Volume 3, Issue 10
October 2023
Medical and Surgical Approaches to Obstructive Sleep Apnea
Ashraf Abduljabbar, Roaa Alkanderi
DOI: http://dx.doi.org/10.52533/JOHS.2023.31002
Keywords: Obstructive Sleep Apnea, OSA, CPAP therapy, oral appliances, Maxillomandibular Advancement, Uvulopalatopharyngoplasty, Radiofrequency Ablation
Obstructive Sleep Apnea (OSA) is a prevalent sleep disorder characterized by recurrent upper airway obstructions during sleep, leading to disrupted sleep patterns and potential health risks. This comprehensive review explores various medical and surgical modalities for the treatment of OSA. Continuous Positive Airway Pressure therapy is the standard treatment for moderate to severe cases, but long-term compliance remains a challenge. Oral appliances and novel technologies, such as Oral Pressure Therapy and Upper Airway Stimulation offer non-invasive alternatives. Surgical interventions, like Maxillomandibular Advancement, Uvulopalatopharyngoplasty, Laser-Assisted Uvulopalatoplasty, Radiofrequency Ablation, Genioglossus Muscle Advancement and Tracheostomy, provide tailored solutions for persistent OSA. Maxillomandibular Advancement in particular, has shown significant efficacy in reducing the Apnea-Hypopnea Index. Uvulopalatopharyngoplasty, while widely used, has variable success rates, often necessitating additional therapies. Laser-Assisted Uvulopalatoplasty and Radiofrequency Ablation are minimally invasive options but require careful patient selection. This review highlights the importance of individualized treatment plans, considering OSA severity, patient compliance, and comorbidities. Advances in non-invasive and minimally invasive treatments have expanded options, enhanced patient quality of life and reducing health risks. Tracheostomy, though less common today, remains valuable in specific cases. A multidimensional approach to OSA management is crucial, tailoring treatments to individual patient needs and optimizing overall well-being.
Introduction
OSA is a prevalent sleep disorder characterized by recurrent episodes of partial or complete upper airway obstruction during sleep, leading to disrupted breathing and oxygen desaturation (1). The clinical spectrum of OSA encompasses a constellation of symptoms, including persistent snoring, excessive daytime sleepiness, nocturnal breathing cessations, morning headaches, irritability, cognitive deficits, and associated depressive symptoms (2-5). Beyond these immediate effects, OSA is intricately linked to a spectrum of comorbidities that extend its impact to cardiovascular and cerebrovascular diseases, metabolic disorders like diabetes, obesity (6), hepatic impairments, compromised cognitive function, strained interpersonal relationships, diminished quality of life, and heightened mortality risk (7-9).
Globally, an estimated 936 million individuals suffer from mild to severe OSA, with 425 million in the moderate to severe category, all within the age bracket of 30 to 69 years (10). In North America, OSA's prevalence spans between 15% to 30% in males and 10% to 15% in females, employing a broader diagnostic criterion rooted in an apnea-hypopnea index (AHI) exceeding five events per hour of sleep (11, 12). Stringent criteria, such as AHI ≥5 events per hour with accompanying symptoms or AHI ≥15 events per hour, reduce the prevalence to approximately 15% in males and 5% in females (11-13).
Fortunately, OSA is amenable to treatment, and early medical evaluation and intervention offer an avenue to alleviate symptoms and avert potential complications, thereby enhancing overall well-being. A spectrum of comorbidities shadow OSA, underscoring the importance of effective therapeutic strategies. These interventions encompass lifestyle modifications, weight management, exercise regimens, positive airway pressure therapy, oral appliances designed to advance the mandible during sleep, and surgical interventions targeting the pharyngeal soft tissues or facial skeleton to augment the upper airway dimensions (14).
The primary treatment for moderate-to-severe OSA is Continuous Positive Airway Pressure (CPAP), recognized as the gold standard due to its efficacy (15). However, long-term tolerance issues affect nearly half of OSA patients, prompting the exploration of alternative non-invasive interventions. Among these alternatives, oral appliances and weight reduction are viable options, though they have limitations in achieving an AHI of less than 5 (16). In cases of persistent OSA resistant to CPAP therapy, surgical modifications offer tailored solutions. Surgical techniques include Maxillomandibular Advancement (MMA), Uvulopalatopharyngoplasty (UPPP), tonsillectomy, and adenotonsillectomy (16).
