Volume 3, Issue 10
October 2023
Role of Nuclear Imaging in Infectious Diseases
Doha Ahmad, Abdulmohsen Alrawili, Ibrahim Al Zehefa, Mohammed AlQarous, Salem Alenezi, Baraa Hamed, Hazem Al-Ahmary, Eman Baothman, Saeed Bamani, Abdulaziz Alsubaie, Mohammed Alshehri, Kholoud Yousef,Mohammed Alghamdi
DOI: http://dx.doi.org/10.52533/JOHS.2023.31001
Keywords: nuclear imaging, infectious disease, infections, radiology, imaging
Pathogens such as bacteria, viruses, or fungi are well-known causes of infectious diseases, and these diseases have a greater impact on populations with limited resources. Rapid and accurate diagnostic criteria and methods are essential to address the emergence of infectious diseases. Improvements in diagnostic criteria and methods are critical to safeguarding public health and mitigating the impact of these diseases on a global scale. Nuclear medicine and imaging have been found to be effective in identifying lesions in patients with idiopathic fever and differentiating between infective and non-infective lesions. This research article reviews the use of nuclear imaging in the prevention, diagnosis, and treatment of infectious diseases, with a comprehensive literature review starting on September 4th, 2023, from research databases such as PubMed, Web of Science, and Cochrane. The literature search for this study focused on the burden of infectious disease, diagnostic inaccuracies, and their outcomes, the recent role of nuclear imaging, and sensitive diagnosis. While nuclear imaging is not typically the first-line diagnostic tool for infectious diseases, it can provide valuable insights in certain situations and should be further explored as a primary diagnostic tool. Nuclear imaging can be used to identify the location of the infection, the source of the infection, and to evaluate the progress of treatment therapy. It is also important to identify the sensitivity and specificity of each infectious disease case to accurately diagnose the disease using nuclear imaging. Although the use of these diagnostic tools is context-specific, nuclear imaging plays a valuable role in the comprehensive assessment of infectious diseases and contributes to improved patient care and research in the field of infectious disease management.
Introduction
Infectious diseases are commonly known to be caused by pathogens such as bacteria, viruses, or fungi and can be transmitted from one individual to another (1). They are associated with multiple determinants of health, such as water and sanitation, housing, climate, sociocultural, and socioeconomic factors, and hence have a disproportionate impact on populations with limited resources (2). Infectious diseases have historically placed a significant burden on human populations, and while progress has been made in controlling and preventing many of them, they continue to pose challenges, especially in certain parts of the world. A 2019 Global Burden of Disease (GBD) study estimated that six infectious diseases were among the top 10 causes of disability-adjusted life years (DALYs) in children less than 10 years of age (3). There was also a notable increase of 58.5% in the global age-standardized DALY rates of HIV/AIDS in 2019 (4). In addition to these statistics, infectious diseases are proven to be notorious, especially in lower-middle-income countries (LMICs). Emerging communicable diseases such as dengue, malaria, HIV/AIDS, and COVID-19 are hard examples of increasing morbidities and mortalities in the African and Asian regions within the past decade (5, 6). A collapse in the healthcare systems of several Middle Eastern countries, such as Syria and Iraq have caused a wave of emerging communicable diseases. Pathogenic infections like cholera, diphtheria, poliomyelitis, measles, and leishmaniasis have also been on the rise in the Gulf region (7).
The presence of rapid and accurate diagnostic criteria and methods is crucial to dealing with the rapid surge in the emerging epidemiological trends of infectious diseases. Given the evolving nature of infectious diseases and the potential for global pandemics, investment in research and development of rapid and accurate diagnostic tools is crucial to ensuring effective preparedness and response efforts. Advances in diagnostic criteria and methods play a critical role in safeguarding public health and mitigating the impact of emerging infectious diseases on a global scale. Patients with suspected pathogenic infections are often prescribed empiric antimicrobial therapy, which eventually leads to the global problem of antimicrobial resistance (AMR) (8). To address these challenges, healthcare systems, policymakers, and healthcare providers must prioritize strategies that promote antibiotic stewardship and responsible use. This includes the development and implementation of rapid and accurate diagnostic methods to guide targeted, effective treatment. To tackle these concerns, the Infectious Diseases Society of America (IDSA) recommends prioritizing diagnostics research and development and policy making (8). Moreover, accelerating the integration of advanced and improved diagnostic tests for disease prevention, treatment, and rehabilitation is also emphasized (8). Acute bacterial infections have been previously diagnosed with the help of CT scans and MRI; however, both of these methods are known to record secondary inflammatory changes, which are often not specific to the infection under scrutiny (9). Using nuclear imaging techniques can augment the information and visualization of infections in a rather effective manner.
