Volume 2, Issue 11
November 2022
COVID-19 Patients with Tension Pneumothorax: Four Case Reports
Lamees Alsulaim, Osamah Sobh, Ghadah Alodhaybi, Leenah AlQarawi, Renda Alhabib, Deema AlMarzoogi, Rawan Almutairi, Beshair AlMansour, Marwa Elmaghrabi
DOI: http://dx.doi.org/10.52533/JOHS.2022.21107
Keywords: Bullae, COVID-19, SARS, pneumothorax, pneumonia
Severe acute respiratory syndrome Corona virus 2 (SARS-CoV 2) was initially identified in December 2019 in Wuhan, China. The coronavirus disease (COVID-19) spread rapidly worldwide to become a global pandemic. Patients infected with this virus presented with fever, cough, shortness of breath, diarrhea, abdominal discomfort, and myalgia. Radiological examination of those patients revealed numerous findings like consolidation, ground glass opacity and can lead to lung collapse. Other uncommon features are presented such as pneumomediastinum, pneumothorax and lung cavity. Pneumothorax was one of the fatal complications mentioned in the literature as it increased the mortality of COVID-19 patients. We report four cases presented to the intensive care unit (ICU) with severe pneumonia complicated during the admission by pneumothorax, which mandated intervention by chest tube to stabilize the patient's condition. There were differences in age, sex, the treatment protocol used and the timing of the development of the pneumothorax. Pneumothorax should be kept in mind in patients admitted with pneumonia secondary to COVID-19, as it causes acute deterioration of the patient and needs urgent intervention.
Introduction
The outbreak of coronavirus disease 2019 (COVID-19) viruses caused a global pandemic. It can lead to various respiratory complications including pneumonia. Furthermore, many cases may develop extra-pulmonary complications secondary to pneumonia such as pneumothorax. Pneumothorax which is defined as the collection of air in the plural cavity considered a potentially fatal complication in intensive care patients (1). In the previous Severe Acute Respiratory Syndrome (SARS) outbreak, which was caused by a different variant of the coronavirus, the risk of pneumothorax in mechanically ventilated patients was between 20-34% (1). There were many case reports representing the presence of pneumothorax in COVID-19 patients even in the non-diseased lung. Roughly, 1% of COVID-19 pneumonia develop pneumothorax, and this occurs even with no pre-existing lung disease (2). However, the presence of pneumothorax does not lead to poor prognosis (2, 3). In this case series, we are presenting four patients who were admitted with COVID-19 pneumonia and developed tension pneumothorax during the hospital course.
Case Presentation
Case 1
A 38-year-old male, diabetic on oral hypoglycemic agents, and smoker of one pack daily with a body mass index of 22.9 was presented to the emergency department (ED) with a five-day history of fever, cough and shortness of breath. His initial vital signs showed a blood pressure of 134/78 mmHg, heart rate 88 pulse/min, respiratory rate 27 breaths/min, temperature 39?C, Oxygen saturation 84% on room air and 95 % with 5 L/O2.
The patient was admitted as a case of COVID-19 pneumonia. After two days, his oxygen requirements increased, and he was transferred to the intensive care unit (ICU) for intubation. The patient was treated according to the protocol with antibiotics, hydrocortisone and antiviral (favipiravir). On the 26th day of ICU admission, he developed persistent tachycardia and an increased requirement for FiO2. Chest X-ray showed a right tension pneumothorax. He was on assisted control mode with a respiratory rate of 15, tidal volume 340 ml, FiO2 50% and a positive end-expiratory pressure (PEEP) of 5. He received the first dose of tocilizumab three days before the new event of tachycardia. After surgical consultation, the surgical team inserted a right chest tube (Figure 1). Afterwards, a computed tomography (CT) was done as the patient deteriorated after two days which showed bilateral severe emphysema and air space disease (Figure 2). The patient developed sepsis and a blood culture revealed Stenotrophomonas maltophilia. However, the sepsis caused multiple organ dysfunction syndrome (MODS) and the patient passed away.
