Volume 2, Issue 12
December 2022
Geriatric Burn Injuries: Prevalence, Management and Clinical Outcome
Safinaz Alshiakh, Dhari Alroudan, Samah Alghamdi, Ali Alhalbub, Theyab Alghamdi, Ohud Althagafi, Fatimah Al Hammad, Ghaida Altheyab, Maram Alajmi, Hassan Alsalem, Mohammed Alshahrani, Abdulelah Bakhsh
DOI: http://dx.doi.org/10.52533/JOHS.2022.21206
Keywords: geriatric, burn, patients, outcome
Burns are a significant public health issue that result in more than 180 000 fatalities annually. For specialized burn care, the geriatric burn population is a sensitive and usually challenging group. Despite the fact that all age groups have shown advances in burn care, geriatrics still have worse survival rates. Burn severity, treatment, and outcomes are impacted in geriatrics because of the physiological differences between them and younger adult burn patients. The atrophic skin of the elderly results in deeper burns, or a higher ratio of full-thickness total body surface area compared to younger patients, but it also hinders the healing of both donor sites and burns. The purpose of this research is to review the available information about geriatric burn injuries: prevalence, management and clinical outcome. Elderly people are more susceptible to complications such pneumonia, congestive heart failure, and pulmonary edema. The morbidity and mortality seen in geriatric burn patients are also attributed to altered immunological and inflammatory response driven by age leading to increased hospital stays and more severe complications. Management of geriatric burn patients involves two concepts. the revolutionary theory of eschar excision and wound closure within the first week of hospitalization, and the conventional strategy of reducing physiologic stress by delaying surgery in the early post-burn stage while the development of effective fluid resuscitation protocols, which has most significantly boosted patient survival, is one of the pillars of modern burn care. The epidemiology of burn injuries in geriatrics is quite variable and demands further research.
Introduction
Burn injuries are a trauma that is overlooked and can happen to anyone, at any time. Although the majority of burn injuries are caused by heat from hot liquids, solids, or fire, the injuries can also be brought on by friction, cold, heat, radiation, chemicals, or electric sources. While energy transfer results in tissue damage in all burn injuries, distinct causes can be linked to various physiological and pathophysiological reactions. Burn injuries cause agony and long-lasting physical and psychological damage that affect a person's mental health, quality of life, capacity to work again, and eventually mortality. Burn injuries are still common worldwide despite a decline in high-income nations, with 90% of burns happening in low- and middle-income regions (1). Burns are a public health problem that causes over 180 000 fatalities worldwide each year. Furthermore, it is widely known and accepted that older burn patients have worse outcomes and a higher fatality rate than younger patients with comparable burns. Geriatrics are more likely to suffer from burn injuries, which may be partly due to eyesight problems and poor coordination that limit their mobility. Furthermore, co-morbidities and weakened immunity provide challenges for the aged. Compared to the younger adult population, geriatric burn patients show higher rates of death and morbidity after a burn injury. Age continues to be a significant predictor of in-patient death among burn victims, with effects on survival lasting for up to two years following the burn (2).
People of all ages are susceptible to burn injuries, which are a substantial source of trauma worldwide. In comparison to the age distribution of the general population, burn injuries occur at higher rates in older adults. The thinner, more atrophic skin of older people, which causes deeper, more serious burns that take longer to heal, is an aggravating factor. Schematic cross-section of aging skin is illustrated in (Figure 1). Age-related physical weakness, slower reaction times, abuse, and neglect have also been proposed as factors in geriatrics heightened susceptibility. The notion that older people are more active than previously believed and are taking part in activities that could result in a burn injury could also be the cause of this overrepresentation. The age threshold for an older adult or geriatric varies in earlier literature, but 65 years of age is the most often accepted definition. According to the World Health Organization, 65 is the lowest age at which the terms older adult or elderly are most commonly used. As per several studies, geriatric burn victims have higher fatality rates than younger patients (3).
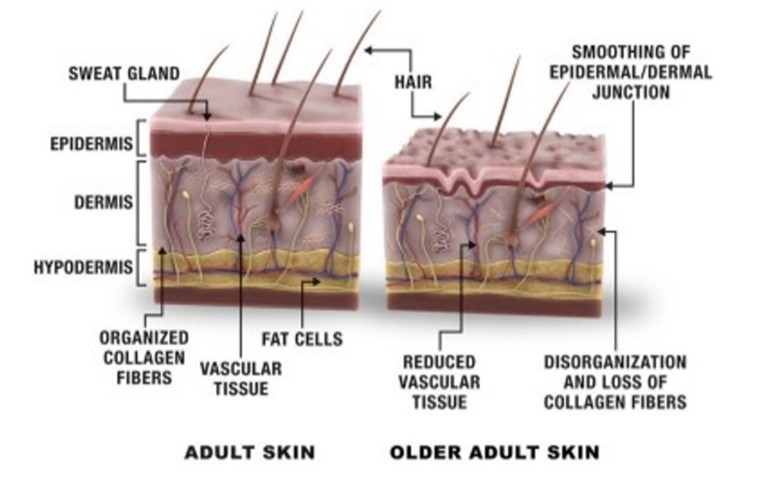
Figure 1: Schematic cross-section of aging skin (15)
Elderly individuals who recover from their injuries have a markedly higher morbidity rate, particularly from infectious sequelae such as pneumonia and others. They have a higher likelihood of spending more time in the hospital, receive home discharges less frequently, and there has been evidence of an increase in the utilization of post-hospitalization resources that is age dependent. Recent developments in burn care, such as resuscitation, early excision and wound closure, nutritional assistance, skin replacements, and regulation of the hypermetabolic response, have increased post-burn survivability. However, the elderly is trailing behind in terms of survival improvements (4). The purpose of this research is to review the available information about geriatric burn injuries: prevalence, management and clinical outcome.
