Volume 3, Issue 11
November 2023
Microleakage Among Different Dental Restorative Materials: Causes, Detection, and Impact on Marginal Integrity
Waleed Aljehani, Alanoud Almakinah, Abrar Alshahri, Omar Albluwy, Shooq Alamray, Amal Alaiyed, Mohammed Alqahtani, Saja Faqiehi, Nadiyah Alasmari, Abdulrahman Alkhaldi, Fay Alenazy
DOI: http://dx.doi.org/10.52533/JOHS.2023.31106
Keywords: Dental restorations, amalgam, composite resin, microleakage, gaps, secondary caries, marginal integrity
Dental restorative materials are essential components in the field of dentistry, serving as compounds or substances used to address a wide spectrum of dental concerns, including cavities, tooth decay, fractures, and cosmetic enhancements. These materials, encompassing amalgam, composite resins, glass ionomer cement, and compomers, are carefully selected based on their specific properties and the requirements of the restorative procedure. However, dental restorations are intricate processes influenced by patient factors and material behaviour, which can lead to various complications. Among these, microleakage emerges as a prevalent and multifaceted issue, with causes ranging from polymerization shrinkage during material curing to thermal changes, cyclic loading, and moisture contamination. The consequences of microleakage are far-reaching, encompassing clinical challenges such as the development of secondary caries, tooth sensitivity, aesthetic concerns, and the potential for restoration failure. The susceptibility to microleakage varies among different dental restoration materials, with amalgam typically exhibiting lower susceptibility compared to more modern alternatives like composite resins and compomers. Glass ionomer cement, when employed with appropriate moisture control, can demonstrate improved resistance to microleakage over time. Detecting microleakage necessitates various methods, including radiography, dye penetration tests, electron microscopy, and microcomputed tomography. Effective prevention and management strategies involve the use of modern adhesive systems, precise restoration techniques, and patient education on maintaining optimal oral hygiene. Continual advancements in dental materials and techniques further contribute to the ongoing efforts to mitigate the challenges posed by microleakage in the ever-evolving landscape of modern dentistry, ultimately enhancing patient outcomes and ensuring the longevity and success of dental restorations while prioritizing overall oral health.
Introduction
Dental restorative materials are substances or compounds used in dentistry to repair, replace, or restore damaged or missing teeth and tooth structures. These materials are fundamental in a wide range of dental procedures, serving to address issues such as cavities, tooth decay, fractures, and cosmetic enhancements (1). Dental materials specifically used for tooth restorations include metal alloys, polymers, ceramics, and composite resins (2). These materials are chosen based on their properties and restorative needs. Amalgam is a traditional dental restorative material commonly used in dental fillings, despite a decline in popularity in recent years due to concerns about its mercury content and its silver appearance. Amalgam fillings are composed of a mixture of metals, including silver, tin, copper, and mercury. The term "amalgam" refers to the chemical bonding of these metals to form a stable, solid compound (1). Amalgam fillings are known for their durability and strength, making them suitable for restoring posterior (back) teeth subjected to heavy chewing forces. Amalgam fillings are relatively easy to place and are cost-effective compared to some alternative materials (2). However, concerns have arisen regarding the mercury content in amalgam. While the mercury in amalgam is bound in a stable alloy, some individuals worry about potential mercury vapor release during placement, removal, or as the filling ages. As a result, there has been a shift towards more aesthetically pleasing dental restorative materials like composite resins, which match the colour of natural teeth. Composite resins are a popular and versatile dental restorative material commonly used in dental fillings. Composite resins are tooth-coloured and closely mimic the appearance of natural teeth, making them an excellent choice for restoring front teeth and other visible areas of the mouth (2). Composite resin dental fillings are composed of a mixture of resin-based materials and fine particles of glass or ceramic. When placed in a tooth cavity, these materials are applied in layers and then hardened with a special curing light (2). This process allows for precise shaping and contouring, resulting in a restoration that blends seamlessly with the surrounding tooth structure. One of the significant advantages of composite resin fillings is their aesthetic appeal. They can be colour-matched to the patient's