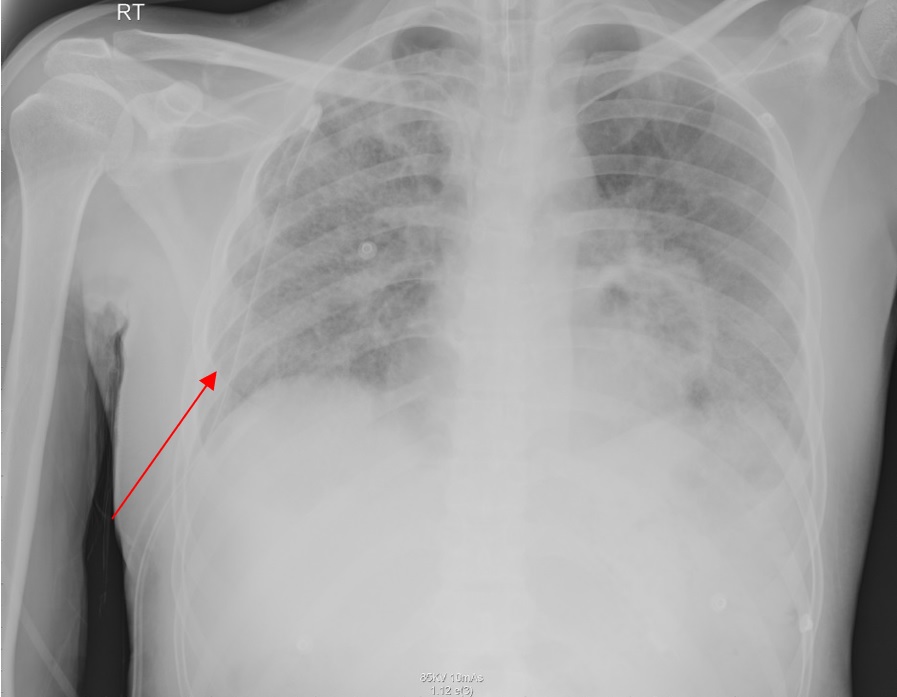
Figure 1: After surgical consultation, the surgical team inserted a right chest tube
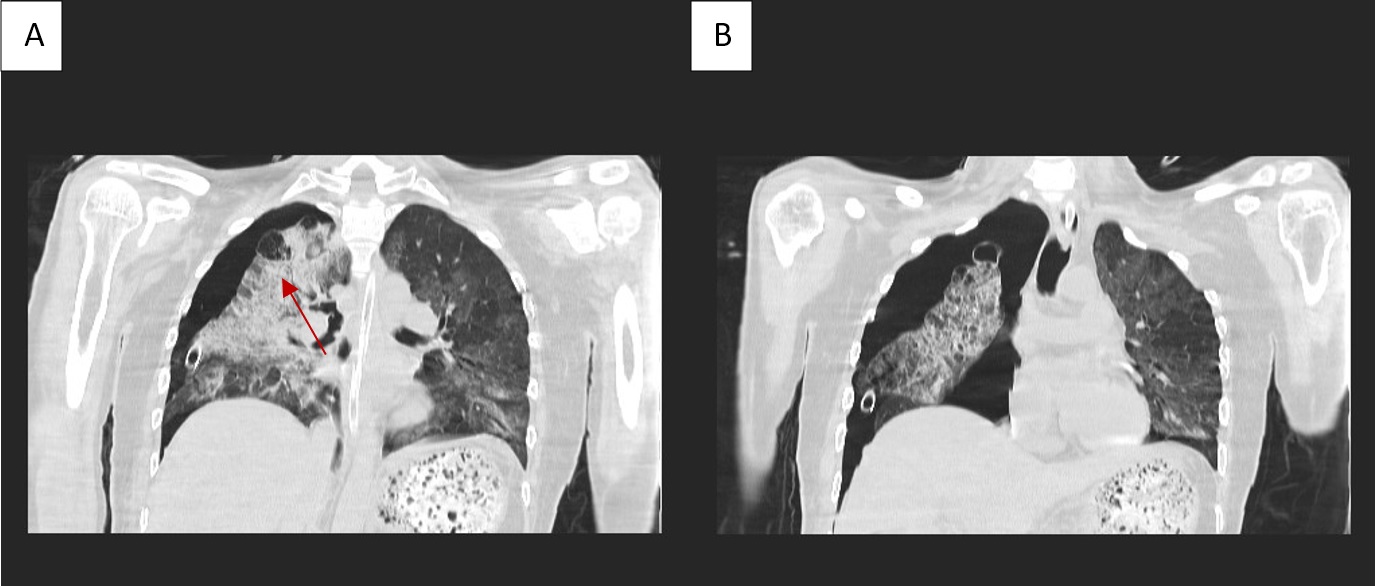
Figure 2: A computed tomography (CT) was done as the patient deteriorated after two days which showed bilateral severe emphysema and air space disease
Case 2
The second case is a 30-year-old pregnant female, gravida 5, para 2 with history of two abortions. She is 22 gestational week and is medically free. She had been complaining of a productive cough and fever for six days. She was being transferred to the ICU from a peripheral hospital. Upon presentation, the patient looked ill, desaturating SpO2 43% on room air after a failed face mask and maintaining her oxygen on BIPAP (bilevel positive airway pressure). She was assessed by an obstetrician for fetal viability, which was normal.