Methodology
This study is based on a comprehensive literature search conducted on November 7, 2022, in the Medline and Cochrane databases, utilizing the medical topic headings (MeSH) and a combination of all available related terms, according to the database. To prevent missing any possible research, a manual search for publications was conducted through Google Scholar, using the reference lists of the previously listed papers as a starting point. We looked for valuable information in papers that discussed information about Geriatric burn injuries: prevalence, management and clinical outcome. There were no restrictions on date, language, participant age, or type of publication.
Discussion
An important epidemiological issue is burn injuries in geriatrics. Burns in older people are linked to greater mortality rates and increased resource use. Over the past 50 years, improvements in burn care have significantly reduced mortality rates, making survival even in patients with severe injuries now a given. Despite the fact that all age groups have shown advances, geriatrics still have worse survival rates than younger cohorts. There is growing interest in better understanding of the epidemiology and effects of injury in geriatrics as this population segment grows. Burn injuries in elderly persons has been the subject of many single-center research studies. However, due to patient characteristics, injury patterns, and management techniques that may be particular to each center, data from individual centers may not be generalizable to all geriatrics. Furthermore, the quantity of burn injuries in elderly patients treated at a single facility may be insufficient to permit meaningful analysis and the creation of efficient intervention strategies (5). Burn severity, treatment, and results are significantly impacted in geriatric burn patients due to significant physiological differences between them and younger adult burn patients. Geriatrics experience burns that are initially deeper than those suffered by younger patients, as measured by a larger ratio of full-thickness total body surface area (TBSA)/TBSA burnt, but they also experience slower healing of their burns and donor sites. Other clinically significant characteristics that hinder the elderly's ability to heal from burns include more severe comorbidities, the related polypharmacy, decreased physiological reserves, and malnutrition (6).
Prevalence
Burns are among the most severe types of traumas that can occur. Elderly burns are rare in developing nations, making up fewer than 5% of burns in South Asian and Middle Eastern nations, whereas they account for nearly 20% of burns in economically developed nations like the United States. The geriatrics are more susceptible to burn injuries than other age groups, and their fatality rates and severity of sequelae are also higher (7). Li. Et al. demonstrated in their findings that geriatrics burn incidents have been steadily declining, from 4.35% in 1999 to 3.81% in 2006. Geriatrics burns can occur at any time of the year, but they seem to happen more often in the summer and winter. Geriatric burns were involved in daily activities in 70% of the cases. The results of the burns were influenced by the co-morbid diseases among the elderly, who made up 83.9% of the casualties. There was no difference in morbidity between patients in rural and urban areas. However, mortality was 30% higher than TBSA burns in rural patients, which was noticeably higher (8). Contrary to this Wang et al. revealed in their study several studies have found rising patterns in burn admissions or burn incidence rates among the elderly. In the second 5-year cohort including years 2014-2018, compared to the first 5-year cohort with years 2009–2013, there were more geriatric patients with severe burns (10.7% versus 7.1% of all patients with severe burns) because of the old population's rapid rise and susceptibility to harm, there are now more geriatric patients with serious burns than ever before. The primary demographics for geriatrics burn prevention are men between the ages of 60 and 69. Flame and flash burns were the most common types of serious burns in older patients, while the summer and winter were the most common seasons for burns (9).
Results of a 7-year-old retrospective analysis showed that the majority of the 693 geriatric burn patients included were male (60.75%) and aged 60 to 69 (56.85%). In December–March and June, burns reached their peak. Flame was the most frequent cause of burns, accounting for 51.95% of all cases, and it predominated among burn patients between the ages of 60 and 69 as well. The median TBSA was 5%, and the most frequent anatomical sites of burns were limbs accounting in 69.41% of cases (10). Findings from Wong et al. study showed that 59 geriatrics were identified from the medical records, with 42% of them being 75 or older throughout a six-year period. The ratio of men to women was 1:1.68. The majority of injuries, almost three-quarters, occurred at home. Scalds made up two-thirds of the burns (11). Tracy et al. reported in their study findings that during the study period, 2394 geriatrics with burn injuries were admitted, making up about 13.4% of all adult admissions. The most frequent type of burn injury in older persons was scalds. Each year, there was a 2.96% rise in the incidence of burns in older adults (incidence rate ratio: 1.030; 95% confidence interval: 1.013-1.046; P< 0.001). The percentage of older adult patients who underwent surgery was lower than that of the younger individuals, but a greater percentage of them underwent skin grafts (3).
