Volume 3, Issue 9
September 2023
The Impact of Family Medicine on Diabetic Eye Care, Screening Programs, Referral Patterns, and Outcomes
Ahmed Alnahdi, Haifa Alkheledan, Ahmad Himayda, Elaf Alturkustani, Ahmed Al Ghareeb, Zahra Al Mattar, Lujain Allehyani, Samer Miski, Majed Alnewaiser, Ayman Alshumrani, Mohammed Alrehaili
DOI: http://dx.doi.org/10.52533/JOHS.2023.30904
Keywords: diabetes, eye, complication, retinopathy, screening
Diabetes mellitus is a long-lasting metabolic disease with a complex etiology. It is characterized by elevated blood sugar levels, which are marked by anomalies in insulin secretion, action, or both. Long-term hyperglycemia causes diverse microvascular and macrovascular diabetic complications, which are primarily responsible for the high morbidity and mortality associated with diabetes. Diabetes leads to significant ophthalmological complications among which diabetic retinopathy is thought to be the most frequent cause of blindness in people of working age, with diabetic macular oedema being the most frequent cause of impaired visual acuity among diabetics. The findings of several research studies suggest that the best way to prevent diabetic retinopathy from leading to blindness is through regular assessment and screening so any complications can be addressed as soon as possible. Furthermore, since early diabetic eye disease stages are asymptomatic, screening people with diabetes is essential. As a result, the primary care physician's involvement is essential for enabling an early diagnosis of this condition. Family physicians play an essential role in the early identification and prevention of diabetic retinopathy. They serve as the initial line of contact for managing diabetes and as referral sources when complications arise. The purpose of this research is to review the impact of family medicine on diabetic eye care, screening programs, referral patterns, and outcomes.
Introduction
Diabetes mellitus is a chronic metabolic disease with a complicated pathophysiology. It is characterized by increased blood glucose levels, or hyperglycemia, caused by abnormalities involving either insulin secretion, insulin action, or both. Long-term hyperglycemia leads to diverse microvascular and macrovascular diabetic complications, which are primarily responsible for significant diabetes-related morbidity and mortality (1). Almost 9.3% (463 million people) of the global population in 2019 were expected to be affected by diabetes, whereas this trend tends to rise to 10.2% (578 million) by 2030 and 10.9% (700 million) by 2045 (2). In Saudi Arabia, 23.7% of the population is diabetic, which is one of the highest rates in the world. Diabetes mellitus leads to numerous complications, one of which is diabetic retinopathy (DR). It is one of the leading causes of blindness in people of working age. It is considered that after 20 years of diabetes, more than 60% of type 2 diabetic patients will develop some retinopathy (3).
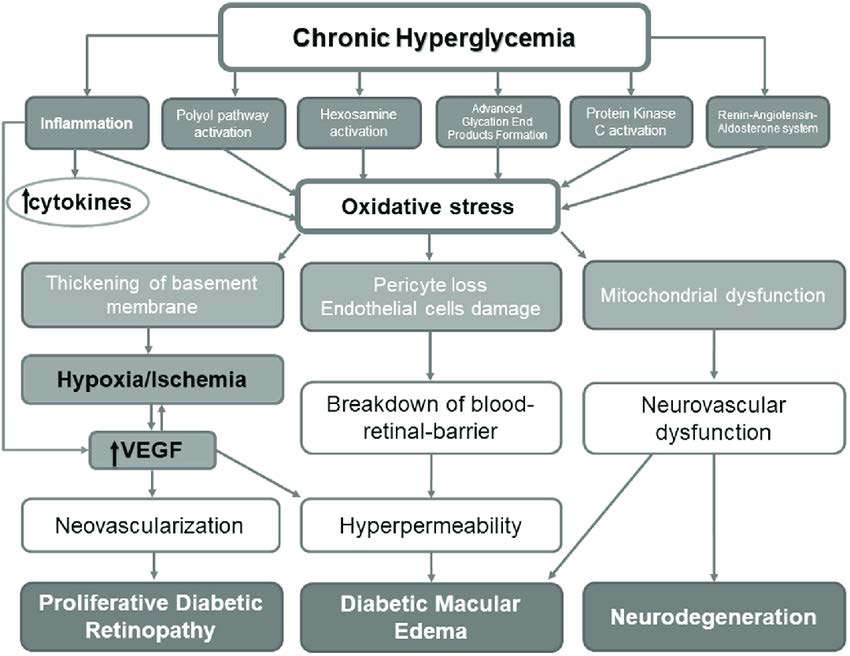
Chronic hyperglycemia induces a cascade of biochemical and structural alterations in retinal arteries, resulting in DR, diabetic macular oedema, and neurodegeneration (4). This pathophysiology is illustrated in Figure 1. Primary care physicians are the front-line healthcare providers for diabetic patients and additionally act as significant sources of information about DR for patients. Understanding the ocular symptoms of diabetes and knowing the screening recommendations can thus influence the timeliness with which primary care or family physicians refer patients to ophthalmology clinics. Ophthalmologists are well aware that the timing of laser treatment in proliferative DR can have a significant impact on the patient's long-term eyesight. DR must be diagnosed with a dilated fundus exam at least once a year. According to the findings of various studies, approximately 31% to 65% of diabetic individuals undergo a yearly dilated fundus test. Although this low incidence is mostly attributed to patient misunderstanding and non-compliance, family physician referral to an eye care specialist may also play a role (5).
