Volume 3, Issue 11
November 2023
Timing, Requirement, and Clinical Perspective of Early Intervention in Orthodontic
Jamal Alqahtani, Kholod Alshehri, Deemah Albrahimi, Renad Alqahtani, Asma Alenezi, Bashayr Alanazi, Shahad Almuzaini, Elaf Alshaeri, Hala Alzaidi, Ghaida Alfagih, Motlaq Al Mutairi
DOI: http://dx.doi.org/10.52533/JOHS.2023.31105
Keywords: Early orthodontic treatment, posterior crossbite, class II, class III
Early orthodontic intervention, commonly referred to as Phase 1 or interceptive orthodontics, aims to correct dental misalignment and bite issues in children aged six to ten. This article synthesizes current evidence-based studies and clinical experiences to provide a comprehensive understanding of the timing, necessity, and efficacy of early orthodontic treatment. Topics explored include the correction of posterior crossbites, Class III and Class II malocclusions, open bites, and arch length disparities. The article underscores the advantage of leveraging the child's ongoing growth for easier and more effective treatment, thereby potentially minimizing future complications and surgical interventions. It also highlights the importance of early intervention in enhancing emotional well-being in children by addressing associated psychological concerns. However, it notes that the effectiveness of early treatment in cases of Class II malocclusions, open bites, and arch length discrepancies is still debated among professionals. The article aims to equip orthodontists with knowledge and clinical insights for optimal early intervention strategies, offering tried-and-true methods where research evidence is inconclusive.
Introduction
Early orthodontic treatment, commonly known as Phase 1 or interceptive orthodontics, is an approach aimed at children aged six to ten, with the objective of addressing bite and dental alignment issues during their developmental stages. The rationale for early intervention lies in leveraging the ongoing growth of facial and jaw bones to facilitate easier and more effective corrections (1). Such treatments can encompass a range of orthodontic devices, including removable appliances, partial braces, and more. The American Association of Orthodontists advises that children have their initial consultation with an orthodontic expert as soon as a potential orthodontic issue is identified, but definitely by the time they are seven years old. Research shows that early intervention for specific types of dental misalignment can be advantageous. This can reduce the duration of subsequent treatments (2). Additionally, correcting these issues early can have a positive impact on a child's emotional well-being by addressing psychological concerns linked to their dental misalignment, as noted by Artese et al. in 2019 (3). The aetiology of a malocclusion may be due either to dental components or to skeletal causes (4). Early treatment can correct posterior crossbites and Class III malocclusion with lasting effects. However, the effectiveness of Class II malocclusions, open bites, and arch length disparities remains disputed. Orthodontists rely on training and experience in these cases (2). Early intervention can offer various advantages, such as enhancing a child's emotional well-being, maximizing growth during this developmental period, improving compliance with treatment, paving the way for a more straightforward second phase, and potentially minimizing the necessity for tooth extractions in subsequent corrective stages. This article aims to provide contemporary knowledge regarding the timing, need, and clinical insights of early orthodontic intervention. It presents findings from evidence-based studies on the subject, and where research is debatable it offers readers tried-and-true short-term treatment methods based on the authors' past experiences.
Methodology
This study is based on a comprehensive literature search conducted on September 23, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the timing, requirements, and clinical perspective of early intervention in orthodontics. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Early orthodontic treatment, also known as Phase 1 or interceptive orthodontics, is typically recommended for children between the ages of six and ten. The aim is to correct bite and dental alignment problems while the child's jaw and facial bones are still growing, making it easier to fix issues that may become more complicated as they age. Treatment can involve removable appliances, partial braces, or other orthodontic devices (1). Table 1 & 2 shows a summary of both advantages of disadvantages of different orthodontic treatment.