natural teeth, ensuring that the filling is virtually indistinguishable. Furthermore, composite resins bond well to the tooth structure, which can help preserve more of the natural tooth and provide additional support (1). Another dental filling material is glass ionomer cement (GIC). GIC is unique because it can bond directly to the tooth structure and release fluoride, making it a versatile and beneficial choice in certain clinical situations (2). The fluoride releasing property helps prevent tooth decay and promotes the remineralization of the enamel. This makes GIC a suitable choice for restoring cavities in primary (baby) teeth as well as in low-stress areas in adult teeth. It is particularly beneficial for paediatric dentistry, where it can be used to restore decayed baby teeth, as it aids in strengthening adjacent tooth structures (3). However, GIC is not as durable as some other materials like composite resins or amalgam, and it may be more prone to wear and fracture in high-stress areas of the mouth (2). To find an ideal and aesthetically pleasing material as well as a durable restorative material, a hybrid between composite resin and GIC was developed, known as compomer. Compomers are dental restorative materials that combine the characteristics of composite resins and glass ionomer cements (1). These materials were developed to offer certain advantages of both composite resins and GICs while minimizing some of their limitations. Compomers are easy to match with the patient's tooth, similar to composite, however, they also carry the ability to release fluoride and promote tooth remineralization, mimicking GIC restorations (4). Since dental restorations are multifaceted procedures, depending on the patient's characteristics as well as material behaviour, they can encompass a range of complications and challenges. Chipping or fracture, dislodgment, periodontal or pulpal issues, recurrent caries, and allergic reactions are some of the complications that can arise after a dental restoration (2). Microleakage stands as a prevalent concern within the realm of dental restorations, and its repercussions can encompass an array of clinical issues. This phenomenon revolves around the minuscule fissures or apertures that manifest at the boundary where a dental restoration interfaces with the surrounding tooth structure (5). These minuscule crevices facilitate the ingress of bacteria, fluids, and debris, potentially culminating in the development of secondary cavities, caries, and a spectrum of other complications (5). The occurrence and extent of microleakage hinge on a medley of determinants, embracing the choice of dental restorative material, the existing state of the tooth, the technique employed for the restoration procedure, and the patient's oral hygiene habits (5). Furthermore, one must recognize that various attributes intrinsic to dental materials, such as biocompatibility, strength, thermal compatibility, and chemical stability, can exert a significant influence on the extent and severity of microleakage. In addition to that, microleakage, as a gateway to secondary caries, can result in failed endodontic procedures, making the tooth more vulnerable to brittleness. In essence, microleakage represents a significant and widespread concern within the context of dental restorations, giving rise to a plethora of clinical challenges.
The study on microleakage among different dental restorative materials aims to address a critical concern in contemporary dentistry. Dental restorations are essential for preserving oral health and function, but their long-term success relies heavily on the integrity of the restoration-tooth interface. Microleakage poses a significant challenge to this dynamic, and hence, should be explored. This study is motivated by the need to comprehensively understand the causes, detection methods, and implications of microleakage in various dental restorative materials to enhance the longevity and effectiveness of dental restorations. The causes of microleakage are multifaceted, and investigating these causes will provide insights into the complexities of this phenomenon and guide the development of strategies to mitigate its occurrence. Additionally, detecting microleakage accurately is equally vital in clinical practice. Furthermore, the study will also delve into the impact of microleakage on marginal integrity, underscoring the clinical significance of preventing and managing microleakage effectively. This study aims to fill a critical knowledge gap by comprehensively investigating microleakage in various dental restorative materials. By addressing the causes, detection methods, and impact on marginal integrity, this research will contribute to improved clinical decision-making, enhanced patient outcomes, and the advancement of dental materials and techniques to mitigate the challenges posed by microleakage in modern dentistry.
