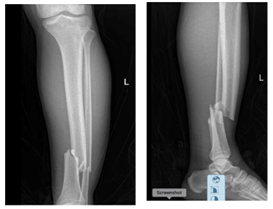
Figure 1: Initial X-ray of the Left Leg (The X-Ray shows the left leg showing the tibial (white arrow) and fibular (red arrow) fractures. This image served as the basis for the diagnosis and treatment plan).
On January 19, 2023, surgical fixation was performed, involving reaming of the intramedullary canal and the introduction of an intramedullary nail fixation measuring 11x34 mm. This procedure was completed without any intraoperative complications (Figure 2). The fibula fracture was conservatively managed, and the patient-initiated physiotherapy to encourage early mobilization.
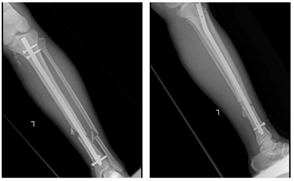
Figure 2: Intraoperative X-ray after Intermedullary Nail Fixation (This X-ray taken immediately after the successful intermedullary nail fixation procedure (white arrow). The image demonstrates the position and stability of the implant).
Postoperatively, the patient experienced an uneventful recovery and was discharged three days after the operation. Outpatient department follow-up visits were scheduled for 10 days post-discharge. The first visit on February 1, 2023, revealed a clean and dry wound with staple removal. However, the X-ray at the second follow-up visit on February 19, 2023, showed no evidence of healing or callus formation (Figure 3).

Figure 3: X-ray at Subsequent Follow-Up (This X-ray taken during a follow-up visit, which revealed a lack of healing progress and callus formation (white arrow). This finding prompted further intervention).
In response to the observed lack of healing progress, the decision was made to perform dynamization of the proximal screws on March 16, 2023. This intervention aimed to introduce controlled micromotion to stimulate callus formation and enhance bone healing. The intraoperative process of dynamization involved the careful modification of the fixation construct, facilitating axial loading at the fracture site. While intraoperative images were not captured, subsequent X-ray imaging confirmed the successful dynamization of the construct (Figure 4).
Subsequent follow-up visits demonstrated encouraging signs of callus formation at the first visit after proximal screw removal on March 29, 2023. The second visit on May 2, 2023, further revealed evidence of healing. By the third visit on July 9, 2023, significant improvements were evident on the X-ray, displaying healing and callus formation at the fracture site (Figure 5). The patient exhibited enhanced weight-bearing capacity and reduced pain, indicating successful fracture healing.

Figure 4: X-ray after Dynamization of Proximal Screws (X-ray image taken following the dynamization of proximal screws (white arrow). It showcases the changes in the fixation construct after introducing controlled micromotion).
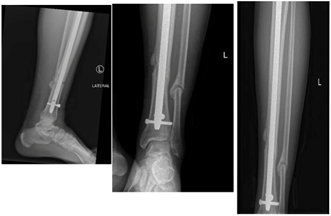
Figure 5: X-ray Showing Signs of Healing and Improvement (X-ray taken during a later follow-up visit, indicating significant signs of healing and improvement at the fracture site (white arrow). The image highlights the positive outcome achieved with dynamization)
Discussion
The presented case of a tibial and fibular fracture managed with intramedullary nail fixation, followed by dynamization, underscores the importance of a tailored and dynamic approach to fracture management.
The utilization of intramedullary nail fixation for the treatment of tibial fractures in our case is consistent with established literature (4, 5). Intramedullary nailing has become the gold standard for managing diaphyseal tibial fractures due to its biomechanical advantages, including enhanced stability and early mobilization (11). The procedure facilitates anatomical reduction and provides robust support, reducing the risk of malunion or non-union compared to conservative methods. This aligns with the findings of numerous studies that have demonstrated favorable outcomes with intramedullary nailing in tibial fracture management (11-14).
Delayed Healing and Non-Union: A Clinical Challenge
Despite the recognized benefits of intramedullary nailing, some tibial fractures may exhibit delayed healing or non-union, which was observed in our case. This phenomenon is not uncommon and has been extensively studied (6, 7). Factors contributing to delayed healing or non-union include poor vascular supply, infection, excessive fracture gap, or inadequate biomechanical stimulation (15). These challenges necessitate a multifaceted approach to fracture management.
The Value of Dynamization in Fracture Healing
Dynamization, introduced in our case as a means to address delayed healing, is a technique that has gained prominence in recent years. Its fundamental principle revolves around promoting controlled micromotion at the fracture site to stimulate callus formation and enhance bone healing (6). This approach is grounded in the understanding that mechanical forces play a crucial role in regulating bone remodeling and tissue differentiation (8).
The decision to employ dynamization was supported by the lack of healing progress evident in successive radiographic assessments. This decision aligns with studies that advocate for dynamization as an effective strategy in cases of delayed union or non-union (7, 8). By introducing controlled axial loading, dynamization creates a microenvironment conducive to bone regeneration, which can expedite the healing process (6).
The case presented here is in concordance with a growing body of literature that underscores the benefits of dynamization in cases of delayed healing or non-union. Several studies have demonstrated the positive impact of dynamization on fracture healing, showing increased callus formation, enhanced bone union, and ultimately, improved clinical outcomes (6-9, 16-17).
Furthermore, the timing and method of dynamization may vary among studies and clinical scenarios. Some research suggests early dynamization, while others advocate for a staged approach (16). The choice depends on individual patient factors and fracture characteristics. In our case, dynamization was employed after an initial period of non-union was observed, with successful results, consistent with similar studies in the literature.
Clinical Implications and Future Directions
The presented case highlights the importance of a flexible and evidence-based approach in orthopedic fracture management. While intramedullary nail fixation remains a robust option for tibial fractures, the occurrence of delayed healing or non-union underscores the need for vigilant monitoring and timely intervention.
Dynamization represents a valuable tool in the orthopedic surgeon's armamentarium, offering the potential to salvage cases that might otherwise progress to non-union. However, its application should be guided by clinical judgment, and not all cases warrant dynamization. Future research should continue to explore the optimal timing and techniques of dynamization and refine our understanding of which patients are most likely to benefit from this approach.
Despite meticulous management, the initial non-union observed in this case prompted the implementation of dynamization, ultimately leading to successful fracture healing. Hypothesizing on the cause of non-union, we postulate that factors such as the severity of the initial trauma, individual patient variability in bone healing response, and the specific fracture pattern may have contributed. Further research and larger-scale studies are warranted to elucidate the multifactorial nature of non-union in tibial fractures and refine treatment strategies for optimal outcomes.
Conclusion
In conclusion, the presented case of a tibial and fibular fracture managed with intramedullary nail fixation and subsequent dynamization exemplifies the evolving landscape of fracture management. While intramedullary nailing remains a mainstay in treating tibial fractures, the potential for delayed healing or non-union underscores the importance of adaptive strategies. Dynamization, with its capacity to stimulate bone healing through controlled micromotion, represents a valuable adjunctive approach. The case and findings presented here contribute to the growing body of evidence supporting the role of dynamization in achieving successful fracture healing and optimizing patient outcomes in challenging orthopedic cases.
Acknowledgements
We would like to thank the orthopedic department at South Qunfidah General Hospital for being so helpful.
Disclosure
Statement:
The authors declare no conflict or interest.
Funding:
None.
Ethical Consideration:
An informed written consent was taken from the patient to report this case without revealing any personal information and approval was not required for publication, as this is a case report.
Data availability:
All data is available withing the article.
Author Contribution:
All authors have read and approved the manuscript. All authors have contributed equally to this manuscript.