Volume 2, Issue 11
November 2022
Smoking and infertility in Saudi Arabian Males: A Systematic Review
Jehad Qutub, Mohammed Shareef, Bandar Abu Murad, Abdullah Alsadiq, Saleh Al Dakhil, Nawaf Alofi, Hani Alharbi, Khalid Alduraibi, Slwan Mohammed, Ahmad Aboukhshaba, Sara Bu zaid
DOI: http://dx.doi.org/10.52533/JOHS.2022.21121
Keywords: infertility, smoking, tobacco, Saudi Arabia, systematic review
Tobacco smoking is now increasing rapidly throughout the Arab countries and is one of the biggest threats to current and future world health. The negative effect of cigarette smoking on the quality of semen has been examined in numerous research. In Saudi Arabia, the overall number of couples consulting infertility clinics is on the rise. This systematic research aims to investigate the impact of smoking on the hormonal profile and semen parameters of Saudi Arabian male patients visiting infertility clinics. Online databases were searched for pertinent English publications that met the inclusion and exclusion criteria of this research (Cochrane library, PubMed, EMBASE, and Google Scholar respectively). Semen parameters (volume, count, motility concentration, pH, morphological and hormonal parameters), morphological abnormalities, and reproductive hormones were all evaluated as clinical endpoints. Finally, we looked at 6 studies that met the inclusion and exclusion standards of this study and were incorporated into the systematic review. The studies enrolled participants from 2004, including 1236 infertile male subjects, 41.54% smokers, and 58.45% non-smokers. Two included studies observed a significant reduction in semen volume, three studies observed a significant reduction in sperm motility, four included studies found a significant reduction in sperm count, and one study each reported a significant reduction in sperm abnormal forms and semen pH respectively in comparison to smoker and non-smoker infertile patients. Overall findings demonstrated a considerable negative impact of smoking on semen parameters. In conclusion, concerning the clinical endpoints that were studied in this analysis, tobacco smoking is found to be associated with a lower testosterone level, semen volume, sperm motility, sperm count and concentration, and an increase in the number of morphological defects or abnormal sperm forms in Saudi Arabian infertile men.
Introduction
Infertility is characterized as a condition of the reproductive system in which a clinical pregnancy cannot be achieved following 12 months of consistent, unprotected sexual intercourse (1). It is estimated that more than 70 million couples worldwide suffer from infertility, and the majority of them live in developing countries (2). Infertility rates in Saudi Arabia, the UAE, and the wider GCC are on the rise and more than double the global average, according to research, with experts pinpointing the trend to lifestyle choices, dietary habits, and undiagnosed medical conditions. Infertility is a serious health problem with a prevalence of around 19%, which is still neglected in Saudi Arabia (3). Concern over the health impacts of genetics, oxidative stress, smoking, and other factors known to induce sperm DNA fragmentation and infertility has increased over the past few decades (4-7).
Tobacco products, chewing, and smoking are harmful addictions in young males that include a variety of toxic, mutagenic, and carcinogenic substances in addition to nicotine, and have been linked to poor sperm quality and, as a result, primarily male infertility. Women exposed to high levels of passive smoking have an increased risk of experiencing infertility (8). Healthcare systems around the world are burdened by smoking, and its addiction is getting worse daily. Smoking has been linked to a myriad of adverse health outcomes that are already well known, including cardiovascular disease, respiratory disease, and cancer of the lungs, bladder, cervix, esophagus, kidney, pancreas, and stomach (9). More recently, researchers have begun to explore the relationship between cigarette smoking and reproductive health. However, recent research has revealed that smoking has devastating effects on reproductive health regardless of gender.
Nowadays, One of the main contributing factors to male infertility is tobacco usage (10), and current surveys indicate that over 120 000 young men in the United Kingdom between the ages of 30 and 50 are unable to conceive as a result of this vice. Male infertility, which accounts for 50% of infertility cases in couples (11) eventually causes despair and other psychological effects, which may be warning indicators of more severe future effects. Rarely has the effect of smoking on semen quality been systematically investigated. We, therefore, therefore, sought to thoroughly review the studies which analyzed the effects of tobacco use on the quality of the semen in male participants who were infertile by defining the parameters based on World Health Organisation (WHO) guidelines and comparing semen parameters between smokers and non-smokers.