Methodology
The initiation of this research project on October 8th, 2023, was prompted by an extensive examination of existing scholarly works, employing renowned databases such as PubMed, Web of Science, and Cochrane. The quest for relevant literature entailed the utilization of a diverse spectrum of medical terminology combinations, alongside manual exploration of pertinent research terminologies through Google Scholar. The principal aim of this literature survey encompassed several pivotal domains, including dental restorative materials, their various classifications, associated complications, the intricate concept of microleakage, the underlying causes of microleakage, the pivotal aspect of marginal integrity, and the variety of techniques utilized for the detection of this phenomenon. It is imperative to underscore that the articles meticulously shortlisted for inclusion in this study underwent rigorous scrutiny, adhering to a set of discerning criteria, thereby ensuring the attainment of a comprehensive and robust foundation for the research endeavour.
Discussion
Microleakage is a common issue in dental restorations that can lead to various clinical problems. It refers to the tiny gaps or openings that develop at the interface between a dental restoration and the tooth structure. These gaps can allow the ingress of bacteria, fluids, and debris, potentially leading to secondary caries (cavities) and other complications (1). Microleakage is influenced by several factors, including the choice of dental restorative material, the tooth's condition, the restoration technique, and the patient's oral hygiene.
Causes of Microleakage
Polymerization shrinkage
Polymerization shrinkage is a phenomenon commonly observed in dental restorative materials, with resin-based composites being particularly susceptible during the curing process. This shrinkage occurs as the material transforms from a pliable, initially malleable state to a solid, hardened form (6). During this transformation, the material contracts or shrinks, leading to a reduction in volume. Therefore, this contraction can give rise to tiny gaps or spaces that materialize between the dental restoration and the surrounding tooth structure (7). These gaps compromise the integrity of the restoration by providing pathways for microleakage, enabling the infiltration of bacteria, fluids, and debris into the crevices (8). This, in turn, can lead to issues such as secondary caries, post-operative sensitivity, and the potential for restoration failure over time (8). Dentists and researchers continually explore strategies to mitigate the effects of polymerization shrinkage, including the development of low-shrinkage restorative materials (9), improved bonding techniques, and incremental layering during restoration placement (10). These efforts aim to strike a balance between achieving adequate polymerization for material strength and minimizing shrinkage-related complications to enhance the long-term success of dental restorations.
Thermal changes
Thermal changes are a significant factor in the dynamic behavior of dental materials and natural tooth structures within the oral environment. This phenomenon involves the expansion and contraction of these materials in response to temperature fluctuations, a process that can have implications for the integrity of dental restorations and the overall oral health of patients (11). Dental materials have specific coefficients of thermal expansion, which dictate how much they expand or contract in response to changes in temperature. These inherent properties mean that dental restorations and the surrounding tooth structure are not immune to the effects of temperature fluctuations. As temperatures rise and fall due to factors like hot and cold foods or beverages, ambient temperature changes, or even exposure to hot and cold air during breathing, dental materials and tooth structures undergo corresponding expansion and contraction (11). This thermal cycling can create stress at the interface between dental restorations and tooth tissues. Over time, this stress can potentially lead to the formation of minute gaps or micro gaps at the restoration-tooth interface (12).
Cyclic loading
Cyclic loading, a crucial consideration in restorative dentistry, refers to the repetitive mechanical stresses that dental restorations and the surrounding tooth structures experience during the various movements associated with normal oral function, primarily biting and chewing. These forces exerted on dental restorations can result in the generation of stress at the interface between the restoration and the tooth, potentially leading to microleakage (13). As individuals perform everyday activities such as biting into food, chewing, and grinding, the teeth and any dental restorations in place are subjected to cyclic loading. These forces can vary in magnitude and direction depending on the type and location of the dental restoration, the specific tooth involved, and the nature of the occlusion (14). The ability of dental restorative materials to withstand cyclic loading and maintain their integrity is a critical consideration in restorative dentistry. Dentists carefully select restorative materials and techniques that can withstand the mechanical stresses of the oral environment, especially in areas subjected to significant masticatory forces.
