Volume 3, Issue 10
October 2023
Endodontic Treatment in Elderly Patients: Success Rates, Satisfaction, and Outcomes
Ainaa Alsharif, Turki Alhabib, Aysha Alwusayfir, Hussain Alyami, Bassam Alshammari, Mohammed Aloufi, Noor Alotaibi, Shahad Alharthi, Shahd Aldaham, May Alotaibi, Faris Alharbi
DOI: http://dx.doi.org/10.52533/JOHS.2023.31005
Keywords: endodontic therapy, elderly patients, success rates, patient satisfaction, clinical outcomes, age-related changes
As the global population continues to age, addressing the nuances of healthcare for elderly individuals becomes increasingly crucial. Within the realm of dentistry, endodontic treatment, or root canal therapy, holds significant importance as it preserves natural teeth, alleviates pain, and enhances oral health. The success rates of endodontic therapy in the elderly are influenced by factors such as dentist experience, patient compliance, and case complexity. Patient satisfaction in this demographic is multifaceted, encompassing pain management, clinical success, communication, and emotional well-being. Clinical outcomes profoundly impact overall oral health and quality of life, including pain relief, infection control, and the preservation of natural dentition. While age-related changes and medical comorbidities introduce challenges, they do not inherently hinder treatment success. This review emphasizes that endodontic therapy remains a viable and effective option for elderly patients, with individualized care plans and patient-centered approaches being paramount. As the elderly population continues to grow, further research and refined practices are essential to meet their evolving dental needs effectively. Dental professionals must remain attuned to the unique challenges and priorities of elderly individuals to deliver high-quality endodontic care.
Introduction
As the world's population continues to age, there is a growing imperative to understand and address the intricacies of healthcare for elderly individuals. Within the realm of dentistry, endodontic treatment stands as a pivotal procedure that not only preserves natural dentition but also alleviates pain and enhances oral health. However, the elderly population represents a unique demographic in which endodontic care warrants distinct consideration. This comprehensive review embarks on an exploration of the multifaceted aspects surrounding endodontic treatment for elderly patients. With a focus on success rates, patient satisfaction, and clinical outcomes, we aim to shed light on the complex interplay of age-related physiological changes, medical comorbidities, and the evolving landscape of dental care.
The success of endodontic treatment in elderly patients is a critical metric by which its efficacy is gauged. These rates exhibit variability influenced by a multitude of factors (1). Among these, age-related changes, such as diminished pulp vascularity and the formation of secondary dentin, may introduce complexities into endodontic procedures but do not inherently jeopardize treatment outcomes. Moreover, the presence of medical comorbidities, which are prevalent in elderly populations, raises pertinent questions about their potential influence on treatment efficacy (2). Current research on this aspect, however, presents a mixed landscape without a conclusive consensus on the magnitude of their impact.
Patient satisfaction occupies a pivotal position in the realm of healthcare quality assessment, assuming even greater importance in the context of endodontic treatment for elderly individuals. The satisfaction of elderly patients with endodontic treatment is a multifaceted construct, influenced by various intricate factors (3). Effective pain management, a cornerstone of patient satisfaction, assumes paramount significance in elderly patients due to their heightened pain sensitivity (4). Minimizing pain during and after endodontic procedures significantly enhances the overall patient experience. In addition to pain management, clinical success represents a central determinant of patient satisfaction. This entails not only the relief of pain but also the restoration of oral function, both of which assume paramount importance in elderly individuals (5). Radiographic evidence confirming proper healing further bolsters satisfaction levels (6). Furthermore, clear and comprehensive communication about the procedure, chair comfort, treatment duration, and clinic accessibility are factors that can significantly impact satisfaction levels in the elderly population. Emotional and psychological well-being also play a pivotal role, with dental anxiety, fear of pain, and prior negative experiences influencing patient expectations and, consequently, satisfaction levels (7).