The patient received ceftriaxone, azithromycin and dexamethasone. After three days, the patients started to have sudden tachycardia and desaturated further. She was diagnosed with pulmonary embolism based on an echocardiography finding and was started on heparin infusion, then intubated and put on mechanical ventilation due to refractory hypoxia. A portable x-ray with an abdominal shield showed severe bilateral pneumonia, so the antibiotic was switched to linezolid. The high-risk committee decided, with family agreement, to terminate the pregnancy by induction rather than caesarean section and deliver a dead baby boy, declaring IUFD (intra-uterine fetal death).
After 15 days of admission, the patient improved slightly after received tocilizumab, extubated and face mask was put on. On day 20 of admission, sudden tachycardia and tachypnea developed, and a chest x-ray showed a left pneumothorax, which was treated by chest tube insertion (Figure 3). The patient was later transferred to a tertiary center and was discharged in good health.
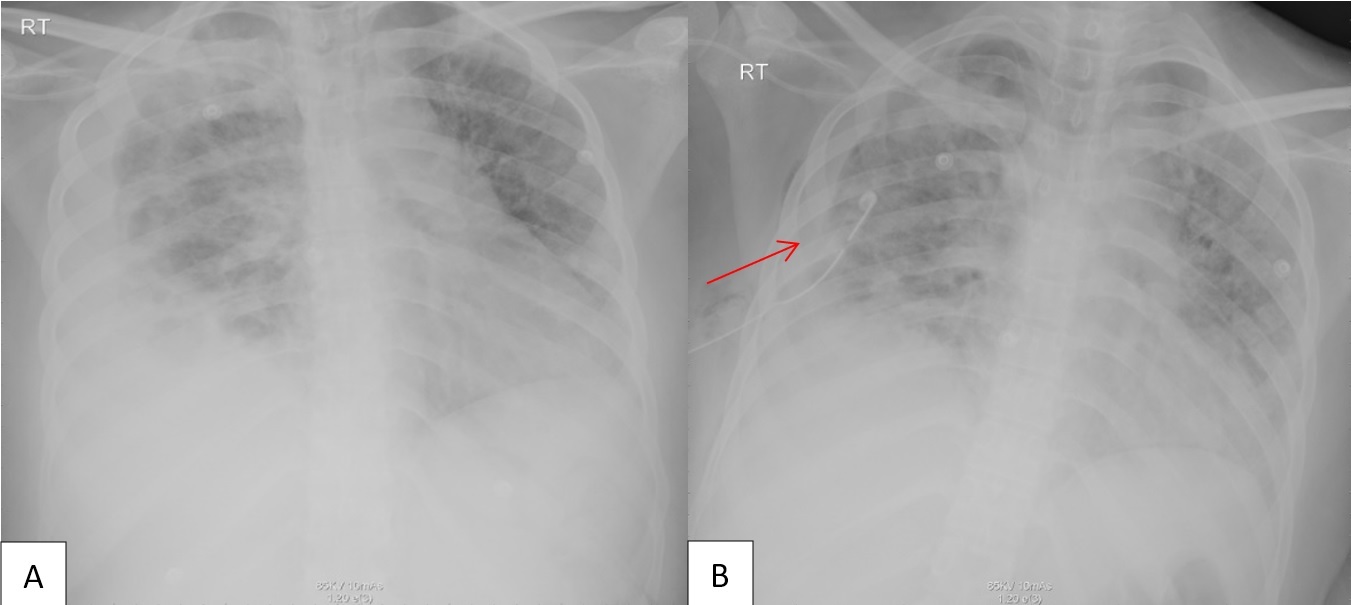
Figure 3: A chest x-ray showed a left pneumothorax, which was treated by chest tube insertion
Case 3
A 70-year-old female was brought by the red crescent to the emergency department as a case of COVID-19 pneumonia after developing fever and cough for five days. She is a known case of diabetes mellitus and is not on regular medication. Her body mass index is 30. Upon admission, her oxygen saturation was 68% on room air. She was started on bilevel positive airway pressure non-invasive ventilation with a PEEP of 5 and FiO2 of 100%. On her second day of ICU admission, the patient was intubated and sedated on pressure-controlled ventilation (FiO2 100% and PEEP 10). On the third day, she had a sudden desaturation drop to 58%. Afterwards, a right tension pneumothorax was diagnosed, and a right chest tube was inserted (Figure 4). Then the patient improved during the admission. She received tocilizumab, hydrocortisone, and a full course of antibiotics, which was guided by the hospital protocol. However, she developed sepsis and MODS and the patient passed away.