Moisture
Moisture and saliva, although essential components of the oral environment, can pose significant challenges during dental restoration procedures, particularly when they infiltrate the restoration-tooth interface. These factors have the potential to disrupt the bonding process and are often associated with microleakage. During restorative dental procedures, maintaining a dry and moisture-free operating field is paramount for achieving successful adhesive bonding between dental restorative materials and tooth structure (15). Many contemporary dental restorative materials, especially adhesive systems and resin-based composites rely on adhesive bonding to establish a robust connection with the tooth. Moisture can interfere with the effectiveness of adhesives, diluting them and impeding their infiltration into the tooth structure (15).
Detection of microleakage
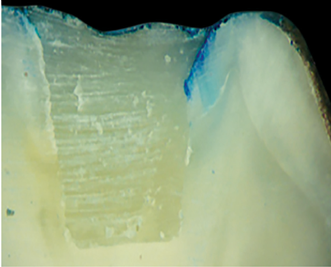
Microleakage can be detected through various methods, depending on the availability of these tools within the clinical setting. The first method is basic radiography. X-rays can be used to detect gaps or voids at the restoration margins; however, they are unable to identify smaller gaps, which can be better noted by other methods of microleakage detection (16). Another method of detection can be through a dye penetration test, which involves applying a colored dye at the restoration interface and observing if it is seeping into the gaps, as illustrated in Figure 1 (17).
Figure 1: Assessment of microleakage using dye penetration method (28)
The penetrated dye makes the gaps visible to either the naked eye or under a microscope. Commonly used dyes are 0.5% basic fuchsin, 2% methylene blue, and 50% silver nitrate (18). Electron microscopy is another type of microleakage detection method that is robust; however, due to its lack of availability in general clinical settings, it is not used as widely. Scanning electron microscopy (SEM) and transmission electron microscopy (TEM) can provide high-resolution images of the interface, revealing microleakage (17). Lastly, microcomputed tomography (Micro-CT) is an advanced imaging technique which provides a three-dimensional view of the restoration tooth interface, showing microleakage in detail (19). This technique allows the precise measurement of the gaps, making it easier for the clinician to plan the management strategy (17).
Impact on marginal integrity
The impact of microleakage on marginal integrity within dental restorations is a multifaceted concern that can have significant implications for a patient's oral health and the longevity of the restoration, as depicted in Figure 2.
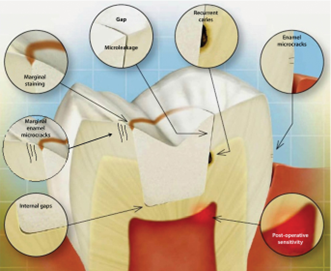
Figure 2: Impact of microleakage on marginal integrity of composite restoration (29)
Microleakage, characterized by the infiltration of bacteria, acids, fluids, and debris into minute gaps or openings at the margins of dental restoration, can give rise to a cascade of clinical issues, particularly affecting the integrity of the restoration's margins. One of the most pressing concerns associated with microleakage is the development of secondary caries (5). As microleakage permits the ingress of bacteria and acids into the crevices, these pathogens find a conducive environment to thrive. Over time, this microbial activity can lead to the demineralization of the tooth structure surrounding the restoration margins, resulting in the formation of secondary cavities or caries (20). These carious lesions often remain hidden beneath the restoration, making them challenging to detect until they progress to a more advanced stage (20). Secondary caries not only jeopardize the health of the affected tooth but can also compromise the overall integrity of the restoration. Microleakage can also manifest as tooth sensitivity, a discomforting condition that patients frequently report. The movement of fluids within the microgaps created by microleakage can result in heightened sensitivity to temperature changes, particularly when consuming hot or cold foods and beverages (21). Additionally, sensitivity to sweets and pressure may ensue, making daily activities like eating and drinking uncomfortable or painful. This sensitivity can significantly impact a patient's quality of life and may necessitate additional dental interventions to address (22). As time progresses, the cumulative effects of microleakage can weaken the bond between the restoration and the tooth. This marginal breakdown can compromise the overall structural integrity of the restoration, potentially leading to failure. When this occurs, the restoration may dislodge or break, necessitating replacement (22). This can be both clinically and economically burdensome for patients, as it often entails additional dental procedures and associated costs.
