Volume 2, Issue 12
December 2022
Case of COVID-19 and Acute Pancreatitis: A Case Report
Ahmad R. Alghamdi, Khalid W. Al-Hariqi, Fatimah M. Bahathiq, Wajd Y. Assahafi, Yara A. Halabi, Abdulmoeen M. Alqarni
DOI: http://dx.doi.org/10.52533/JOHS.2022.21218
Keywords: Acute pancreatitis, COVID-19, Renal vein thrombosis, Diabetic ketoacidosis
Background: Respiratory symptoms, including cough, shortness of breath, and fever, have been reported to be the most common symptoms of Coronavirus disease (COVID-19). However, extra respiratory symptoms, such as gastrointestinal manifestations, have also been reported.
Case Presentation: In our paper, we report a case of a 32-year-old African female patient with no previous medical history who presented to the emergency department with altered mental status for one day. The patient had a history of fever, epigastric pain, decreased oral intake, vomiting, and diarrhea. Initial laboratory findings revealed elevated blood glucose, amylase, lipase, blood urea nitrogen, and creatinine levels. Urine ketones were also positive, and blood gases demonstrated severe metabolic acidosis. The patient was admitted to the intensive care unit as a case of diabetic ketoacidosis, acute kidney injury and acute pancreatitis that was later confirmed by computed tomography imaging, where it revealed bilateral renal vein thrombosis with left kidney infarction. Additionally, reverse transcriptase-polymerase chain reaction (RT?PCR) confirmed COVID-19. The patient improved significantly following conservative management and anticoagulation and was discharged home.
Conclusion: Our case demonstrates the importance of considering COVID-19 as a possible cause of acute pancreatitis and that acute kidney infarctions should be part of the differential diagnosis of acute kidney injury in patients who are COVID-19 positive.
Introduction
Acute pancreatitis in adults is most commonly caused by cholelithiasis and excessive alcohol intake. Other causes include infections, hypertriglyceridemia, hypercalcemia, exposure to certain drugs, toxins, ischemia, and trauma (1).
Coronavirus disease (COVID-19) is a disease caused by infection with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) that rapidly evolved into a global pandemic after being first discovered in Wuhan, China (2). Even though COVID-19 mainly affects the respiratory system, other systemic manifestations have been reported and cannot be neglected, such as thromboembolic events involving both the arterial and venous systems, which have been linked to COVID-19 in the recent literature (3–6). Renal manifestations, including acute kidney injury caused by kidney infarction, have also been reported in patients with COVID-19 (7).
Case Presentation
A 32-year-old African woman with no previous medical history presented to our emergency department (ED) with altered mental status for one day. According to her family, the patient complained of fever, decreased oral intake, epigastric pain, severe anorexia, diarrhea, and vomiting for one week. She described the pain as a continuous sharp epigastric pain that radiated to the back, was aggravated by lying down and was slightly relieved by leaning forward. The patient denied history of edema, recent abdominal trauma, alcohol consumption, smoking, or illegal drug abuse. She also denied taking any medications. There was no history of contact with sick people.
Upon examination in the ED, the patient appeared ill and was in pain with a Glasgow Coma Scale (GCS) of 13 (E:3 M:5 V:5). She was hemodynamically stable with a body temperature of 36.6 °C, a pulse rate of 107 bpm, blood pressure of 145/83 mmHg, a respiratory rate of 22 breaths per minute, and oxygen saturation of 98% on room air. Abdominal examination showed mild epigastric tenderness without guarding or rigidity. No other findings were apparent.
Initial arterial blood gas on room air exhibited a severe metabolic acidosis with pH 7.10, PCO2 44 mmHg, PO2 32 mmHg, and HCO3 11. Her glucose level was 64.79 mmol/L, and her urine ketones were positive. Complete blood count revealed a hemoglobin level of 145 g/L, leukocyte count of 5.19×109/L, and platelet count of 271×109 L. Lactate dehydrogenase was 333 U/L. Creatinine was 500 μmol/L, blood urea nitrogen 31.29 mmol/L, albumin 29 g/L, and serum calcium level 2.4 mmol/L. In addition, her liver function tests were within normal limits: aspartate transaminase 25 U/L, alanine transaminase 14 U/L, total bilirubin 8 µmol/L, and direct bilirubin 2.19 µmol/L. A significant elevation was noted in both amylase and lipase levels 1182 iU/L and 417 iU/L, respectively. Anterior-posterior (AP) view of the chest X-ray showed bilateral opacities with peripheral infiltration (Figure 1). Abdominal ultrasound showed no sonographic evidence of cholelithiasis, acute cholecystitis, or biliary obstruction.