Despite the spectrum of OSA treatments, each approach has inherent limitations and potential side effects. This review aims to provide a concise overview of common OSA treatment modalities, offering insights into their clinical indications in adult patients, and seeks to provide an updated assessment of both medical and surgical OSA management approaches.
Methodology
This review employed a systematic and multidimensional approach to synthesize relevant scientific literature pertaining to OSA and its management. The initial phase involved exhaustive searches across reputable academic databases such as MEDLINE, Google Scholar, and Science Direct, with no publication date restrictions. The review encompasses a wide spectrum of topics, beginning with an exploration of non-invasive medical treatments including Continuous Positive Airway Pressure therapy and oral appliances and then proceeding to surgical interventions for OSA. Additionally, randomized controlled trials, meta-analyses, and prospective studies were scrutinized to present the most current and credible findings.
Discussion
This review evaluated the evidence from the literature for management strategies employed for the treatment of OSA. These management strategies were segregated into two types of approaches of medical and surgical interventions which are explained in detail further below.
Medical Management of OSA
As the recognition of OSA and its far-reaching implications for health and well-being has expanded, a wide range of medical interventions has emerged to address this complex sleep disorder. This comprehensive overview delves into the diverse landscape of medical approaches for managing OSA. It encompasses non-invasive therapies, such as continuous positive airway pressure CPAP, oral appliance therapy, and various innovative technologies, all designed to alleviate the adverse effects of OSA.
Continuous Positive Airway Pressure (CPAP) Therapy
CPAP therapy is considered the standard treatment for moderate to severe OSA. It entails the use of a CPAP machine, which delivers a continuous stream of pressurized air through a mask worn over the nose, mouth, or both (Figure 1). The primary objective of CPAP therapy is to maintain an open upper airway during sleep, preventing recurrent airway obstructions characteristic of OSA.
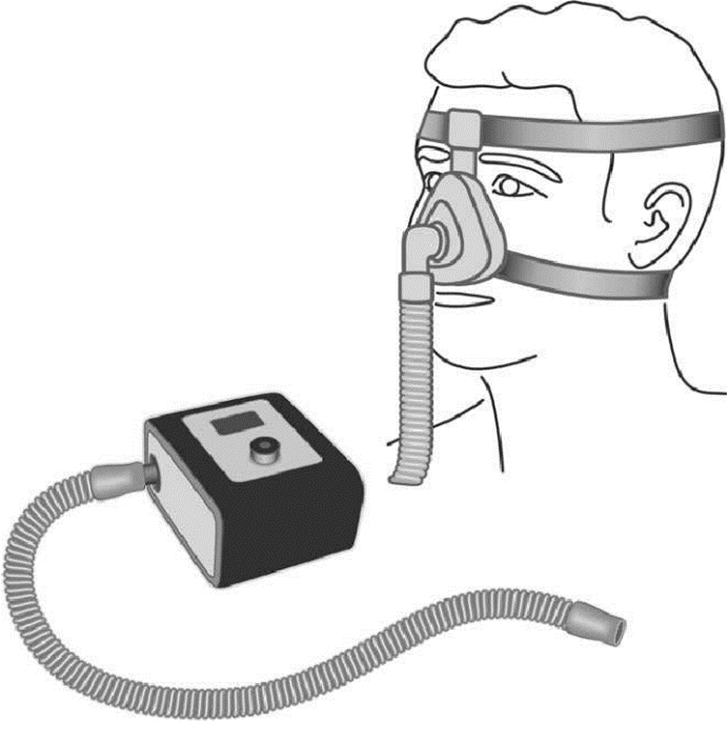
Figure 1: Continuous positive airway pressure (CPAP) circuit. A blower device is connected to an interface (in this case a conventional nasal mask) via a tube. The interface is attached to the external nose using headgear that consists of two adjustable straps.