Methods
Definition of outcomes and inclusion criteria
Outcomes will be extracted from studies conducted on male infertile patients compared the semen parameters of infertile smokers and non-smokers. The following clinical outcomes were reported by the studies: Semen parameters (semen volume, count, concentration, motility, and pH), morphological flaws in spermatozoa, and reproductive hormones were all evaluated as clinical objectives.
Search strategy
Online databases such as PubMed, Google Scholar, EMBASE, and Cochrane library were searched for relevant articles that satisfied the pre-determined inclusion and exclusion criteria. The terms ‘male infertility, ‘male’, ‘infertile men’, ‘smoking’, smokers, ‘non-smokers’, ‘semen parameters’, ‘semen’, ‘smoking and infertility’, ‘sperm count’, ‘sperm motility’, ‘sperm concentration’, ‘sperm morphology’, ‘testosterone’, ‘Saudi Arabia’, ‘Kingdom of Saudi Arabia’ were used to find relevant publications. The phrases "males," "men," "cigarettes," "nicotine," "tobacco," and "non-fertile" were also included one at a time in the search process in order to improve it. Reference lists of appropriate articles were also checked for pertinent publications.
Screening and extraction
Articles whose titles weren't pertinent were disqualified. The full text and abstracts of papers were examined in the second phase to include those that met the inclusion criteria. The titles and abstracts were organized, evaluated, and checked for duplicate entries using reference management (Endnote X8). We used a double screening technique to maintain outstanding quality throughout this key stage, with one screening used to analyze titles and abstracts and the other to assess entire texts. After ensuring that all significant articles were included, an organized extraction sheet that was relevant to our targeted outcomes was made. The page listed the desired outcomes as well as the baseline characteristics. Study design, the total number of smokers and non-smokers, and source were the baseline characteristics.
Quality assessment
We used the modified Newcastle-Ottawa scale (NOS) for cross-sectional studies and cohort studies (12), which primarily consists of three primary domains: the quality of methods, compatibility, assessment, and reporting of the results. Each category is given a maximum of five, two, and three stars on this scale, respectively. Power estimates, sequential participant selection, and recruiting bias were used to evaluate the selection. Studies that made adjustments for either participant age or other risk factors such as varicocele, and diabetes were used to create comparability. It is generally agreed that research with little chance of bias should be given a maximum of five stars. On a scale of 0 to 10, studies were classified as poor studies (0–4), satisfactory studies (5–6), good studies (7–8), and very good studies (9–10).
Results
Search results
We were able to uncover a total of 285 citations using the previously specified search techniques, which were subsequently reduced to 223 after duplicates were eliminated. Only 18 citations remained after the title and abstract screening that qualified for the following stages. Only 6 articles met our inclusion and exclusion criteria after the full-text screening. Figure 1 displays the thorough search and screening procedure.