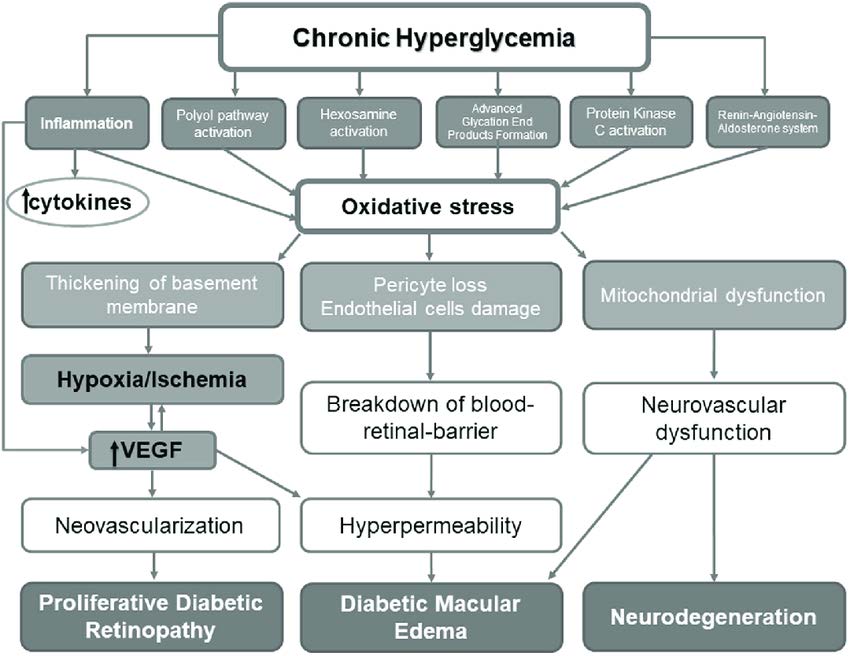
Figure 1: The pathophysiology of diabetic retinopathy (4)
DR progresses in phases from non-proliferative DR to proliferative DR. Early diagnosis and prompt referrals are vital for preventing further deterioration. General physicians play an important role in the community because they are patients' first point of contact. Guidelines from numerous associations advise physicians caring for diabetic patients on how to screen for conditions requiring referral to an ophthalmologist (6). A pictorial representation of DR is shown in Figure 2.
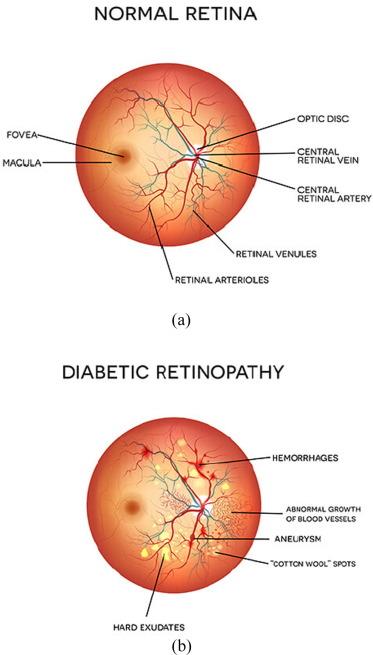
Figure 2: Illustrative representation of diabetic retinopathy in comparison to normal retina (22)
To prevent diabetes-related eye diseases related to vision loss, highly effective treatments such as retinal laser photocoagulation and intravitreal injection therapy are available. However, the efficacy of these treatments is dependent on early diagnosis. Because early diabetic eye disease stages are asymptomatic, screening people with diabetes is essential. Countries with nationwide screening programs have reduced diabetic eye disease-related blindness by up to 50%. The overall image quality achieved in general physician-based diabetic eye disease screening is satisfactory, and it should be accepted by ophthalmologists and patients in the majority of instances (7). The purpose of this research is to review the impact of family medicine on diabetic eye care, screening programs, referral patterns, and outcomes.