Clinical outcomes and management
Results of a 17-year-old retrospective analysis demonstrated that patients over the age of 70 make up a modest 8.6%, yet important portion of burn patients. Even for low percentage TBSA burns, this cohort has higher overall ICU admissions, days on the ventilator, ICU stays, in-hospital mortality, and overall mortality rates. The risk of mortality increases with the presence of smoke inhalation (12). Results of a multicentre database study showed that at the time of discharge, patients in all age groups had significant deficits in their scores on the Short Form-36, the Functional Independence Measure, and the Brief Symptom Inventory among 737 patients who were 55 years of age or older. For patients aged 55 to 74 years, recovery of physical and psychosocial functioning was greatest from discharge to six months, and for patients 75 years of age or beyond, it was greatest at one year follow-up. Geriatrics functional outcomes and psychosocial quality of life are both profoundly impacted by severe burn injuries. The impact, however, and recovery paths appear to be age-related. The greatest possible recovery for older persons may be facilitated by rehabilitation programs lasting up to a year after injury (13).
Palmieri et al. reported in their study findings that the average patient was 72.3 years old, had a 7.8% TBSA burn, and stayed for 11.2 days. The majority of patients were sent home or to a skilled nursing facility. The average time between being discharged and administering the survey was 46.1 months. Compared to 58% of patients who were referred to a skilled nursing facility, 24% of patients who were sent home died soon after being discharged and before being interviewed. In a multivariate analysis, mortality increased with age and government insurance but decreased with discharge to Functional Independence Measure and Short-Form-12 scores did not differ between groups. There is a significant long-term death rate among elderly burn survivors after discharge. Post-discharge mortality was higher for patients who were admitted to a skilled nursing facility or received government insurance (14). Studies have shown that older patients have a decreased ability to recover from burn injury when compared to younger patients because of physiological changes such as changes in nutritional and metabolic status and anatomical changes including dermal thinning caused by aging. Geriatrics are more vulnerable to severe burn injury involving deep-partial thickness and full-thickness, which is associated with high morbidity and mortality. This is because they have worse vision, less coordination, comorbidities, and medication-induced side effects (15).
When examining the current treatment plans used for elderly burn patients, persistent discussions about surgical and intensive care standards are present. Thoughtful consideration of important factors such physiological age, pre-burn functional state, and premorbid diseases, as well as trends toward a moderate, non-aggressive resuscitation approach, appear to be good suggestions for interdisciplinary treatment options. The amount of body surface area operated in a single session after receiving a surgical treatment order should be tailored to the patient's overall condition. Improved therapy alternatives have helped to lower mortality rates even in the elderly during the past few decades, despite geriatric burn victims having a reported greater fatality rate than younger patients. A thorough rehabilitation program needs to receive more attention as a result of the improved outcome (16). Allorto stated that there are guidelines for resuscitating acute burn injuries of more than 10% to 15% of TBSA, and prophylactic antibiotics should not be given to patients with acute burns as the prevention of infection should take priority. First aid should include cooling the burn with cool running tap water up to three hours after the injury Burnshield may be used if cool running water is not available including good wound cleaning and the use of topical antimicrobial dressings. While taking into account additional conditions including neuropathic pain, anxiety, and depression, a standardized strategy to pain treatment with an incremental pharmaceutical approach should be used (17).
There are two concepts on how to manage burns in older patients: the traditional method of limiting physiologic stress by avoiding surgical intervention in the early post-burn stage, and the novel theory of eschar excision and wound closure during the first week of hospitalization (18). One of the pillars of contemporary burn care is the creation of efficient fluid resuscitation regimens, which has most significantly increased patient survival. It seeks to prevent reduced tissue perfusion, multiple organ failure, sepsis, and mortality, and it has been demonstrated that the primary objective of optimizing cardiac preload overestimates the fluid requirements in burn patients. Burn resuscitation guidelines come in a variety of forms. The Parkland formula, as defined by Baxter, is still the most popular, despite the fact that there is still disagreement over the ideal resuscitation fluid composition and regimen. Acute renal failure and hypovolemia should be avoided by titrating enough resuscitation in order to minimize burn depth conversion, pulmonary edema, abdominal compartment syndrome, and the phenomenon of fluid overloading referred to as fluid creep. Various strategies have been used in an effort to prevent this resuscitation hazard, including colloid rescue, reducing the administration of opioids, implementing fluid resuscitation protocols, and close loop computer-driven protocols (7). Surgical and medical interventions for the management of burns in geriatric population remains debatable also the epidemiology and prevalence are variable hence demanding further clinical population-based research additionally the studies available in the present literature addressing burn injuries in geriatrics are quite limited.
Conclusion
In need of specialist burn care, elderly people represent a fragile, growing, and medically demanding demographic. Inferior clinical outcomes are the result of poorer surgical management in the elderly due to etiology, comorbidities, physiological variations, and pre-hospital care. Further research can be beneficial in developing effective management strategies to improve outcomes and quality of life for geriatric burn patients.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