Positron emission tomography (PET) and single-photon emission computed tomography (SPECT) are the prototype techniques for tracking the biochemical functions inside the human body. These imaging techniques are non-invasive and quantitative, providing information about the presence and location of specific molecules or radiotracers in the body and their concentrations (10). These techniques offer unique advantages for visualizing metabolic and physiological changes associated with infections. PET is a powerful imaging modality that involves injecting a patient with a radiotracer, which emits positrons. When a positron encounters an electron, they annihilate, emitting gamma rays. PET scans detect these gamma rays to create detailed 3D images of metabolic activity. It is widely used in oncology for cancer staging and treatment monitoring (11). SPECT, on the other hand, utilizes radiotracers that emit single gamma rays. A gamma camera rotates around the patient, capturing the emitted radiation and creating 3D images. SPECT is valuable in cardiology for assessing myocardial perfusion and in neurology for brain imaging (11). Gallium scanning and white blood cell scintigraphy are the types of nuclear imaging that are specifically used for infection and inflammation detection in the human body. Gallium-67 is used in Gallium scanning to detect sites of inflammation and infection, particularly in cases of fever of unknown origin or certain types of pneumonia, and White Blood Cell Scintigraphy uses white blood cells tagged with a radiotracer (11). Studies have shown that nuclear medicine and imaging are effective for patients with idiopathic fever. Moreover, identified lesions can also be differentiated based on whether they are infective or non-infective through nuclear imaging (12). This research article will review the contributions of nuclear imaging to the prevention, diagnosis, and treatment of infectious diseases.
Methods
This study is based on a comprehensive literature review started on September 4th, 2023, from research databases such as PubMed, Web of Science, and Cochrane. Multiple medical headings and their plausible combinations were utilized during the process. A manual search of research terms related to the topic was also carried out using Google Scholar. The burden of infectious disease, diagnostic inaccuracies and their outcomes on infectious diseases, the recent role of nuclear imaging, and sensitive diagnosis were the focal points of the literature search for this study. There were no exclusive criteria for the selection of articles.
Discussion
Nuclear imaging techniques, particularly PET and SPECT, can play a significant role in the diagnosis and management of infectious diseases in specific scenarios. While these techniques are not typically the first-line diagnostic tools for infectious diseases, they can offer valuable insights in certain situations and, hence, should be explored further as primary diagnostic tools. Nuclear imaging methods can be used in the following ways to extract information about infectious diseases:
Identification of infection sites and inflammation assessment
Nuclear imaging can identify the location of infection foci within the body (12, 13). Radiotracers can be used to detect areas of increased metabolic activity within the tissues, indicating the presence of an infection in that region. According to the European Society of Cardiology, abnormal metabolic activity in the perivalvular area on either FDG-PET imaging or radiolabeled leukocyte scintigraphy has been known as a crucial diagnostic criterion for infective endocarditis (14). Nuclear imaging can also visualize inflammation by targeting specific markers of inflammation, such as increased blood flow and immune cell recruitment. Complete body PET scans with certain radiotracers can help identify multiple infection sites in a single imaging session, making them particularly useful for systemic infections (11, 13).
Localization of Infection Source
Nuclear imaging is known to aid in determining the source of infection, such as by identifying an infected prosthetic device or abscesses (15). It may also assist in differentiating infections from non-infectious conditions that may have similar clinical presentations, helping to avoid unnecessary treatment (9, 11). Chronic infections such as tuberculosis or fungal infections can be difficult to diagnose using conventional methods (16). However, nuclear imaging has proven to be a useful adjunct in these cases (16, 17). In cases where conventional diagnostic methods may be inconclusive or where infections are difficult to detect through physical examination alone, nuclear imaging can help prevent delays in diagnosis and treatment.
Monitoring Response to Treatment
Nuclear imaging can also be used to monitor the response of infections to treatment (18, 19). This information is crucial for optimizing patient care. In cases where nuclear imaging reveals that treatment is not effectively reducing metabolic activity or inflammation at the site of infection, it can indicate treatment failure. This early detection allows for prompt intervention, such as adjusting the treatment or exploring the possibility of drug resistance (18, 19). Additionally, by tracking changes in metabolic activity at the infection foci or inflammation over a certain time, an assessment of treatment effectiveness can be ascertained (19). If the infection site shows decreased metabolic activity and reduced inflammation, it suggests that the treatment has been effective, potentially avoiding the continuation of unnecessary antibiotics or interventions.