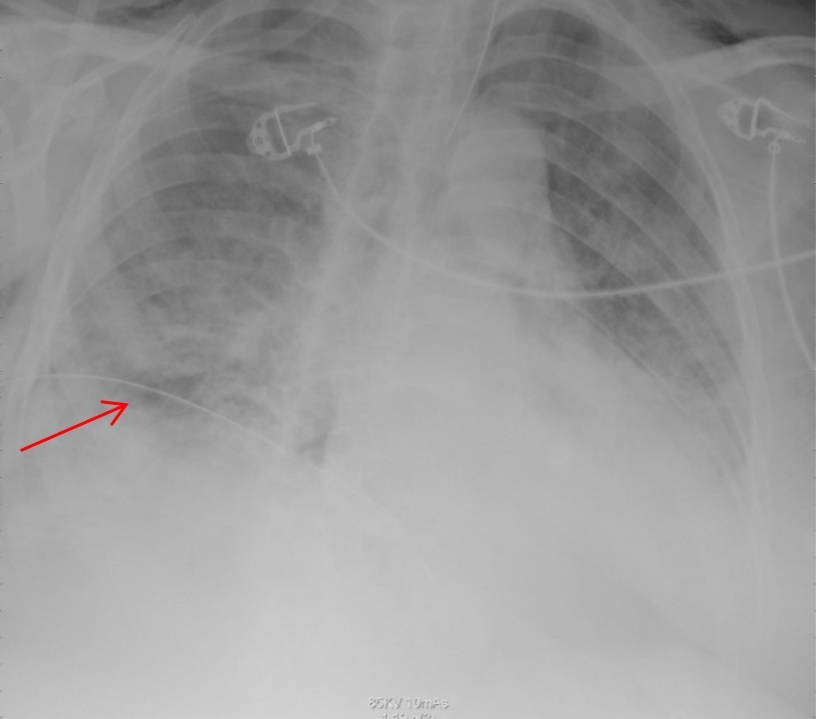
Figure 4: A right tension pneumothorax was diagnosed, and a right chest tube was inserted
Case 4
An 84-year-old-male, diabetic and bedridden for one year due to neurodegenerative disease, with a BMI of 23.9, was brought to the hospital by a red crescent due to shortness of breath and cough that started ten days before presentation. He was initially diagnosed with aspiration pneumonia, but the polymerase chain reaction (PCR) was positive for COVID-19. His vital signs in the ED showed a blood pressure of 135/72 mmHg, pulse 116 beats/minute, O2 saturation of 85% on room air, temperature of 36.6 ?C, and respiratory rate 32. The patient was wearing a face mask, but due to desaturation, he was intubated after the second day of admission and was mechanically ventilated on PEEP 5 and FiO2 100%. He was treated with caspofungine, favipravir and steroids. After 12 days of intubation, the patient desaturated further after developing a left sided pneumothorax (Figure 5). The Patient had a chest tube placed but passed away after developing acidosis and respiratory failure.
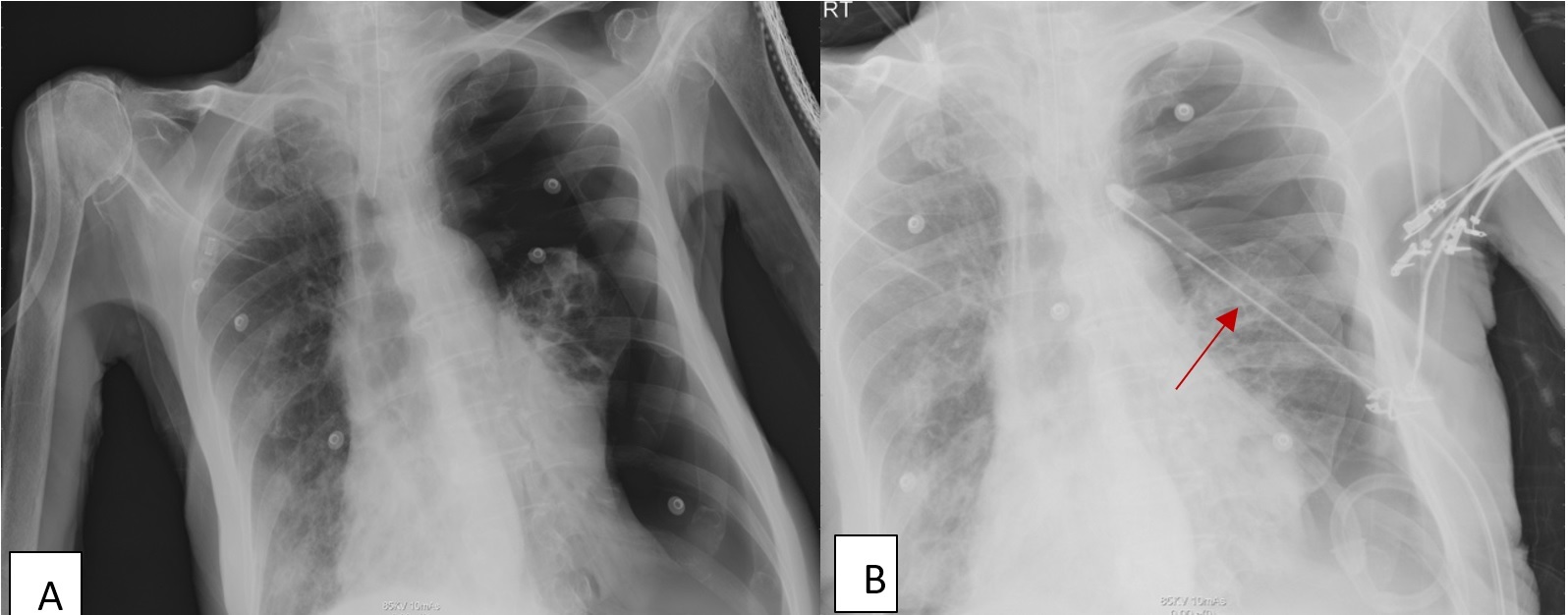
Figure 5: The patient desaturated further after developing a left sided pneumothorax
Discussion
The development of pneumothorax in COVID-19 patients is still not fully understood. One of the suggestive mechanisms is barotrauma after intubation (4). In non-ventilated patients, repetitive prolonged cough is considered a strong factor that can lead to alveolar damage by increasing the intra- alveolar pressure and can result in sub-pleural rupture. In such cases, other risk factors include a history of smoking and previous lunge disease where it can cause the bullae to devolve and develop pneumothorax (5, 6). On a cellular level, the changes of the parenchyma secondary to COVID-19 can play a role. For instance, the disruption of protein, downregulation of surfactant, loss of extracellular matrix and surfactant and hyper-coagulative state can all contribute to developing pneumothorax in COVID-19 patients (7). Shan et al. studied post-mortem patients who died from COVID-19 and reported the presence of desquamation of pneumocyte and hyaline membrane formation which is consisted of the diagnosis of Acute Respiratory Distress Syndrome (ARDS) (6).