Methodology
This study is based on a comprehensive literature search conducted on August 10, 2023, in the PubMed, Web of Science, Science Direct, and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed the impact of family medicine on diabetic eye care, screening programs, referral patterns, and outcomes. There were no restrictions on date, language, participant age, or type of publication.
Discussion
Diabetes is becoming more prevalent, and it has emerged as the leading cause of blindness worldwide. Diabetes and its related vision-threatening disease have become a worldwide epidemic, resulting in increased healthcare costs and disability (8). Diabetes-related ophthalmological complications can be effectively treated with early intervention, for which family physicians are critically important. During the monitoring of patients with ophthalmologic pathology, the family physician might adopt diagnostics and treatments utilizing professional knowledge and abilities. The family physician can diagnose 18.8±1.2% of eye diseases in patients 40 years of age and older, including 4.6±0.7 cases of myopia, 3.8±0.6 cases of hyperopia, 2.2±0.5 cases of astigmatism, 1.4±0.4 cases of cataracts, 2.3±0.5 cases of glaucoma, 0.1±0.1 cases of DR, and 4.4±0.7 cases of other eye diseases (9).
When diagnosed early, laser photocoagulation can help prevent blindness. However, due to the disease's silent nature, the majority of individuals present late and in irreversibly advanced stages. Thus, regular screening is critical for the early detection of DR changes. This underscores the necessity of family physicians being aware of the standardised diabetes-screening recommendations and implementing them in their practise (10). Improving physician adherence to guideline-recommended care remains a challenge; one such barrier is the prompt referral of a DR for evaluation. Furthermore, busy primary care practises lacking organisational support and computerised monitoring systems, telecommunication, and sustainability have outstripped the capability and resources for DR eye care implementation, increasing the burden of DR eye care on the health care system and economy. With a restricted healthcare budget and increasing morbidity due to DR, it is critical to investigate concerns concerning physicians' knowledge and practises, as well as the current healthcare system for DR (11).
Evidence from literature
Gale et al. suggested that, as per recent guidelines and practise patterns in individuals with type 1 diabetes, the first eye exam should be done 5 years following diagnosis and subsequently every year if there is no diabetic retinopathy. While an initial eye exam for patients with type 2 diabetes should be performed at the time of diagnosis and then annually if no DR is noted, Pregnancy is a significant risk factor for uncontrolled hyperglycemia and the advancement of DR, according to multiple studies. Screening for pregnant patients with type 1 diabetes is advised soon after conception, while when possible, screening for type 2 pregnant patients should occur prior to conception, with follow-up early in the first trimester (8). Family physicians play an integral role in this context, as they are the first to identify diabetic eye diseases and opt for screening. Tierney highlighted the importance of family and primary care physicians as they initiate the patient on a program of watchful follow-up, treatment, and referral to an ophthalmologist from the initial fundoscopic examination and visual acuity evaluation (12).
Gill et al. reported that the nonmydriatic ophthalmoscope and standardised screening criteria resulted in a rather good sensitivity for screening for diabetic retinopathy by general physicians. When compared to an ophthalmologist's assessment utilising retinal diagrams, the mean sensitivity for the right decision to refer for further investigation was 87%, with a specificity of 57%. When compared to the current family physician's approaches, this degree of accuracy constitutes an improvement. Previous research has shown that even when the eyes are dilated, physicians utilising traditional direct ophthalmoscopy properly identify less than 50% of severe retinopathy. Even experienced ophthalmologists have rates of correct assessment of just approximately 50% when utilising regular direct ophthalmoscopy without dilatation (13). However, Song et al. reported concerns concerning the usefulness of fundoscopy as a DR screening technique in primary care, which were raised by the fact that all primary care physician’s documentation of fundoscopic examination results was normal, even though nearly 40% of the same individuals were found to have the disease when seen by a specialist. Although earlier studies suggested that training might increase family physician's DR screening accuracy, it is still necessary to compare the cost-effectiveness of this strategy to other population-based screening methods, such as teleretinal imaging programs and artificial intelligence diagnostics. Furthermore, however, the authors agreed that family physicians play an essential role in the screening for diabetic DR, particularly in areas with limited access to specialised eye care (14).