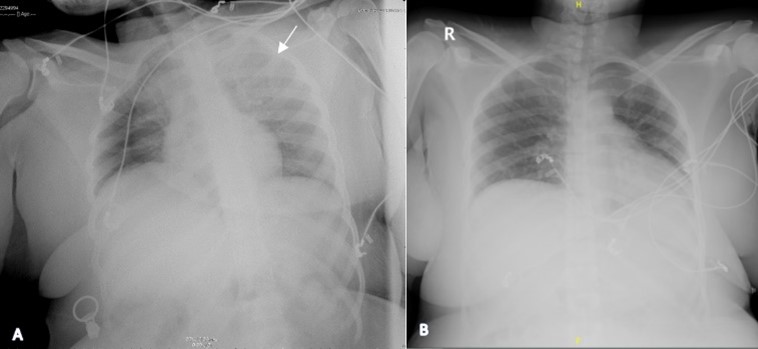
Figure 1: AP view chest X-ray taken upon admission (A). Repeated chest X-ray (B)
The patient's condition worsened, and she became tachycardiac with a pulse rate of 155 bpm, hypotensive 79/52 mmHg, mean arterial pressure 64 mmHg, tachypneic with a respiratory rate of 33 breaths per minute, oxygen saturation of 98% on room air, and her GCS score declined to 9 (E:3, M:5, V:2). She was admitted to an isolation room in the intensive care unit as a case of acute pancreatitis, acute kidney injury (AKI), and diabetic ketoacidosis (DKA). Considering the diagnosis, she was kept nil per os (NPO) and was treated conservatively with good hydration, optimization of electrolyte balance, and insulin infusion. Given the presentation, the diagnosis of an infected necrotizing pancreatitis was considered, and the patient was started on Meropenem.
By the next day, reverse transcriptase-polymerase chain reaction (RT?PCR) was positive for COVID-19 infection. Based on the clinical picture and bilateral infiltration on chest x-ray, this result was confirmatory of a COVID-19 infection. Furthermore, a computed tomographic (CT) scan of the abdomen showed evidence of acute pancreatitis without any structural abnormality and bilateral renal vein thrombosis with left kidney infarction (Figure 2), and the patient was started on a heparin infusion.
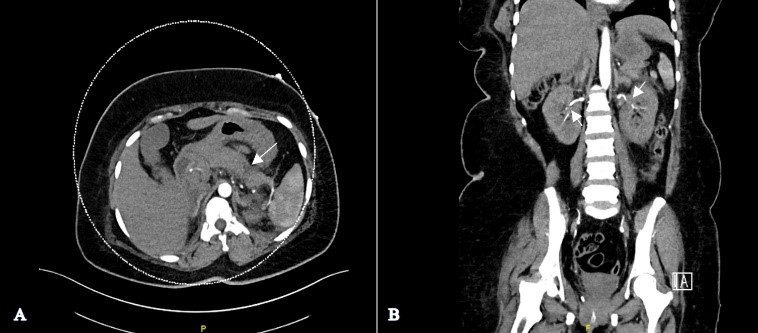
Figure 2: A) Axial computed tomography scan of the abdomen with contrast showing fat stranding and free fluid surrounding the pancreas suggestive of acute pancreatitis. B) Coronal computed tomography scan of the abdomen with contrast showing a filing defect in t
Three days following the initial positive RT?PCR result, a repeated sample was negative for COVID-19. A high-resolution CT (HRCT) scan showed bilateral peripheral ground glass opacities and bilateral lower lobe-dependent atelectasis (Figure 3).
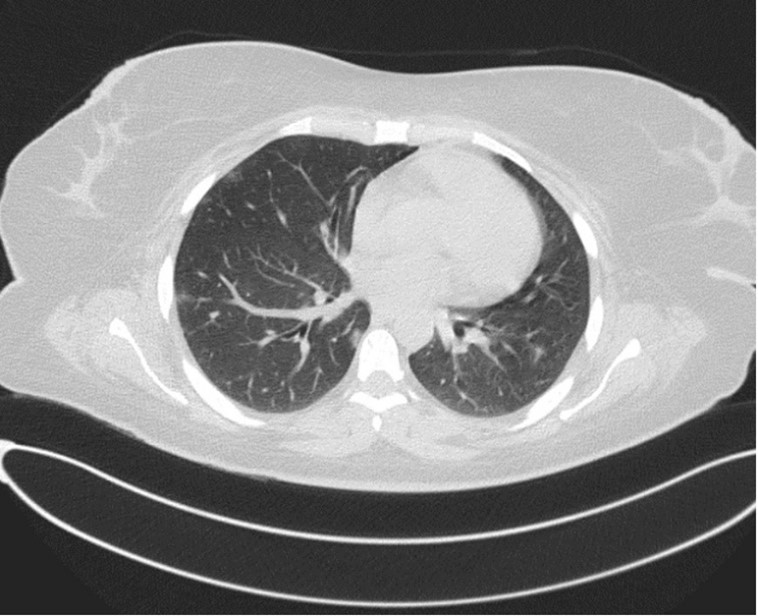
Figure 3: A high-resolution CT (HRCT) scan showed bilateral peripheral ground glass opacities and bilateral lower lobe-dependent atelectasis
The patient received Meropenem for a total of 14 days, Caspofungin for 5 days, and Favipiravir for seven days. She improved clinically during her hospital stay and was accordingly discharged home as a case of post-COVID-19 hypercoagulopathy, bilateral renal vein thrombosis, and newly diagnosed diabetes based on the presence of manifestations of DKA, high fasting blood glucose (13 mmol), and hemoglobin A1C of 7.7% on warfarin sodium 5 mg tablets, insulin ASPART 10 I/U TID, and insulin glargine 22 I/U Q24 hrs with outpatient follow-up appointments in the diabetology and coagulation clinics.