|
Table 1. Advantages of early orthodontic treatment, along with relevant references for each point. |
|
|
Advantages of early Orthodontic treatment |
Description |
|
Corrects Bite Issues (1) |
Issues such as overbites, underbites, and crossbites can be effectively corrected. |
|
Improves Space for Permanent Teeth (5) |
Early treatment can make room for crowded, incoming teeth. |
|
Decreases Risk of Tooth Damage (6) |
Protruding or misaligned teeth are at a higher risk for chipping or breaking. |
|
Psychological Benefits (7) |
Improved appearance can enhance self-esteem in children. |
|
Cost-Effective (8) |
Early treatment can sometimes prevent the need for more extensive and expensive treatments later. |
|
Table 2. Disadvantages of early orthodontic treatment, complete with relevant references for each point. |
|
|
Disadvantages of early Orthodontic treatment |
Description |
|
Longer Treatment Time (9) |
Some children might undergo a two-phase treatment, which can extend the overall time they spend in braces. |
|
Over-Treatment (10) |
There is a possibility that some children might be treated who would otherwise have outgrown their orthodontic problems. |
Posterior crossbite
Posterior crossbites in baby teeth are commonly observed, with a reported occurrence rate ranging from 8% to 22% (11, 12). The primary cause of these crossbites is a narrowing of the upper jaw (maxilla), often coupled with a discrepancy in the length of the maxillary arch. This can result in shifts in the lower jaw's (mandible) position due to interference from the teeth. About 80% of all one-sided posterior crossbites in mixed dentition arise from such functional mandibular shifts. While there are instances of these crossbites self-correcting, it is more common for the issue to persist into the adult teeth. When this happens, it often leads to uneven muscle activity and skewed growth of the mandible, elevating the risk of future issues with the temporomandibular joint. Therefore, the persistence of such conditions may not only affect dental alignment but could also have broader implications for jaw function and overall oral health (13, 14). To mitigate potential negative consequences, it is advisable to begin early orthodontic care as soon as the child and their parents are receptive to the idea. The objective is to achieve regular bite alignment, which ensures the right bite development as the child grows. Doing so keeps the first permanent molars from emerging misaligned and reduces the likelihood of requiring more complex orthodontic interventions later on (15-17).
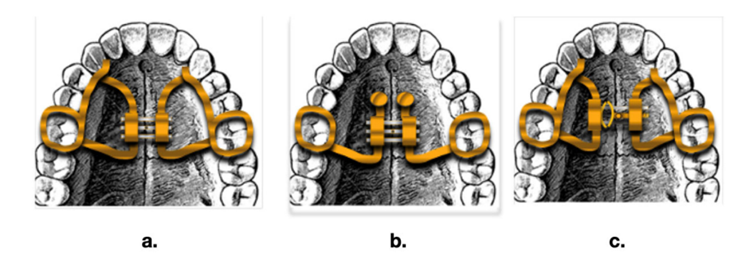
The preferred device is a Rapid Palatal Expander (RPE), which is divided into three types (Figure 1) (18). Daily use for four to six weeks is typical to address transverse differences, followed by 9–12 months of stabilization. Retention devices are not needed if no other issues exist. While Masucci et al. noted a 30–40% relapse after palatal expansion in baby teeth, others found long-term stability after early crossbite corrections (19).
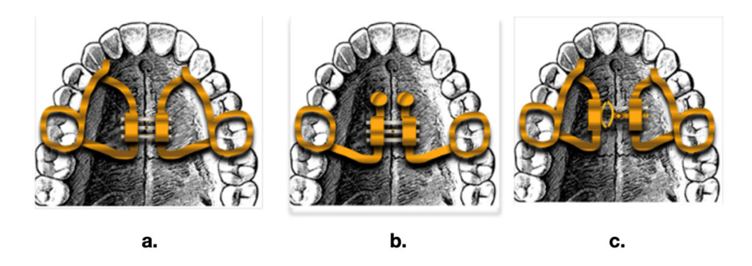
Figure 1: Three different types of palatal expander: (a) Hyrax expander; (b) Rep on mini screws; (c) Leaf expander (18).
Class III malocclusion
Since Class III malocclusion tends to worsen during adolescent growth, early interception is recommended, preferably during the deciduous dentition phase, to gain maximum skeletal effect from orthodontic treatment. A cephalometric analysis is also vital to ascertain the degree of underlying front-to-back and up-and-down jaw discrepancies. Additionally, it is essential to check for any particularly adverse genetic tendencies in the family's medical history (2).
For inherited Class III malocclusions, a cephalometric x-ray assesses the Wits appraisal, vital for evaluating early intervention success and vertical skeletal dimension. A pronounced Wits value (-7mm or more) with a hyperdivergent pattern might necessitate future orthodontic-orthognathic treatments after growth (20). Once the desired level of expansion is achieved, the maxilla is drawn forward with a force ranging from 300-600gF on each side, directed roughly 30 ° downward and forward. This approach encourages a positive reaction from the upper jaw sutures during expansion and forward movement, addressing any imbalances between CO and CR. Consequently, it improves the patient's facial appearance, enhancing their self-confidence. Effective for mild to moderateClass III malocclusions with standard/reduced vertical dimensions, the nighttime facemask, paired with intermaxillary elastics, offers near-continuous Class III traction. Early facemask use benefits teeth and skeletal structure, reducing future surgery risks, especially in children under ten with specific Class III traits (21-26). Baccetti et al. has shown that treatment, particularly in children with only deciduous teeth at around five years old, results in more favorable skeletal outcomes. These include notably smaller increases in the total length of the mandible (Co-Pg) as opposed to the more pronounced protrusion of the maxillary dentoalveolar when treatment is carried out during the mixed dentition stage, which is typically around eight years of age (27, 28). There is no evidence indicating that adding RPE to a protraction facemask routine, aiming to relax the surrounding upper jaw sutures and enhance the forward shift of the upper jaw, enhances maxillary forward movement. Hence, this method should be specifically used for patients displaying a narrowed upper jaw (29, 30). For very young children, around four to five years old, a simple method to correct anterior crossbite involves attaching cleats or buttons to the top second deciduous molars and bottom deciduous canines for consistent use of Class III elastics. This is both effective and cost-efficient. However, with the advent of skeletal anchorage, there's been a trend toward using bone-supported techniques for moving the upper jaw forward with a facemask, rather than methods that rely on the teeth. Research shows that when the facemask is anchored to the teeth, there is more forward tilting of the upper front teeth, better correction of the space between upper and lower front teeth, and modification of the back teeth alignment. On the other hand, facemasks anchored to the bone produce better skeletal outcomes and fewer undesired changes to the teeth. This technique causes less downward shift of point A, a lesser rise in the angle of the lower jaw, and a more upright growth direction for the upper front teeth. It is especially fitting for Class III patterns with excessive vertical growth (2). Nienkemper and his team proposed using Class III elastics attached to a mentoplate as a method to avoid the necessity of external traction (31-33).