Specifically recommended for patients with an AHI exceeding 15 per hour or those with lower AHI but experiencing excessive daytime sleepiness (EDS), CPAP has a well-established track record for reducing OSA severity, sleepiness, blood pressure, and accident risk while enhancing sleep-related quality of life (17). Individualized therapeutic pressure settings are determined through manual or home titration using automatic CPAP devices, with the importance of well-fitting masks, particularly nasal masks, underscored for effective treatment.
Debates surround the choice between automatic CPAP and fixed-pressure CPAP devices. While both types exhibit similar air leak rates, some studies suggest potential advantages of fixed-pressure CPAP in terms of blood pressure reduction and renal function preservation (19). Cliffold et al (20) reported that patients who required higher fixed CPAP pressures tended to use autotitrating CPAP more frequently and reported experiencing greater benefits from this adaptive therapy approach.
However, despite its efficacy in alleviating OSA symptoms, recent research has raised concerns about CPAP's ability to address associated health issues, such as insulin resistance and cardiovascular disease. Long-term trials, including the Sleep Apnoea Cardiovascular Endpoints (SAVE) and Randomized Intervention with CPAP in coronary artery disease (CAD) and OSA (RICCADSA) trials, have failed to demonstrate significant benefits in preventing cardiovascular complications or mortality, mainly due to low CPAP compliance (21, 22). Patients often use the therapy for less than 4 hours per night, reflecting real-world challenges in adherence. Moreover, CPAP's potential to prevent comorbidities like diabetes and cognitive dysfunction is limited due to non-compliance (23-25). Adherence rates tend to be higher in patients with EDS and significant daytime limitations, while those with insomnia, females, mildly symptomatic individuals, or comorbidities may have lower success rates. The impact of health and safety risk behaviors on CPAP discontinuation cannot be ignored.
For patients struggling with CPAP tolerance, bilevel ventilation and telemedicine have emerged as promising alternatives. Automatic bilevel ventilation may benefit patients with poor CPAP tolerance or those with overlapping OSA-COPD syndrome. Telemedicine, which has proven cost-effective, especially during the COVID-19 pandemic, may potentially set a new standard of care for managing OSA patients on CPAP (26-28).
Oral Appliances
Oral appliances, designed to reposition the mandible and stabilize the upper airway, provide a non-invasive alternative for managing OSA. Several earlier studies have lauded oral appliances for their cost-effectiveness, relative comfort, and ease of use, which can enhance patient compliance (29). Oral appliances are commonly constructed from thermoplastic materials, and among them, mandibular repositioning devices or mandibular advancement devices (MADs) stand out as the most frequently employed type of oral appliance therapy for managing OSA (30), The MAD's mechanism of action is typically attributed to its ability to enlarge the cross-sectional dimensions of the upper airway by anteriorly displacing the mandible and the attached tongue, ultimately leading to improved upper airway patency Figure 2 (31).
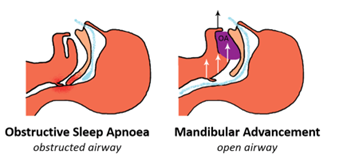
Figure 2: Mandibular advancement device with and without (34)
A study by de Britto Teixeira et al. evaluating mandibular advancement devices (MADs) highlights their potential efficacy, particularly for mild to medium-to-moderate OSA cases (32). These results highlight that oral appliances, when appropriately selected and monitored, can serve as an effective alternative for certain OSA patients, addressing the pressing need for diverse treatment options in the OSA management continuum. However, it's crucial to note that another randomized controlled trial reported no clinically meaningful difference in treatment outcomes between MADs and nasal continuous positive airway pressure (nCPAP) for this patient subgroup (33).