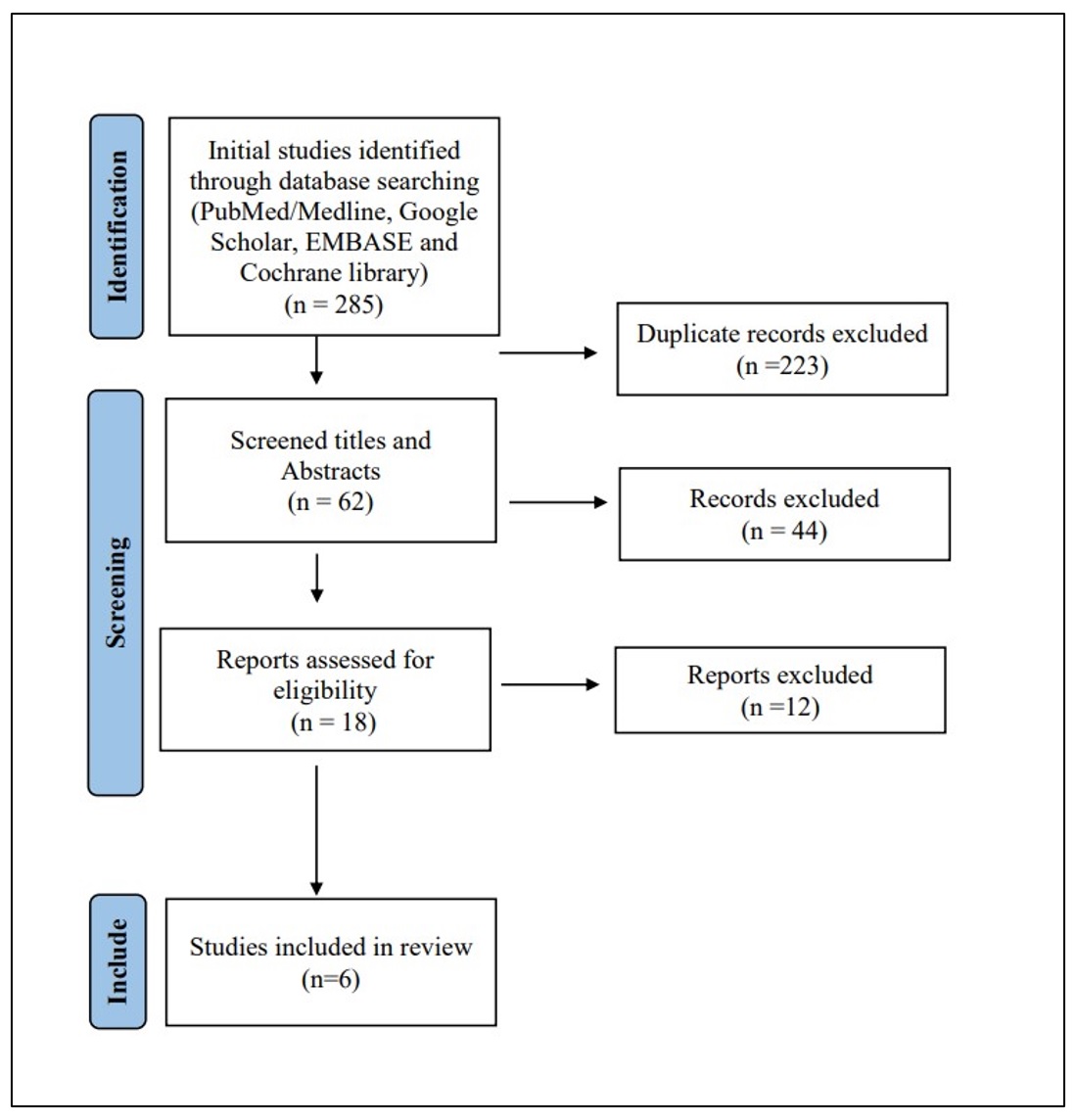
Figure 1: PRISMA flow chart of the included studies
Results of quality assessment
The majority of the included research had satisfactory quality and a low risk of bias, according to our assessment of bias, while the remaining two studies produced good and satisfying results. None of the listed research produced unacceptable outcomes (Table 1).
|
Table 1. Summary of the results of bias assessment of the included studies NOS for non-randomized observational studies |
|||||
|
Studies |
Selection |
Comparability |
Outcome |
Total Score |
Study Quality |
|
Al-Turki et al. |
*** |
** |
** |
7 |
good |
|
Hussein et al. |
*** |
* |
** |
6 |
satisfactory |
|
Al-Turki et al. |
*** |
* |
** |
6 |
satisfactory |
|
Alenzi et al. |
*** |
** |
** |
7 |
good |
|
Kumosani et al. |
*** |
* |
** |
6 |
satisfactory |
|
Obaid et al. |
*** |
* |
** |
6 |
satisfactory |
Characteristics of the study included
Finally, we examined 6 studies that satisfied the eligibility criteria of this investigation and are included in this systematic review. The studies enrolled participants between 2004 and 2022, including 1236 infertile male subjects, 41.54% smokers, and 58.45% non-smokers. The mean age of the included male subjects ranged between 32 and 43 years. All of the included research investigations were observational studies, collecting data either prospective or retrospective in nature. Regarding the cities covered by the included studies, Al Khobar was the subject of two studies, while Buridah, Al Jouf, Jeddah, and Riyadh were each represented by a single study. Most of the patients present with primary infertility in clinics. The main characteristics of the included studies have been summarised in Table 2.