Assessing the accuracy and clinical utility of diagnostic tests has been a crucial aspect of clinical medicine. The sensitivity and specificity of a diagnostic test are the fundamental metrics used to determine the performance, accuracy, and reliability of the diagnostic test (20). The sensitivity and specificity of nuclear imaging for infectious diseases can vary widely depending on several factors, including the specific radiotracer used, the type of infection, and the clinical context (11).
Sensitivity
Sensitivity in medical diagnostics measures a test's ability to correctly identify individuals with a specific condition (20). It quantifies the proportion of true positives, indicating cases correctly detected among those who truly have the condition. High sensitivity means the test effectively captures most positive cases, minimizing false negatives. This crucial metric ensures early disease detection, allowing prompt intervention and improved patient outcomes. However, excessively high sensitivity may lead to increased false positives, requiring a balance between accurate detection and minimizing unnecessary interventions (20). Sensitivity is vital for effective screening tests and diagnostic tools, guiding clinical decision-making and public health initiatives. The sensitivity of a nuclear imaging diagnostic test can be variable and depends on the radiotracer used and the type of infection targeted for diagnosis (20). In some cases, nuclear imaging can have high sensitivity, especially when radiotracers target specific infection-related markers such as glucose metabolism or inflammatory processes. For instance, for Takayasu arteritis, the sensitivity of nuclear imaging for diagnosis and therapy evaluation was found to be 92% (21). FDG-PET image for Takayasu arteritis is shown in Figure 1. Similarly, the sensitivities of Nuclear imaging for pancreatic cancer, osteomyelitis, and vasculitis were found to be 96%, 95%, and 92%, respectively (21). The robustness of imaging for osteomyelitis has been illustrated in Figure 2. In another study, a sensitivity of over 90% was observed for the diagnosis of endovascular graft infections using PET/CT (15), also illustrated in Figure 3. In addition to that, sensitivity results for fungal infections were also higher, and hence, PET scans for the detection of fungal infections as well as therapy evaluation were recommended (22). Evidence for the accurate diagnosis of musculoskeletal injuries using nuclear imaging also positively recommends the procedure for robust diagnosis (23).

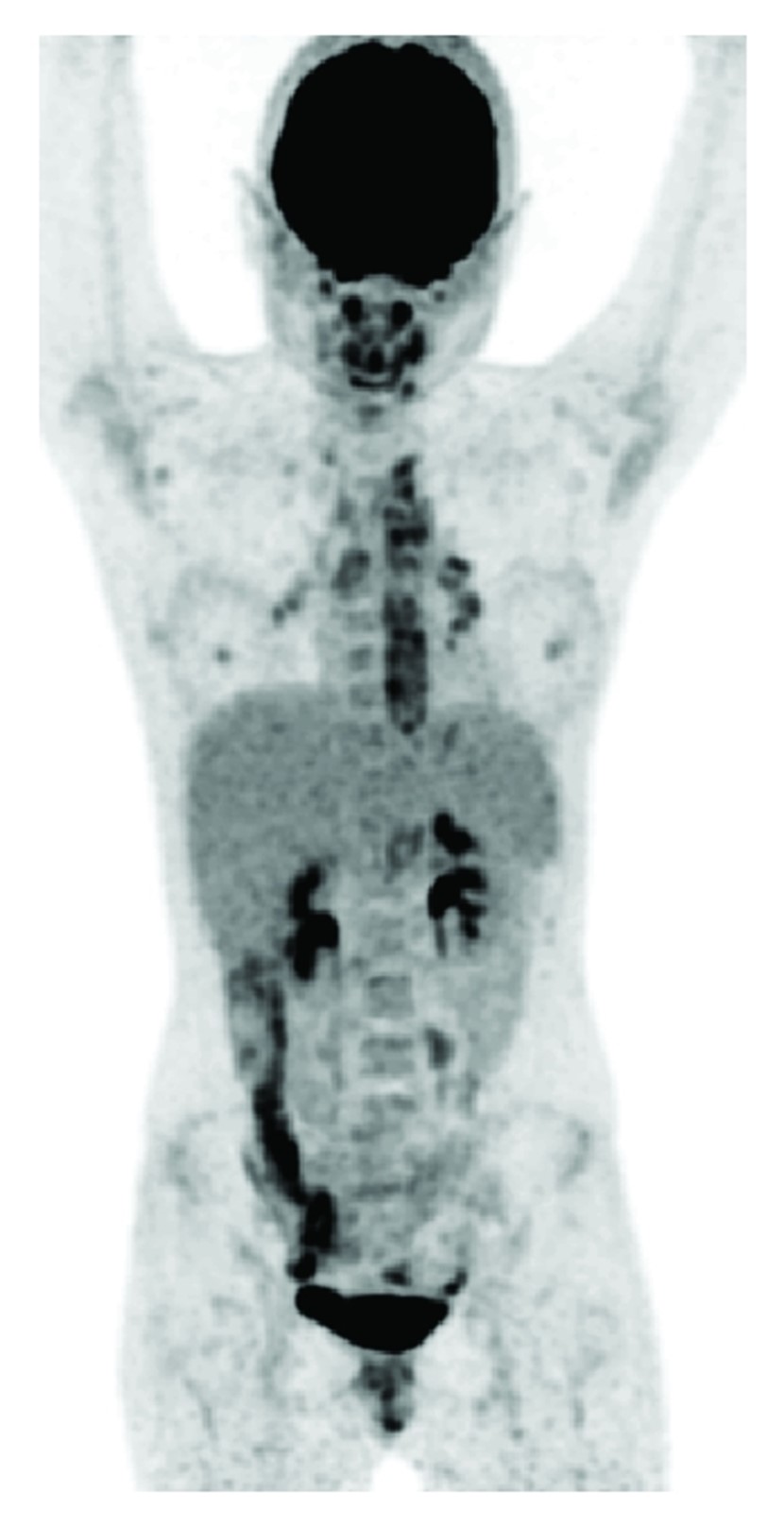
Figure 1: Takayasu’s arteritis: high FDG uptake located more centrally (aorta and main branches in the thoracic region) and in this case uptake in reactive lymph nodes in mediastinum and hill (confirmed by biopsy) (21)