According to Yamaya et al., patients with COVID-19 pneumonia can develop pneumothorax as a complication in almost 21 days (4). CT scan is considered as an important tool and strongly recommended in COVID-19 patients. CT scanning in COVID-19 pneumonia is reported as extensive ground-glass opacity with a peripheral or posterior distribution mainly found in the lower lobes. Uncommon findings can include pleural effusion, pericardial effusion, lymphadenopathy, cavitation, CT halo sign and pneumothorax (8).
In the present cases, we found that the presence of pneumothorax in patients with COVID-19 pneumonia can be present at any time of admission whether they were mechanically ventilated or not. Other factors may also contribute to developing pneumothorax include the length of ICU admission, intubation period, especially if barotrauma is present. Furthermore, repetitive coughing may cause progressive alveolar damage which can increase the intra-alveolar pressure (1).
Moreover, male patients are more prone to develop pneumothorax, especially mechanically ventilated patients. Furthermore, ARDS is a predominant risk factor of patients who develop pneumothorax, but in some reviews development of pneumothorax can occur in non-ventilated patients also (2). Ventilated patients with high peak inspiratory pressure greater than 40, PEEP, and high minute ventilation are all at risk for developing predominant even without COVID-19 (2, 3).
Conclusion
Many Differential diagnoses have to be kept in mind such as pulmonary embolism in COVID-19 pneumonia patients. In addition, COVID-19 pneumonia patients are prone to develop pneumothorax which can be associated with barotrauma due to the high ventilation setting.
Acknowledgement
We would like to express our thanks to King Saud Hospital for their support and for our great team.
Disclosure
Statement
The authors declare no conflict of interest
Funding
None
Ethical consideration
Ethics approval and consent to participate and their relative, approval was also obtained from Qassim Health Clusters Ethical Committee NO.1442-1247460
Authors’ contributions
All authors have read and approved the manuscript. All authors have contributed equally to this manuscript.