|
Table 2. Baseline characteristics of the included studies in this review. |
||||||||
|
Studies |
City |
Study design |
Data collection period |
Number of participants included |
Age (smokers, non-smokers) |
Infertility types |
||
|
Smokers |
Non-smokers |
|||||||
|
Al-Turki et al. |
Al Khobar |
retrospective cross-sectional |
2008 - 2013 |
194 |
322 |
35.3 ± 7.0 |
a88.7%, b11.3% |
|
|
Hussein et al. |
Buridah |
prospective observational |
2009 - 2010 |
50 |
50 |
37.1 (8.3), 39.5 (9.0) |
Smokers: a24, b26 non-smoker: a17, b33 |
|
|
Al-Turki et al. |
Al Khobar |
retrospective cross-sectional |
2010 - 2012 |
90 |
168 |
34.23±7.66, 34.07±7.92 |
Smokers: a75, b15 non-smoker a126, b42 |
|
|
Alenzi et al. |
Al Jouf |
prospective observational |
2009 - 2010 |
100 |
92 |
43.17±1.17, 42.93±1.03 |
NR |
|
|
Kumosani et al. |
Jeddah |
prospective observational |
18 months (publication: 2008) |
38 |
32 |
37.1 ± 1.4, 37.1 ± 1.2 |
NR |
|
|
Obaid et al. |
Riyadh |
prospective observational |
2004 |
100 (total) |
26 - 30 |
NR |
||
a: Primary infertility, b: Secondary infertility, NR: not reported
The major study endpoints such as volume, count, motility, and pH semen parameters have been summarised in Table 3. Two included studies observed a significant reduction in semen volume (12, 13), four studies observed a significant reduction in sperm motility (12-15), four included studies found a significant reduction in sperm count (12, 13, 15, 16) and one study each reported significant reduction in sperm abnormal forms (12), sperm concentration (16) and semen pH (13) respectively in comparison to smoker and non-smoker infertile patients. Overall results showed significant deleterious effects of tobacco smoking on semen parameters.
|
Table 3. Summary of the outcomes of the included studies in this review. |
|||||||
|
Studies |
Sperm abnormal forms (smoker vs. non-smoker) |
Serum testosterone (smoker vs. non-smoker) |
Semen volume (smoker vs. non-smoker) |
Sperm motility (smoker vs. non-smoker) |
Semen PH (smoker vs. non-smoker) |
Sperm count (smoker vs. non-smoker) |
Sperm concentration (smoker vs. non-smoker) |
|
Al-Turki et al. |
NR |
*277.4 ± 189.3 vs. 409.1 ± 381.0 |
2.8 ± 1 vs. 3.1 ± 0.7 |
*30.7 ± 25.2 vs. 39.9 ± 27.4 |
7.4 ± 0.4 vs. 7.4 ± 0.2 |
110.7 ± 104.8 vs. 124.9 ± 142.5 |
NR |
|
Hussein et al. |
*92.34 ± 3.50 vs. 89.42 ± 3.87 |
NR |
*2.012 ± 0.64 vs. 2.52 ± 0.612 |
*25.72 ± 14.71 vs. 37.86 ± 15.32 |
NR |
*28.55 ± 18.64 vs. 44.9 ± 24.75 |
NR |
|
Al-Turki et al. |
NR |
*383.8 ± 239.5 vs. 422.5 ± 139.2 |
*2.8 ± 1.35 vs. 3.08 ± 0.76 |
*31.5 ± 23.1 vs. 40.05 ± 25.43 |
*7.43 ± 0.3 vs. 7.37 ± 0.34 |
*42.15 ± 29.6 vs. 49.86 ± 39.94 |
NR |
|
Alenzi et al. |
14.51 ± 5.02 vs. 14.09 ± 0.45 (Morphology) |
2.83±0.21 vs. 2.33±0.07 |
NR |
NR |
NR |
22.5 ± 5.49 vs. 21.96 ± 6.31 |
NR |
|
Kumosani et al. |
NR |
NR |
2.8 ± 1.9 vs. 2.4 ± 1.3 |
9.8 ± 2.4 vs. 15.3 ± 2.7 |
NR |
*3.0 ± 0.7 vs. 5.3 ± 1.13 |
NR |
|
Obaid et al. |
NR |
NR |
NS |
NS |
NR |
Significant reduction |
Significant reduction |
NR: Not reported; NS: Not significant; *Statistical significance
Discussion
Cigarette smoking has long been recognized as a general health risk. According to a recent comprehensive study in the Kingdom of Saudi Arabia, the incidence of tobacco use among teenagers has increased over previous years, with up to 39.6% of adolescents being found to smoke (17). In Saudi Arabia, numerous research has been conducted to show the negative health effects of smoking as well as the effects of male infertility. As far as we are aware, this is the first comprehensive examination done on the topic of smoking's impact on male infertility in Saudi Arabia. Despite this, many smokers are young and in their prime reproductive years. Semen analysis represents the most basic evaluation of male infertility. The WHO’s laboratory manual for the testing and processing of human semen serves as the current foundation for evaluating semen parameters (18). Smoking