On the other hand, sensitivity may be lower in cases of chronic or latent infections, as the metabolic activity or inflammatory response may be less pronounced. Diagnostic assessments of the use of nuclear imaging for patients with rheumatoid arthritis, and inflammatory bowel disease were found to be inconclusive (19). In the case of autoimmune thyroiditis, there is a lack of evidence, and hence, FDG-PET/CT should be avoided (21).
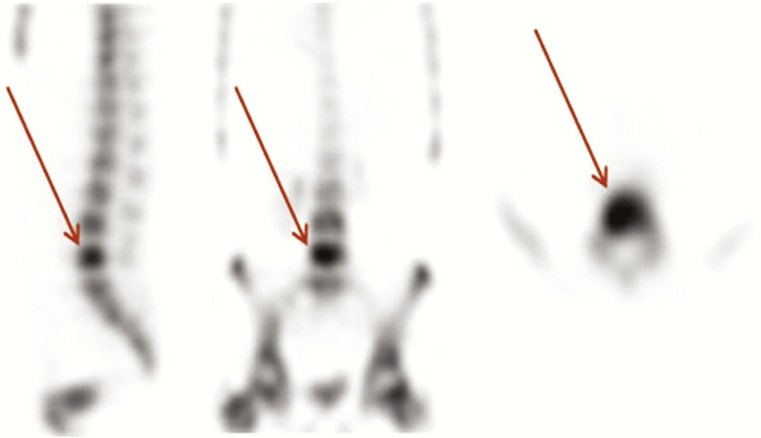
Figure 2: 99mTc-hydroxy methylene diphosphonate bone SPECT scan of a patient with osteomyelitis of fifth lumbar vertebra (24)
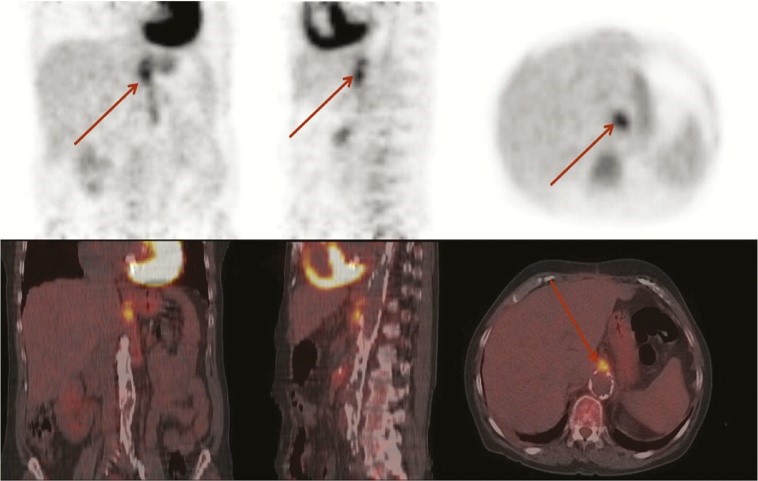
Figure 3: 18F-FDG PET/CT scan of patient with proven Escherichia coli infection of vascular graft (24)
Specificity
Specificity in medical diagnostics gauges a test's capacity to correctly identify individuals without a particular condition (20). It quantifies the proportion of true negatives, signifying cases correctly excluded among those who genuinely do not have the condition. High specificity ensures a low rate of false positives, reducing unnecessary anxiety and interventions. It is essential for confirming true disease absence and ensuring the reliability of negative test results. However, excessively high specificity might increase false negatives (20). Striking a balance between specificity and sensitivity is vital to developing accurate diagnostic tests. Specificity plays a pivotal role in preventing misdiagnoses and guiding appropriate clinical decisions for patient care. Similar to the sensitivity, specificity can also vary depending on the radiotracer and the type of infection (20). High specificity radiotracers are designed to target infection-specific markers. 100% specificities were reported for vasculitis as well as Takayasu arteritis in the literature for FDG-PET, combined with CT (21). 80% specificity was quoted in the literature for the diagnosis and therapy evaluation of prosthetic valve endocarditis (PVE) (25), and 90% for overall infective endocarditis (26), using PET scans. Further better specific accuracy (100%) was observed by using Radiolabeled leukocyte scintigraphy (27). Despite the presence of such strong evidence supporting the specificity of nuclear imaging, lower specificity rates have also been reported, particularly in cases where inflammation or other non-infectious conditions can lead to increased uptake of the radiotracer, potentially leading to false-positive results. Lower specificities were observed for PET scans in infections such as sarcoidosis (21) and osteomyelitis attributed to diabetic foot (28).
It is safe to deduce that both the sensitivity and specificity of nuclear imaging should be considered within the broader clinical context. The diagnostic accuracy of any test often depends on a combination of clinical evaluation, laboratory tests, imaging findings, and patient history (11). In addition to that, the choice of radiotracer plays a significant role in determining the accuracy of nuclear imaging for infectious diseases. Researchers and