The clinical outcomes associated with endodontic treatment in elderly patients are multifaceted and profoundly impact their overall oral health and quality of life. The primary objective of endodontic treatment—pain relief—assumes paramount significance in the elderly (8). Effective pain management enhances not only oral comfort but also the patient's overall quality of life. Furthermore, endodontic therapy effectively controls and eliminates infection within the tooth, preventing systemic spread (9). Radiographic evidence of the resolution of periapical lesions and the absence of post-operative complications substantiates treatment success (10). Moreover, maintaining natural dentition is critical for elderly patients. Successful endodontic therapy empowers them to sustain functional dentition, which directly impacts chewing efficiency and overall nutrition (11). The preservation of natural dentition is intricately tied to patient satisfaction and overall well-being. This contributes significantly to an improved overall experience and treatment outcome.
Methodology
This study is based on a comprehensive literature search conducted on September 12, 2023, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed success rates, satisfaction, and outcomes of endodontic treatment in elderly patients. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Survival and success of endodontic therapy in elderly patients
Before delving into the success of endodontic therapy in older patients, it is essential to understand the broader epidemiological context of aging and dental health. The aging demographic shift is a well-documented global phenomenon. According to the World Health Organization, the proportion of individuals aged 60 and over is expected to nearly double by 2050, reaching approximately 22% of the global population (12). This demographic shift has profound implications for healthcare, including dental care.
Research in this field has shown that endodontic therapy can indeed be successful in older patients, with success typically defined by criteria such as pain relief, the absence of swelling or infection, and the preservation of the treated tooth (13). Smith et al. conducted an investigation where they studied the factors influencing the success of conventional endodontic therapy and found the success rates of the elderly (≥60 years) to be one of the highest among all age groups at 88.64% (14). Several factors can influence these success rates. For instance, the skill and expertise of the dentist performing the procedure play a crucial role, as experienced endodontists tend to have higher success rates (15). Patient compliance with post-treatment instructions is vital; patients must adhere to proper oral hygiene practices and attend follow-up appointments for the best outcomes (16). Moreover, the complexity of the case, including the extent of infection or damage, can impact success rates, as some cases may inherently be more challenging than others (1). Therefore, establishing and adhering to rigorous follow-up protocols is essential to ensure that any potential issues are promptly identified and addressed.
Age-related physiological changes in the oral cavity, such as alterations in dental pulp, dentin, and periodontal tissues, can have epidemiological implications for endodontic outcomes in older patients (Figure 1) (17). These changes may contribute to a higher prevalence of dental pathologies in this demographic, necessitating a greater need for endodontic therapy. Further, older individuals often present with comorbidities, which can have significant epidemiological implications for dental health. Chronic conditions like diabetes, hypertension, cardiovascular disease, and autoimmune disorders are more prevalent in this age group (2). Epidemiological studies can help identify the relationships between these comorbidities, the medications used to manage them, and the success rates of endodontic therapy.
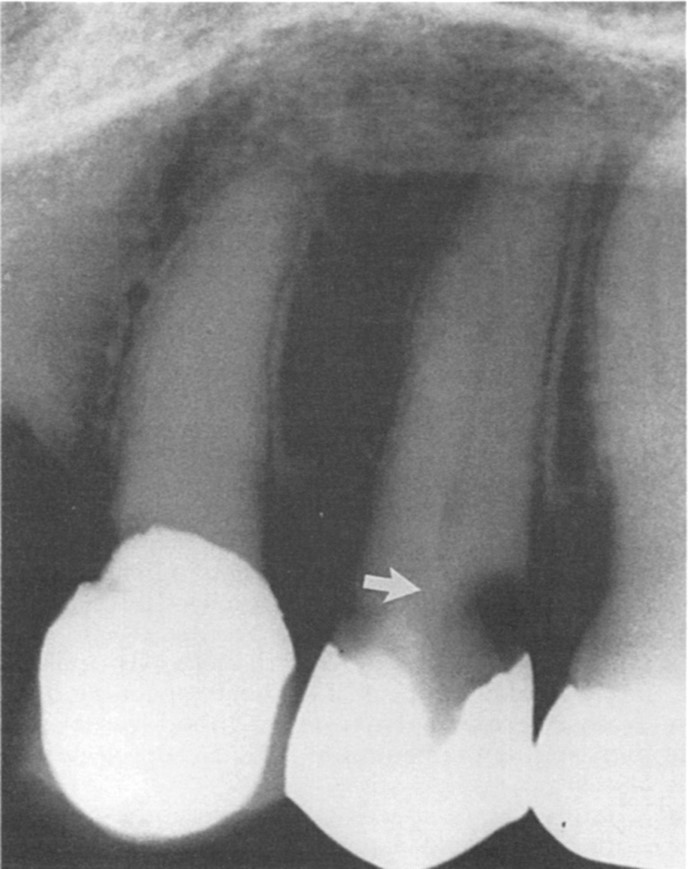
Figure 1: The interaction of restorations, caries, and time has led to the development of dentin formation. In the first premolar, calcific metamorphosis is evident, with a notably small pulp space remaining. In the second premolar, dentin formation (indicated b).