is well known to have significant negative effects on sperm quantity, quality, and morphology in the preceding investigation. In our systematic review, we aimed to review and evaluate semen parameters in infertile Saudi Arabian smoking and non-smoking men. Our systemic review aggregated the published evidence on the effect of cigarette smoking on Saudi Arabian infertile men in the period of 2004 to 2022. Our review findings suggest that smoking (tobacco or hookah) has an overall negative effect on conventional semen parameters. Smokers were more likely to experience primary infertility than non-smokers. It was found to be associated with reduced sperm count and sand sperm motility, concentration, and volume and increased abnormal morphology.
Two meta-analyses that evaluated semen parameters demonstrated that smoking has a negative impact on semen parameters and reported these findings. As per Sharma et al. (19), cigarette smoking was linked to decreased sperm motility and abnormal morphology. The other meta-analysis, which included 16 trials, concurred with the earlier research that smoking caused sperm counts to drop and morphological flaws in spermatozoa to increase (20). The outcomes from these two meta-analyses and systematic reviews in terms of sperm motility, sperm count, and sperm morphology were quite similar. Heavy cigarette smoking was found to be associated with subfertility in young Saudi males via decreasing semen quality in a dose-dependent way, according to a cross-sectional investigation of the young Saudi population. Their investigation further revealed that smokers were at a higher risk of developing oligospermia and teratozoospermia compared with non-smokers and that the effect was dose-dependent (21). However, other international research conducted on healthy males rather than individuals with subfertility or infertility was unable to show any discernible detrimental effects of smoking on the quality of semen (22, 23).
According to Hussein et al. (12) included study in this review reported a statistically significant difference between smokers and non-smokers for all semen parameters. Also, they showed that there were no statistically significant differences in semen parameters between men smoking cigarettes or shisha. Furthermore, their investigation revealed a statistically significant negative correlation between smoking index and the percentage of sperm motility (r = -0.38; P = 0.006) and between smoking duration and the percentage of sperm motility (r = -0.32; P = .026). There was also a marginally significant positive correlation between the smoking index and the percentage of abnormal sperm forms (r =0.28; P = .046). Al-Turki et al. (14) found significant evidence that smoking had detrimental impacts on semen parameters in infertile males during five years in Saudi Arabian males attending infertility clinics. They compared 322 non–smoking infertile men with 194 fertile men and reported a significant difference in the serum testosterone and sperm motility. Semen volume, sperm ejaculation, and sperm count were shown to be higher in the non-smoker group even though the analyzed parameters failed to establish statistical significance. In another study conducted by the same author, Al-Turki et al. (14), also concluded that smoking resulted in a dramatic reduction in hormonal levels and semen parameters. In their investigation, they observed that primary infertility was more common in smokers versus non-smokers with P < ?44.0705, and the total serum testosterone level was lower (383.8 ± 239.5 versus 422.5 ± 139.2 ng/dL (0.009 CI< ?9.9415)), serum prolactin level was higher (18.68 ± 13.28 versus 12.85 ± 12.34 ng/mL (0.001 CI < ?0.123)). The mean progressive motility in smokers was 31.5 ± 23.1 compared to a non-smoker’s 40.05 ± 25.43% (0.002 CI< ?3.2962) and the total sperm count was 119.52 ± 114.12 in smokers and 139.71 ± 104.82 million/mL in non-smokers (0.07 CI < 1.4657).