Another Novel Technologies
Other non-surgical or minimally invasive medical management options for OSA include Oral Pressure Therapy (OPT), Nasal Expiratory Positive Airway Pressure (EPAP), and Upper Airway Stimulation. OPT creates negative oral cavity pressure during sleep, preventing throat tissue collapse without surgery. OPT circumferentially increases the size of the retropalatal and retrolingual airways by pulling forward the soft palate and the tongue (35). EPAP is designed as a disposable, single-night-use solution. It comprises one-way valves or resistors that are affixed to the nasal passages using a hypoallergenic adhesive. These valves are engineered to permit easy airflow during inhalation while providing substantial resistance during exhalation, resulting in the generation of positive pressure throughout the exhalation phase. This positive pressure effectively acts as a support mechanism, preventing the upper airway from collapsing during subsequent inhalations. Extensive, extended-term research has indicated the device's effectiveness in treating individuals with various degrees of OSA (1, 36). Upper Airway Stimulation, an FDA-approved option for carefully assessed patients with moderate to severe OSA and a Body Mass Index (BMI) under a certain threshold (under 32), offers an alternative treatment approach (37, 38).
Surgical Interventions
Surgical treatments aim to enlarge and stabilize the upper airway and may provide an option for patients in whom conventional medical treatment has failed (39). Surgical approaches to OSA management, including maxillomandibular advancement (MMA), pharyngeal surgeries such as uvulopharyngopalatoplasty (UPPP), laser assisted uvulopalatoplasty (LAUP), and radiofrequency ablation (RFA), as well as multi-level and multi-phased procedures.
Maxillomandibular advancement (MMA)
Maxillomandibular advancement (MMA) is a surgical technique aimed at repositioning the upper and lower jaws forward to enlarge the upper airway and reduce its collapsibility during sleep (40, 41). MMA stands as a clinically proven and safe long-term treatment option for the majority of patients dealing with moderate-to-severe OSA. This assertion is substantiated by substantial improvements in key parameters, including the AHI, diastolic blood pressure, and self-reported sleepiness, accompanied by significant enhancements in the quality of life (QOL) (42). Figure 3 illustratively shows before and after the MMA surgical procedure (43).
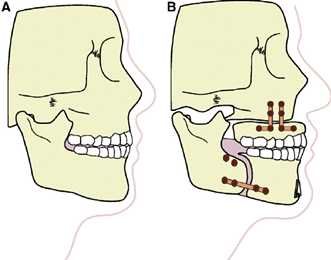
Figure 3: Before (A) and after (B) maxillomandibular advancement surgery (43)
The efficacy of MMA is particularly noteworthy, as it consistently achieves a remarkable reduction in AHI from an average of 64/h to 11/h. Moreover, MMA demonstrates impressive surgical success and cure rates, with 86% and 43% of patients achieving AHI levels below 5/h, respectively (44). Consequently, the precise identification of potential responders and non-responders to MMA before surgery is of paramount clinical significance (45). However, the identification of suitable candidates for MMA presents a significant challenge, given that factors such as cardiovascular disease (CVD), central apnea index (CAI), and anatomical characteristics, such as a larger soft palate and tongue size, may exert influence on surgical outcomes (45, 46). Numerous factors, including patient demographics, polysomnographic data, and surgical variables, have been investigated as potential predictors of a positive surgical outcome. These variables encompass younger age, lower baseline weight, lower initial AHI, and a more substantial maxillary advancement (47)
Uvulopalatopharyngoplasty (UPPP)
Uvulopalatopharyngoplasty (UPPP) is currently the most prevalent surgical intervention employed for adults presenting with mild to moderate OSA. This procedure aims to enhance the oropharyngeal airspace by excising specific throat tissues, which may include the uvula, soft palate, and tonsils. It typically encompasses a series of surgical steps, including tonsillectomy (if not previously performed), adjustment and reorientation of the posterior and anterior tonsillar pillars, and the excision of the uvula and posterior palate. While UPPP is comparatively less invasive and generally well-tolerated in comparison to other surgical modalities, its effectiveness, as defined by various criteria primarily rooted in respiratory parameters, is notable, albeit modest, with response rates often hovering around 50% in short-term follow-up. It is worth noting that UPPP is frequently complemented by additional nasopharyngeal or oropharyngeal procedures. The pictorial representation of the process of UPPP is shown in Figure 4 (48).