Discussion
COVID-19 mainly presents with respiratory manifestations. However, the literature has also reported gastrointestinal and hepatobiliary manifestations in many patients (1,8). Furthermore, COVID-19 is considered to be a predisposing factor for both venous and arterial thrombotic events due to Virchow Triad disturbances (9). Renal vein thrombosis (RVT) is a rare condition that most commonly occurs in patients with nephrotic syndrome and other conditions that increase the risk of hypercoagulopathy, including COVID-19, as seen in previously reported cases (7,10).
On the other hand, acute pancreatitis is a common disease with well-known risk factors and has recently been linked to COVID-19 infections in multiple case reports (11–14). Although the exact etiology has yet to be determined, it has been proposed that increased angiotensin-converting enzyme 2 (ACE-2) expression in pancreatic cells may increase the susceptibility to entry of SARS-CoV-2 into the host cell, making it a target cell for COVID-19 infection. (15)
This case reflects a rare presentation of simultaneous acute pancreatitis and bilateral renal vein thrombosis in a patient with a positive COVID-19 infection. Our patient did not exhibit respiratory symptoms initially, but rather, she presented with manifestations of DKA and AKI, as well as gastrointestinal symptoms suggestive of acute pancreatitis, which was confirmed by laboratory (Table 1) and radiological imaging (Figure 2).
|
Table 1: Summary of laboratory findings |
||
|
Patient’s Results |
Laboratory Reference Range |
|
|
Hemoglobin (g/L) |
145 |
120-150 |
|
Leukocytes: WBC count (109/L) |
5.19 |
4-11 |
|
Platelet count (109/L) |
271 |
150-400 |
|
Prothrombin time (sec) |
15.3 |
11-16 |
|
Partial thrombin time (sec) |
22.5 |
26-39 |
|
International normalized ratio (INR) |
1.17 |
0.8-1.2 |
|
Arterial blood gas |
||
|
pH |
7.10 |
7.35-7.45 |
|
PCO2 (MmHg) |
44 |
35-48 |
|
PO2 (MmHg) |
32 |
83-108 |
|
HCO3 (mmol/L) |
11 |
21-28 |
|
Alanine transaminase (U/L) |
14 |
14-60 |
|
Aspartate transaminase (U/L) |
25 |
15-37 |
|
Total bilirubin (µmol/L) |
8 |
0-18.7 |
|
Direct bilirubin (µmol/L) |
2.19 |
0-3 |
|
Albumin (g/L) |
29 |
34-50 |
|
Amylase (U/L) |
1182 |
25-110 |
|
Lipase (U/L) |
417 |
10-60 |
|
Serum calcium (mmol/L) |
2.4 |
2.1-2.55 |
|
Blood glucose (mmol/L) |
64.79 |
3.6-6.1 |
|
Hemoglobin A1C |
7.7% |
4.5-6.2 |
|
Creatinine (µmol/L) |
500 |
44-90 |
|
Blood urea nitrogen (mmol/L) |
31.29 |
2.6-6.4 |
|
Urine RBCs (/Hpf) |
Nill |
|
|
Urine ketones |
Present |
|
Other possible causes of acute pancreatitis were ruled out, and the patient was managed accordingly. Based on the clinical context of our patient, lack of other risk factors, and further workup we trust that the occurrence of bilateral renal vein thrombosis was most likely caused by vascular damage and coagulopathy secondary to Coronavirus. Close observation of the patient showed that her condition gradually improved, with complete resolution of the symptoms. The patient had a favorable outcome and was discharged with follow-up appointments.
Conclusion
Even though acute pancreatitis is a well-known condition with multiple risk factors, our case demonstrates a possible causal relationship between COVID-19 infection and acute pancreatitis. This information may be beneficial in predicting COVID-19 as a possible cause of both acute pancreatitis and renal vein thrombosis. We believe that a full workup is necessary to avoid making an incorrect diagnosis and that acute kidney infarctions should be a differential diagnosis of AKI in patients with COVID-19 infection.
Disclosure
Conflicts of interest
The authors declare no conflicts of interest for this report.
Funding
None.
Ethical considerations
Written informed consent was obtained from the patient for publication of this case. The ethics committee’s approval was not required for publication, as this is a case report.
Data availability
Further data can be obtained from the corresponding author, Dr. Yara A. Halabi, upon reasonable request.
Author contributions
Ahmad R. Alghamdi, Fatimah Bahathiq, Wajd Assahafi, and Yara Halabi: Study conception, data collection, data analysis; writing reviewing & editing. Khalid Al-Hariqi: data analysis; writing reviewing & editing. Abdulmoeen Alqarni: supervision and data validation.