In the al Jaouf region, Alenzi et al. (24), investigated how hookah smoking affected male reproductive dysfunction brought on by varicocele. In contrast to non-hookah smokers with varicocele, hookah use in varicocele patients considerably adversely affected semen parameters such as semen quality and motility. In the hookah varicocele (HV) group (2.83 ± 0.21), testosterone levels were significantly (P = 0.05) lower than in the non-hookah varicocele (NHV) group (2.33 ± 0.07). When compared to the NHV group, which had sperm counts that were higher (22.5 ± 5.49, 14.51 ± 5.02, respectively), the HV groups had lower sperm counts (21.96 ± 6.31), and lower sperm morphology (14.09 ± 0.45). This study primarily focused on the impact of hookah on patients with varicocele who have lower testosterone levels. Furthermore, compared to varicocele patients who did not smoke hookah, prolonged hookah use and the frequency of hookah sessions may have an impact on the reproductive hormone levels and semen analysis.
In particular, Grade III varicocele, which causes reduced sperm motility and a higher proportion of defective sperm morphology, is a significant contributor to male infertility (25). The mechanism behind this is that varicocele reduces testicular blood renewal with a consequent accumulation of toxic substances. Smoking is a major contributing factor to varicocele development and severity. Varicocele potentiates the toxic effects of environmental exposure to genotoxic substances such as those found in smoking (26). Significant rates of Grade II and III varicocele were found in individuals who smoked hookah in Alenzi et al. (24), Patients with varicocele caused by non-smoking have reported having a lot of Grades I varicocele. This finding highlights the possibility that hookah use contributes to the emergence of varicocele-induced male infertility through the influence of semen characteristics.
Tobacco and its toxic compounds lead to excessive production of reactive oxygen species (ROS). The key mechanism responsible for sperm damage is the lipid peroxidation of the spermatozoa membrane caused by ROS. It has been emphasized that due to the abundance of polyunsaturated fatty acids in their plasma membranes, human spermatozoa are particularly vulnerable to oxidative stress-induced destruction by ROS (27). Sperm concentration, viability, motility, and regular morphology all decline as a result (28, 29). It alters the fertilizing capacity of the sperm (30) and reduces antioxidant activity, which has a possible adverse effect on sperm density, motility, and morphology (31, 32). The ROS in tobacco smoking induces lipid peroxidation of the sperm plasma membrane; this is considered to be the key mechanism in inducing sperm damage that leads to decreased sperm viability, sperm concentration, sperm motility, and increased morphological defects (33, 34). In comparison to mainstream smoke, sidestream smoke contains several toxic substances at higher levels, including ROS such as superoxide and hydrogen peroxide (15, 29) as well as cadmium (15, 35). They have also previously been shown to affect semen quality and cause disturbance in sperm acrosome function (28). In somatic cells, Ca2+-ATPase activity was found to be affected by heavy metals, especially cadmium. Cadmium induces extensive membrane damage, including a significant decrease in the activities of membrane-bound ATPases (Na+ /K+ -ATPase, Ca2+-ATPase, Mg2+-ATPase), the indicators of membrane function in testis, lymphocytes, muscle cells, liver, and kidney (36, 37). In one of the included studies, the researchers analyzed the content of metals (magnesium, zinc, and cadmium) and plasma membrane Ca2+-ATPase activity of sperm (15). They discovered that smoking dramatically lowers Ca2+-ATPase activity, which is linked to higher cadmium concentrations and decreased motility, suggesting a relationship between tobacco and sperm motility. Alkaloids, nitrosamines, and cotinine are additional hazardous components linked to smoking; these compounds create reactive oxygen species such as free radicals and peroxides. These species disrupt the DNA in the sperm nucleus' integrity by altering its base composition, breaking DNA strands, and packing chromatin. DNA fragmentation is the result, which can lead to an increase in the aberrant sperm types in smokers (38).