Yung et al. reported that almost 35% of general physicians claimed they never suggest patients for an ocular checkup, while 26% indicated they always refer patients. The remaining ones refer to specific instances. Only 70% of patients who are not referred to a specialist have their fundus examined by their primary care physician, and 96% of these examinations have been performed with an undilated pupil. At the time of referral, 20% of Type I patients are diagnosed, while 50% are diagnosed after one year. Moreover, only 2% of Type II patients are referred at the time of diagnosis, and 70% are referred after a year. Optometrists receive 20% of recommendations, whereasophthalmologists receive 75% of them. This demonstrates that a significant percentage of family physicians do not adhere to the suggested standards established for the management of diabetic eye (15).
Liu et al. narrated that the majority of family physicians have knowledge of diabetic eye screening recommendations. Results of a knowledge-based study demonstrated that 81% of primary care physicians scored professionally, indicating that low screening rates are more likely to be explained by causes other than a lack of provider knowledge. Although most physicians believe their eye exam skills are insufficient to perform diabetic eye screening, they are generally trained to perform direct ophthalmoscope eye exams during medical school. This training is sometimes rather restricted, and most physicians are not confident in the accuracy of their exams for diabetic eye screening (16). Raising the concern of not effectively practising the screening programs Silva et al. concluded that diabetes-related ophthalmic complications are not effectively screened, particularly in primary care settings, and additional quality improvement initiatives may increase adherence to suggested screening regimens (17).
Research has shown that people are more likely to be tested or screened if their family physician recommends it, and patients with diabetes rely on their physicians for advice on how to manage all aspects of the disease. Therefore, patients should discuss their visual health with their physicians, and they should recommend complete dilated eye exams on an annual basis. Early diagnosis and prompt treatment of diabetes can frequently avoid vision loss and blindness; unfortunately, many individuals seek eye care too late for the treatment to be beneficial (18). Marie et al. described how family medicine physicians improve the administration of healthcare services. The family physician needs to perform a direct ophthalmoscopy right away when diabetes is identified. Sometimes, ophthalmological evaluation is limited to patients with chronic diabetes or visual disturbances, concentrating more on symptoms than signs (19).
Chen et al. stated that while the ophthalmologist can offer the patient DR specialised services, the family or primary care physician is primarily responsible for prevention and control. Therefore, they can only save the sight of the thousands at risk for diabetic retinopathy when primary and specialised care have developed entrenched cooperation (20). Similarly, Watson et al. described that, compared to other medical professions, general practitioners examine more diabetic patients, and many of these patients remain connected with them for a long time. Consequently, general physicians are in a good position to conduct an opportunistic screening. Moreover, findings demonstrated that individuals who participated in the interviews viewed themselves as the guardians of the healthcare system and were eager to contribute more significantly to DR screening provided their demands could be addressed (21). Early diagnosis is one of the foundational steps in diabetic eye care that can be effectively performed by family physicians, as early diagnosis will lead to prompt referral and management, which can successfully prevent more serious complications and blindness. Our review highlights the importance of family physicians in diabetic eye care. Additionally, we recommend that regular training sessions for family physicians to educate more on diabetic eye care screening and referral are needed so more accurate diagnoses of diabetic eye diseases are made timely since few studies included in the review reported a lack of physician trust and capability in diagnosis. Furthermore, the family physician’s role in the management of diabetic eye diseases could not be elaborately studied due to the dearth of studies in the literature, which is the limitation of our paper. This underscores the need for further clinical research so the outcomes of the involvement of family physicians in the management of diabetic eye diseases can also be assessed.
Conclusion
Family physicians play an essential role in the early identification and prevention of DR. They serve as the initial line of contact for managing diabetes and as referral sources when complications arise. Therefore, their knowledge and efficacy in the diagnosis of diabetic eye diseases is of prime importance. Awareness and training sessions for family physicians for diabetic eye diseases should be promoted and held on a regular basis to reduce diabetic ophthalmological complications and achieve optimal outcomes in patients through timely prevention and management.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.