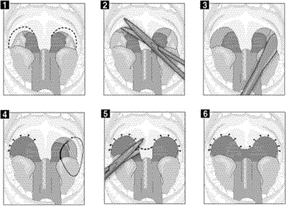
Figure 4: Process of perming UPPP. 1. Begin by marking a distinct incision line on the sides of the uvula. 2. Proceed with the removal of a small portion (approximately 2-3 mm) of the front part of the tonsillar pillar and the mucous membrane that connects them.
The reported success rates of UPPP as an OSA treatment span a wide range, falling between 16% and 83%, contingent on the chosen criteria for defining a favorable outcome (49, 50). Some investigators stipulate surgical success or cure post-UPPP as a 50% reduction in the AHI, while others couple this criterion with an absolute AHI threshold of 20 or less (51-54). Emerging scientific evidence suggests that, for comprehensive improvements in healthcare-related outcomes, particularly in conditions such as hypertension (HTN), it is imperative to achieve an Apnea-Hypopnea Index (AHI) of less than 5. Notably, even mild sleep apnea elevates the risk of developing HTN (55).
A study by Khan et al. found that irrespective of changes in BMI, UPPP achieved an AHI of 5 or less in 24% of patients, and an AHI of 10 or less in 33% of individuals with OSA who underwent polysomnography six months prior and post-surgery. In cases where residual OSA persisted, and CPAP therapy was initiated, the required pressure setting decreased by an average of 1.4 cm H2O (56).
Collectively, insights gleaned from a series of investigations assessing the efficacy of UPPP in OSA management underscore its value as a therapeutic intervention. Li et al.'s (57) retrospective review, for instance, documented a substantial reduction in the AHI post-UPPP, with an overall success rate of 78%, particularly when employing an anatomy-based staging system. Browaldh et al.'s (58) randomized controlled trial reinforced UPPP's effectiveness, demonstrating a substantial mean AHI reduction of 60%, albeit with limitations related to patient BMI. Sommer et al.'s (59) trial further supported UPPP's effectiveness in reducing AHI and daytime sleepiness, with high patient satisfaction, although the shorter follow-up duration impedes long-term outcome assessment. Choi et al.'s (60) meta-analysis identified predictors of success, notably highlighting the significance of Friedman staging and mandibular plane to hyoid distance. These findings collectively contribute valuable insights into the clinical utility of UPPP in managing OSA and underscore the need for tailored treatment approaches based on individual patient characteristics.
Laser assisted uvulopalatoplasty (LAUP)
LAUP is a minimally invasive outpatient procedure designed to treat OSA. Unlike other surgical options, LAUP doesn't require sutures and has evolved over time as an effective treatment for snoring and OSA. It aims to expand the airway in the oropharyngeal region by using lasers (CO2 or Nd:YAG) to remove and tighten tissues. Scar tissue formation is crucial for its success. The procedure involves creating incisions in the soft palate, sometimes including uvula removal (61). Illustrative representation of LAUP is shown in Figure 5 (61).
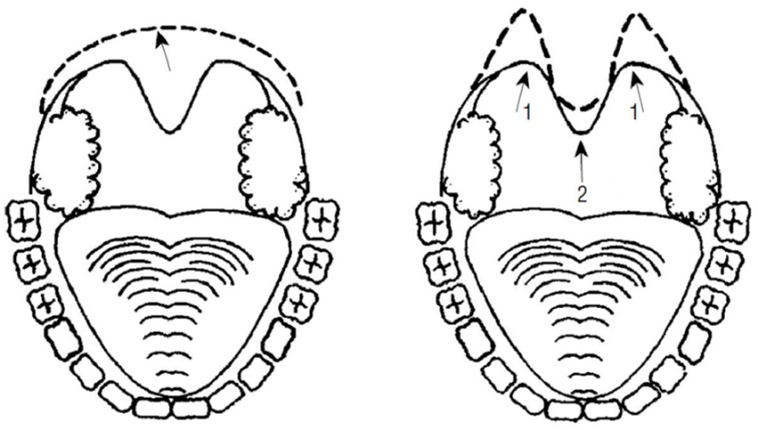
Figure 5: Illustrative representation of LAUP (61)
Göktas, Ö et al.'s study on LAUP for OSA highlights that LAUP can yield a reduction in the AHI score comparable to other mucosal resection methods. However, their research also underscores that the effectiveness of LAUP diminishes over time, and there is a notable risk of increased AHI scores following the procedure (61). In another investigation by Ferguson et al., 46 snoring patients with an AHI ranging from 10 to 27 were randomly divided into two groups: one underwent LAUP, while the other received no treatment and was monitored for 7 months. Actively treated patients exhibited reduced AHI, decreased snoring intensity, and lower snoring frequency, whereas non-treated patients experienced minimal changes in these parameters (62). In contrast, Larossa et al. (63) conducted a randomized trial involving 28 snoring patients with an AHI < 30, assigning them to either LAUP or sham surgery, and monitored them for 3 months. Their findings revealed no significant differences in the assessed outcomes between the two groups. Currently, LAUP isn't recommended as a primary OSA treatment due to insufficient evidence supporting its effectiveness. Palatal implants may be an alternative for patients with persistent or recurrent snoring or mild OSA after LAUP (64).