Modern endodontic techniques and materials have significantly improved treatment outcomes (18). Innovations in diagnostic tools and imaging technology enable more accurate treatment planning. Biocompatible materials, such as gutta-percha and resin-based sealers, enhance the longevity and success of root canal treatments. Moreover, advances in instrumentation, like nickel-titanium rotary files, facilitate more efficient and precise procedures, reducing the risk of procedural errors (9).
Understanding these factors that shape the success of endodontic therapy in older patients is crucial. It allows dental professionals to tailor treatment plans to meet the specific needs of this demographic. Furthermore, successful endodontic therapy can significantly enhance the overall quality of life for older individuals by preserving their natural teeth.
Patient satisfaction with endodontic therapy in elderly patients
Elderly patients place significant value on the retention of their teeth through non-surgical root canal treatment (RCT) (9). However, it is essential to acknowledge that the priorities of elderly patients often diverge from those of their younger counterparts. This distinction can significantly influence treatment planning. For elderly patients, the primary goal of treatment tends to be guided by short-term objectives and asymptomatic functionality rather than aesthetics and long-term stability (20). It is worth noting that despite their positive attitudes towards nonsurgical RCT, some elderly patients may decline dental implants due to concerns related to fear or cost (21, 22).
The appreciation of non-surgical RCT among elderly patients stems from various factors, including pain and swelling relief, improved chewing and digestion, enhanced esthetic appearance, boosted self-esteem, and the preservation of natural teeth. Furthermore, non-surgical RCT contributes to the maintenance of dignity, speech, and support for existing prostheses (21). However, it's essential to recognize that not all elderly patients share uniformly positive opinions regarding non-surgical RCT. Some express concerns about the extended duration of dental visits, the need to keep the mouth open for an extended period, dryness of the mouth due to prolonged visits, and the inconvenience associated with rubber dam isolation (21).Several reasons contribute to the avoidance of dental treatment by elderly individuals. High treatment costs, fear of pain, limited knowledge or understanding of dental care requirements, reduced cognitive abilities, decreased tolerance for treatment steps, and limited mobility are among the primary factors influencing their decisions (23).
Interestingly, endodontic treatment significantly improves the quality of life (QOL) among elderly patients, as indicated in a review by Neelakantan et al. (24). Patients experiencing pain reported a significantly lower QOL in most domains, except for functional limitation, highlighting the substantial impact of pain on an individual's QOL. Contrary to expectations, elderly patients in the study reported a significantly better oral health related QOL (OHRQOL), challenging assumptions that age-related oral diseases would lead to poorer OHRQOL. These findings align with several studies demonstrating a reverse age association with OHIP-14 scores (25).
It is noteworthy that older individuals may perceive pain differently than their younger counterparts due to previous experiences and may consider dental problems minor compared to systemic diseases. Additionally, the need for RCT may align more with the expectations of the elderly, who may view it as an opportunity to maintain good oral health and retain natural dentition, in contrast to younger patients, who might perceive it as an unexpected necessity (26).
Furthermore, the impact of endodontic problems on QOL varies depending on the tooth's location. Issues in the anterior and premolar teeth tend to have a more substantial impact on QOL, likely due to aesthetic concerns associated with these teeth. Additionally, a noteworthy gender difference in QOL exists, with women requiring RCT reporting significantly poorer QOL than men. Thisdiscrepancy may be attributed to women's heightened awareness of appearance and health, potentially leading to a more pronounced effect of endodontic problems on their QOL. Moreover, women may experience more anxiety related to endodontic treatment, contributing to their poorer QOL in this context (27).