Only one included study assessed sperm concentration between smoker and non-smoker groups significant difference in sperm concentration between the smoker and non-smoker groups was observed. The concentration of sperm in the smoker and non-smoker groups varied significantly. Primary infertility was more prevalent in the smoking group (57%). There was a higher rate of secondary infertility (55%) in the non-smoker group. Male infertility was primarily caused by normal spermatozoa with aberrant semen parameters (18%) in the smoking group compared to asthenozoospermia (27%) in the non-smoker group (16). An earlier meta-analysis has been performed on the effects of smoking on semen parameters that study mainly focused on sperm concentration. Also, Vine et al. (39) conducted a meta-analysis on smoking and male reproduction and showed that the sperm concentration of smokers was 13% lower than that of non-smokers. The authors showed that exposure to more than 10 cigarettes per day reduced sperm concentration by 13% to 17% (40). Smoking is strongly associated with abnormalities in histone-to-protamine transition and with alteration of protamine expression in human spermatozoa. Hamad et al. (41) revealed that patients who smoke possess a higher proportion of spermatozoa with an alteration of the histone to protamine ratio than patients who do not smoke and suggest that cigarette smoking may inversely affect male fertility. A study on the effects of smoking on protamine 1 and 2 transcripts in human spermatozoa was conducted by Hamad et al. (42), showed that smoking has a harmful impact on sperm quality and sperm protamine mRNAs, and these findings will provide fresh proof of smoking's harmful impact on male fertility. Protamine transcript ratios could also be used as a measure of male fertility.
Before the current WHO manual for the evaluation of human semen was published, earlier research had shown that quitting smoking was associated with an improvement in semen parameters. The result of recent studies makes it clear that quitting smoking had a positive impact on sperm concentration, semen volume, and total sperm count (43). However, none of the research we reviewed examined the effects of smoking frequency or cessation on the features of semen. According to studies, Saudi Arabia has infertility rates that are rising and are more than double the global average. Experts attribute this trend to variables related to lifestyle. There was no evidence to support this greater prevalence of infertility. The main risk factor for male infertility is smoking, and it is becoming more prevalent today than in previous years. Then, we think there is a lot of work to be done. One of the most crucial initiatives will be to encourage young Saudi Arabians to give up smoking to raise fertility rates as well. It is advised that smokers who are receiving fertility therapy give up smoking to increase their chances of having children.
Strength and limitation
To the best of our knowledge, this is the first comprehensive analysis of how smoking affects Saudi men who are infertile. The fact that there was significant heterogeneity among the research endpoints that were included may be a limitation. This can be a result of the observational data being used. Although randomization is not an issue with observational studies, the selection of controls may lead to bias. Another limitation refers to the quality of included studies, which also varied. For more conclusive evidence, more studies with similar endpoints are needed. Not all of the included studies contained information on aspects including the length of infertility as well as related issues such as genital infections, varicocele, and environmental factors. For instance, not all risk factors such as participant age, use of medication, and obesity, which might have affected semen quality, were consistently reported.
Conclusion
In conclusion, the clinical endpoints examined in this investigation showed that smoking increased morphological abnormalities and was related to decreased sperm counts in Saudi Arabian infertile men. Additionally, in this cohort of infertile males, the production of testosterone hormones related to reproduction was impacted. It is advised that smokers who are receiving fertility therapy give up smoking to improve their fertility.
Disclosure
Conflict of interest
There is no conflict of interest
Funding
No funding
Ethical consideration
Non applicable
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