Relationship of microleakage with type of restoration material
Microleakage can vary depending on the type of restoration material used because each material has unique properties that influence its susceptibility to microleakage. Microleakage with amalgam restorations is relatively low. Its ability to adapt closely to cavity walls and expand slightly upon setting helps create a good seal, reducing the likelihood of microleakage. However, over time, amalgam restorations can corrode and degrade, potentially leading to gaps or marginal breakdown. Evidence suggests that physical stressors such as ionizing radiations and non-ionizing electromagnetic fields can fasten the release of mercury from the amalgam filling, causing microleakage over time (23). On the other hand, GICs may exhibit some initial microleakage due to their initial setting characteristics, these fillings tend to improve with time as they bond with the tooth structure due to their ability to have higher dimensional stability, lower thermal conductibility, and better chemical adhesion to the tooth (24). The presence of moisture during placement can negatively affect the bonding of GICs, leading to increased microleakage. Therefore, proper isolation and moisture control are crucial when using GICs (13). Composite resins have become popular for their esthetic properties, but they are also prone to microleakage. Their polymerization shrinkage during curing can create gaps at the restoration margins, increasing the risk of microleakage (25). However, advances in composite materials, along with techniques such as incremental layering and the use of low-shrinkage composites, have helped reduce the extent of polymerization shrinkage and, consequently, microleakage (12). Compomers are a hybrid of composite resin and glass ionomer cement, designed to combine some of the advantages of both materials. They exhibit less polymerization shrinkage than traditional composites, which may reduce the potential for microleakage (26, 27). It is crucial to note that the risk of microleakage is not solely determined by the type of restoration material but also by factors like the skill of the dentist, the quality of the restoration placement, and the patient's oral hygiene practices. Furthermore, advancements in dental materials and techniques continue to evolve to reduce microleakage and enhance the longevity and effectiveness of dental restorations across all material types.
Prevention and management of microleakage
One of the best prevention strategies for microleakage is the use of modern adhesive systems, which can improve bond strength and reduce microleakage (15). Moreover, proper cavity preparation and restoration techniques can also minimize polymerization shrinkage stress and improve marginal integrity. The choice of dental restorative material should consider factors like the tooth's location, function, and esthetic requirements. Finally, patients should be encouraged to maintain good oral hygiene and attend regular dental check-ups to detect and address microleakage issues early.
Conclusion
In summary, microleakage in dental restorations is a pervasive concern with multifactorial causes, including polymerization shrinkage, thermal changes, cyclic loading, and moisture contamination. These tiny gaps or openings at the restoration margins can lead to various clinical problems, such as secondary caries, tooth sensitivity, esthetic issues, and potential restoration failure. The susceptibility to microleakage varies among different restoration materials, with amalgam generally exhibiting low susceptibility, while composite resins and compomers are more prone to it. Glass ionomer cement, when used with proper moisture control, can exhibit improved resistance to microleakage over time. Detection methods, including radiography, dye penetration tests, electron microscopy, and microcomputed tomography, aid in identifying microleakage and planning appropriate interventions. Prevention and management strategies involve the use of modern adhesive systems, meticulous restoration techniques, and patient education on maintaining good oral hygiene. Additionally, advancements in dental materials and techniques continue to evolve to minimize the impact of microleakage, emphasizing the importance of comprehensive care to ensure the long-term success and durability of dental restorations and the overall oral health of patients.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.