Clinical outcomes of endodontic therapy in elderly patients
Achieving predictable and effective root canal treatment (RCT) hinges on several critical factors (Table 1). Access to the infected pulp space is paramount, but challenges may arise when dealing with limited mouth opening, unfavorable tooth alignment, over-eruption, intolerance of lengthy procedures, or pulp space calcification. In cases where these complexities are present, it may not be feasible to salvage the tooth, necessitating careful treatment planning.
At the core of RCT is the fundamental goal of preventing or healing apical periodontitis. Whether evaluating a tooth with a large and patent pulp space or one with a canal system barely visible on radiographs, the biological objectives of treatment remain consistent. Pulp breakdown and the development of apical periodontitis occur due to the infiltration of microorganisms into the pulp space (28, 29). It's worth noting that microorganisms typically do not spread in large numbers from the canal system to invade peri-radicular tissues. Instead, a gradual release of microbial toxins through apical and lateral portals triggers a host response aimed at containing the disease, which can result in bony rarefaction (30). Consequently, RCT primarily aims to eliminate microbial infection from the canal space and prevent its recurrence. When executed before apical periodontitis fully develops, RCT can prevent lesion formation. In cases with established apical periodontitis, the elimination of root canal infection creates the conditions necessary for periapical tissues to initiate self-restoration to health.
Expectations regarding RCT outcomes are typically high, with many reporting success rates exceeding 90%, although general practice experiences may yield somewhat lower rates (31). A pertinent question arises concerning the role of host defenses in these outcomes, particularly whether elderly patients may anticipate less favorable results compared to their younger counterparts. Current epidemiological data have not revealed age-related variations (32, 33). It is widely acknowledged that RCT's predictability remains consistent between young and elderly patients, provided that effective management of pulp canal infection is ensured. Nevertheless, challenges related to infection control may arise, especially when dealing with damaged, biologically aged teeth.
The primary objectives of RCT encompass the removal of intracanal infection and the prevention of reinfection by creating an environment conducive to the healing of apical periodontitis (20). While an in vitro study suggested that disinfecting older dentin is more challenging than younger dentin (34), a systematic review found no substantial influence of age on the initial RCT success rate (35). Hence, patient age alone should not be regarded as a prognostic factor. Cases involving vital pulps typically exhibit a very favorable prognosis, although meticulous assessment of medical conditions and systemic diseases is crucial (36). Notably, cases with preoperative periapical lesions tend to have poorer prognoses, potentially with systemic diseases playing a more substantial role (19). Although periradicular tissues heal readily in both elderly and young patients, relying solely on a 6-month recall period for radiographic evaluation may prove inadequate. Studies suggesting differences in success among age groups should consider the smaller sample sizes in older patient groups and the local factors that can complicate treatment (37).
|
Table 1. A concise overview of the key points concerning endodontic therapy outcomes in geriatric patients, highlighting success rates, patient satisfaction factors, clinical outcomes, challenges related to aging, and the importance of personalized care. |
|
|
Key Aspect |
Summary |
|
Success Rates |
- Success rates range from 75% to 95% in geriatric patients. |
|
- Variability influenced by dentist experience and case complexity. |
|
|
Patient Satisfaction |
- Multifaceted, influenced by factors like pain management, clinical success, and communication. |
|
- Pain relief and functional restoration are paramount for satisfaction. |
|
|
Clinical Outcomes |
- Impact overall oral health, including pain relief, infection control, and preservation of natural dentition. |
|
- Maintaining natural dentition enhances chewing efficiency and nutrition. |
|
|
Age-Related Challenges |
- Age-related physiological changes may introduce complexities. |
|
- Medical comorbidities can impact treatment planning and efficacy. |
|
|
Individualized Care |
- Tailoring treatment plans to address unique needs of elderly patients is crucial. |
|
- Patient-centered approaches contribute to improved outcomes. |
|
Conclusion
Endodontic treatment in elderly patients has shown promising success rates, with factors such as dentist expertise, patient compliance, and case complexity playing crucial roles. Patient satisfaction in the elderly population hinges on effective pain management, successful treatment outcomes, clear communication, and emotional well-being. Clinical outcomes of endodontic therapy in older individuals significantly impact their quality of life, including pain relief, infection control, and the preservation of natural dentition. While age-related changes and medical comorbidities present unique challenges, they do not inherently hinder treatment success. As the elderly population continues to grow, it is vital to tailor endodontic care to meet their specific needs.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