clinicians continuously work on developing and optimizing radiotracers to improve the diagnostic accuracy of nuclear imaging for specific infectious diseases, thus recuperating the sensitivity and specificity of each diagnostic test. Hence, the sensitivity and specificity of nuclear imaging for infectious diseases should be evaluated on a case-to-case basis (20, 21). Moreover, nuclear imaging is often used in conjunction with other diagnostic tools, such as blood tests, microbiological cultures, and clinical evaluation, to provide a comprehensive assessment. This synergistic approach helps in accurately diagnosing medical conditions, planning treatments, and monitoring the progression of diseases, ultimately improving patient care, and advancing medical knowledge. The choice of imaging modality and radiotracer depends on the specific clinical scenario and the suspected infectious agent (11). Highlighting the limitations of the use of nuclear imaging for the diagnosis and treatment of infectious diseases, nuclear imaging is known to involve exposure to ionizing radiation. Ionizing radiation, while invaluable in medical diagnostics and various other applications, also has several disadvantages and potential risks, such as the risk of cancer, tissue damage, unwanted genetic mutations, and radiation sickness.
The risk-benefit ratio of such procedures must be evaluated, especially in vulnerable populations such as pregnant women and children. Additionally, these techniques may not be readily available in all healthcare settings, and their use is typically reserved for cases where they can provide unique diagnostic insights. The key to optimizing the risk-benefit ratio of nuclear imaging lies in careful patient selection, dose optimization, adherence to safety guidelines, and informed decision-making in consultation with healthcare providers. When used judiciously and appropriately, nuclear imaging contributes to enhanced patient care, facilitates research and drug development, and plays a vital role in advancing our understanding and management of various medical conditions.
Conclusion
Nuclear imaging techniques like PET, SPECT, FDG-PET, and Radiolabeled leukocyte scintigraphy may not be the first-line methods for diagnosing infectious diseases, but they do provide unique insights and are utilized in specific clinical scenarios to aid in the diagnosis and management of infections. These imaging modalities offer valuable information about infection localization, monitoring treatment response, detecting chronic infections, and differentiating infections from other conditions. While its use is context-specific and often accompanied by other diagnostic tools, nuclear imaging plays a valuable role in the comprehensive assessment of infectious diseases and contributes to improved patient care and research in the field of infectious disease management.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.