Class II malocclusion
While evidence supports early treatment benefits for Class II malocclusions, there is a disparity between scientific knowledge and clinical practice. Research suggests that two-phase treatments are not markedly better than a single intervention during puberty. These studies also reveal that the two-phase method does not significantly simplify the second phase, whether in terms of tooth extractions, the need for jaw surgery, or the length of the second phase of treatment. Yet, many professionals still advocate for this two-phase approach (6, 34-37). The only justifications for recommending early intervention in Class II treatment are a marginally increased chance of injury to the upper front teeth and the possible psychological concerns due to bullying (2). If Class II malocclusion coexists with transverse or vertical problems, early intervention is advised. Simple yet effective initial treatments are preferred to maintain patient motivation and minimize financial strain. The puberty growth phase remains pivotal for Class II corrections, saving resources for potential second-phase treatments.
Open bite
Effectively treating open bites in the early orthodontic stages largely relies on pinpointing their origin (2). Effective open bite treatment can be achieved if it is due to maxillary constriction or dental behaviors like tongue thrusting. Yet, if it is due to a dominant dolichofacial growth pattern, early treatments like RPE might not control the maxilla's growth direction. Ensuring normal respiratory function is essential when starting treatment. Myofunctional therapy, with devices to adjust tongue position, is recommended. Despite the treatment, open bite solutions have unpredictable long-term success. Future treatments using skeletal anchorage devices may offer better control and consistent outcomes for open bite cases (38).
Arch length discrepancy
In orthodontics, it is common for professionals to come across significant inherited discrepancies between tooth size and arch length from a young age. The main decision is whether to adjust the foundational bone or the shape of the arch, using methods like expansion, moving teeth backwards, or tilting them forward, or to choose serial extraction. If a lingual crossbite is present due to the upper jaw being too narrow, expanding the upper jaw is the primary solution, delaying the extraction decision until after the expansion. Without a crossbite, deciding between expanding or extracting depends on the growth pattern and face type of the patient. For patients with upright or backwards-slanting lower front teeth, and where a broad overview X-ray shows a promising space for teeth to emerge without signs of the lower second molar getting stuck, using a lip bumper to create space in the lower jaw may be appropriate. However, the overall front-back and up-down relationships of the bite and jawbone, along with the patient's facial soft tissues, are vital to the final treatment choice.
Besides the clear signs like a major Class II malocclusion where the upper front teeth lean outwards or open bites associated with a face that grows too much vertically and lips that do not close properly, there are other factors suggesting extraction might be the right choice. These include early loss of one or more side teeth causing the center line of the teeth to shift, gingival recession on a protruding lower tooth, proclination of the upper or lower teeth, abnormal growth patterns of the first permanent molars linked to early loss of the second deciduous molars, clear outward positioning of both jaws, deep bends in the arch of the jaw, the upper big teeth lining up vertically in the back part of the upper jaw, and the lower second molar getting stuck. In essence, a comprehensive evaluation that considers both physical features and diagnostic signs is crucial in determining the best treatment path (2).
Conclusion
The review emphasizes the significance of early intervention in orthodontic issues, ideally between ages 6 and 10, to prevent complicated treatments in later stages. Early orthodontic interventions are essential for diagnosing, preventing, and managing potential skeletal and dental challenges in children. Understanding the specifics of each malocclusion or discrepancy, along with being receptive to innovative treatment methods, enables orthodontists to provide optimal care. Thus, both clinicians and patients benefit from an informed approach based on rigorous research and continuous adaptation to evolving best practices.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.