Radiofrequency ablation (RFA)
RFA has emerged as a promising, minimally invasive treatment option for individuals grappling with mild to moderate OSA and other sleep-disordered breathing conditions. In contrast to conventional surgical interventions that can entail higher morbidity and extensive tissue manipulation, RFA offers distinct advantages, making it an appealing choice for both patients and healthcare providers. Given that long-term cardiovascular complications of OSA are associated with even lower values of the AHI, it is imperative for patients treated with RFA to undergo follow-up assessments for residual AHI, even if symptoms initially appear adequately improved (65).
One of the primary strengths of RFA lies in its ability to target multiple levels of the upper airway, including the turbinates, soft palate, and the base of the tongue (66). This multifocal approach emerges as a secure and efficient choice for appropriately selected individuals dealing with mild-to-moderate OSA. Moreover, RFA treatment presents minimal morbidity and is particularly suitable for patients who encounter challenges with or decline CPAP therapy (67). Indeed, Sonsuwan et al.'s (68), findings suggest that Transoral RFA treatment may effectively serve as the first-line treatment for mild to moderate OSA, with baseline AHI associated with preferable outcomes. Similarly, a prospective study comparing CPAP to radiofrequency submucosal ablation for mild to moderate obstructive sleep apnea demonstrated similar effectiveness of both therapies, indicating a potential role for primary treatment of mild to moderate OSA with submucosal ablation (69). These findings collectively highlight the comparable efficacy of Transoral RFA and submucosal ablation as alternative treatments for this patient population.
Farrar et al. adopted a comprehensive approach to address potential obstruction sites, resulting in clinically effective outcomes, including reductions in Epworth Sleepiness Scale scores and Respiratory Disturbance Index levels among patients with OSA syndrome. They concluded that RFA should be considered a viable treatment option, especially for patients who either refuse or cannot tolerate CPAP therapy (66) Additionally, RFA stands out due to its repeatability over time with minimal associated morbidity, enabling clinicians to fine-tune treatment to individual patients' needs and responses, enhancing its flexibility.
However, the decision to apply RFA at specific sites within the upper aerodigestive tract should be based on a thorough evaluation of each patient's anatomy and condition. Currently, there are no standardized recommendations for the application of RFA, underscoring the importance of personalized treatment planning.
A significant milestone in assessing RFA's efficacy for OSA was the completion of a randomized controlled trial comparing multilevel RFA with CPAP, the established gold standard for OSA management. Focusing on patients with mild obesity and mild to moderate sleep apnea, this study revealed that both multilevel RFA and CPAP demonstrated similar effectiveness in improving various aspects of patients' lives, including daytime sleepiness, sleep-related quality of life, and overall quality of life. These improvements were sustained over several months of follow-up, although long-term outcomes and the need for additional therapies remain areas of inquiry (70).
For patients with moderate to severe Obstructive Sleep Apnea-Hypopnea Syndrome (OSAHS) presenting with glossopharyngeal plane obstruction, a noteworthy alternative treatment approach was identified in a study by Zu et al., (71). Their research demonstrated that a combination of Expansion Sphincter Pharyngoplasty (H-UPPP) with either tongue base radiofrequency ablation or tongue base traction surgery exhibited similar efficacy. This suggests that both surgical interventions can effectively treat OSAHS based on the patient's specific condition and surgical requirements.
Genioglossus Muscle Advancement (GA)
In the treatment of moderate to severe OSA, some patients encounter difficulties with positive airway pressure therapy and may seek surgical alternatives such as GA. This surgical procedure involves advancing the genioglossus muscle to enhance the tension of the tongue base, thereby reducing the risk of the tongue collapsing into the airway during sleep.
Song et al. found in their meta-analysis, has shown that GA can independently reduce the AHI by an average of 41.7% (72). GA plays a vital role in the arsenal of surgical options for managing OSA. The described modification offers several advantages, including the reliable capture of the genial tubercle without an increased risk of tooth root injury, eliminating the need for bone grafting. Moreover, this approach allows for the maintenance or even reduction of the chin profile, making it particularly advantageous for patients with a prognathic profile and severe OSA (73).
Tracheostomy
Historically, the therapeutic landscape for OSA primarily centered around addressing upper airway obstructions, a central element in OSA's pathophysiology. Tracheotomy, introduced as a treatment option in 1969, emerged as an effective approach, supported by extensive research demonstrating its capacity to alleviate OSA symptoms (43). Nevertheless, recent years have witnessed a shift away from the widespread use of tracheotomy. Advances in upper airway surgeries and the development of less invasive alternatives have provided more patient-friendly options for managing upper airway obstruction.
However, it's crucial to acknowledge that tracheotomy still holds significance in specific OSA cases where other treatment modalities prove ineffective or unsuitable. The decision to pursue tracheotomy is guided by individualized patient assessments, with a steadfast commitment to delivering personalized care. While tracheotomy was once a primary method for addressing OSA by circumventing upper airway obstruction, its utilization has diminished due to the availability of less invasive yet equally effective alternatives. Nonetheless, it continues to play a pivotal role in selected cases, ensuring that patients receive the most appropriate and effective treatment tailored to their unique needs and medical conditions.
Tonsillectomy and adenotonsillectomy
Adenotonsillectomy is the preferred initial treatment for pediatric OSA (74). In adult cases, tonsillectomy is typically considered when the tonsil tissues are enlarged, and isolated tonsillectomy has demonstrated unexpected success rates, particularly in individuals with substantial tonsil enlargement and moderate OSA (AHI, below 30 per hour) (75). It is rarely performed alone in pediatric OSA cases; instead, it is commonly combined with adenoidectomy, proving effective as the primary treatment for most children (76). Numerous studies, including prospective interventional trials, have investigated tonsillectomy as a standalone therapeutic approach for adult sleep apnea. These investigations have consistently demonstrated a substantial reduction in the apnea-hypopnea index. Specifically, the initial mean index of 40 events per hour, with a 95% confidence interval ranging from 28 to 51, was markedly reduced to a final measurement of seven events per hour, encompassing a 95% confidence interval of 3 to 11. It is noteworthy that this favorable outcome was consistently observed across all patients who underwent tonsillectomy, with an impressive 64% achieving a state of complete remission from the condition (77). This suggest that tonsillectomy may effectively treat adult OSA, especially when patients have large tonsils and mild to moderate OSA (AHI < 30 per hour).
Conclusion
Obstructive Sleep Apnea is a complex sleep disorder with a wide array of treatment options. CPAP therapy is considered the gold standard treatment for moderate to severe OSA. Oral appliances, novel technologies, and various surgical interventions provide alternatives, each with its own set of benefits and limitations. Individualized treatment plans based on patient characteristics and preferences are essential to optimize outcomes. The choice of treatment should consider OSA severity, patient compliance, and potential comorbidities. Advances in non-invasive and minimally invasive treatments have expanded the options available to patients, improving their quality of life and reducing the associated health risks. Overall, a multidimensional approach to OSA management is essential to tailor treatments to individual patient needs and enhance overall well-being.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
