Volume 6, Issue 1
January 2026
Eustachian Tube Balloon Dilation in Chronic Otitis Media with Effusion
Ashraf Abdulaziz Abduljabbar, Ahmed Ibrahim Alshanqiti, Abdulaziz Muhayya Alotaibi, Abdulaziz Ahmed Ghunaim, Salah Esam Mogarbel, ?Faisal Ahmad Khaleefah, Abdulrahman Jamal Taha, Alaa Basem Sharqawi
DOI: http://dx.doi.org/10.52533/JOHS.2026.60105
Keywords: Otitis media with effusion, Balloon dilation of the Eustachian tube, Ventilation tube insertion, Eustachian tube dysfunction
Otitis media with effusion (OME) is the occurrence of fluid accumulation in the middle ear cavity without showing any signs of acute infection. It is more common in children and can become chronic in both children and adults. It is caused by ear infection, Eustachian tube dysfunction, or secondary to subclinical bacterial infection. It is characterized by aural fullness, hearing impairment, and the inability to perform the Valsalva maneuver. Ventilation tube insertion is the recommended treatment for chronic OME, combined with adenoidectomy in children. However, it is associated with a high recurrence rate. Balloon dilation of the Eustachian tube (BDET) has shown promising results in the treatment of chronic OME. However, a comprehensive review discussing the role of BDET, either alone or combined with other procedures, is lacking. This review aims to discuss current management of OME in children and adults, focusing on the role of BDET. There is no definitive medical therapy for OME; however, some medications can help alleviate symptoms, such as topical steroids and mucolytics. Although balloon dilation of the Eustachian tube has been widely used in the adult population, there were concerns regarding its use in children. However, multiple studies have emphasized the effectiveness and safety of BDET in the treatment of chronic OME in children. It has shown improvement in various postoperative outcomes, such as clinical symptoms, postoperative otoscopy results, postoperative acoustic impedance, and postoperative pure tone audiometry in both adults and children. Future studies should investigate the use of BDET as first-line therapy for chronic OME in children and adults.
Introduction
Otitis media with effusion (OME) is defined as the presence of fluid in the middle ear without signs or symptoms of acute ear infection. It is common among the pediatric population, with a prevalence of 60% in children under 2 years of age, and thereafter, middle ear fluid begins to dissolve with age (1). After the age of 7, the prevalence of the disease significantly decreases and remains below 20% (2). While in adults, the prevalence of OME is around 0.6% (3, 4). The majority of OME cases resolve spontaneously within 3 months; however, the rate of its recurrence and chronicity can reach up to 40% and 25%, respectively (5). Etiology of OME includes ear infection (acute otitis media), Eustachian tube dysfunction (ETD), syndromes, such as Down’s syndrome and cleft palate (3). It also may occur secondary to subclinical bacterial infection or gastro-esophageal reflux disease (3). Its hallmark manifestations include aural fullness, hearing impairment, and the inability to perform the Valsalva maneuver (6).
Currently, ventilation tube insertion is the recommended treatment for chronic OME with hearing loss in children and adults (4, 7). A concurrent adenoidectomy is also recommended for children older than 4 (4). The ventilation tube insertion procedure enables air to flow from the external auditory canal into the middle ear cavity, bypassing the Eustachian tube, and thereby helping to equalize middle ear pressure with atmospheric pressure (8). Although it has been effective in improving hearing and reducing the prevalence of middle ear effusions, the improvement persists only while the tube stays in place or until normal Eustachian tube function is restored (9). The recurrence rate of OME after ventilation tube insertion is reported to be around 15–20% (10, 11).
Balloon dilation of the Eustachian tube (BDET), also known as balloon Eustachian tuboplasty (BET), was introduced to clinical practice by Ockermann et al. in 2010 (12) and has shown effectiveness in the treatment of ETD. BDET works by applying pressure to the mucous membrane and soft tissues to promote prolonged Eustachian tube patency (13). It is a minimally invasive endoscopic procedure aimed at the dilation of the cartilaginous portion of the Eustachian tube through catheterization. Although BDET demonstrates high success rates, a dependable overall assessment of its outcomes is limited by the methodological heterogeneity across studies (14).
Many hypotheses have been proposed to explain the mechanism behind balloon dilation, including microtears in the cartilaginous part of the Eustachian tube (15), reduction of mucosal inflammation, and diminishing of the biofilm infections burden (13). Reports indicated that BDET can effectively cure OME in both adults and children regardless of its unclear mechanism. Multiple studies have investigated the safety and efficacy of BDET, either alone or combined with other procedures, in the treatment of chronic OME. However, a comprehensive, in-depth review discussing the role of BDET and its contributing role to other treatment modalities in the treatment of OME in adults and children is lacking. The aim of this review is to investigate the current management of chronic otitis media with effusion, with more focus on the use of balloon dilation of the Eustachian tube in adults and children.
Methods
A comprehensive literature search was conducted in Medline (via PubMed), Scopus, and Web of Science databases up to December 2, 2025. Medical Subject Headings (MeSH) and relevant free-text keywords were used to identify synonyms. Boolean operators (AND’, OR’) were applied to combine search terms in alignment with guidance from the Cochrane Handbook for Systematic Reviews of Interventions. Key search terms included: “Otitis media with effusion” AND “Balloon dilation of the Eustachian tube”. Summaries and duplicates of the found studies were exported and removed by EndNoteX8. Any study that discusses Eustachian tube balloon Dilation in chronic otitis media with effusion and published in peer-reviewed journals was included. All languages are included. Full-text articles, case series, and abstracts with the related topics are included. Case reports, comments, and letters were excluded.
Discussion
Management of Otitis Media with Effusion
Multiple treatment methods for OME have been introduced that can be classified into medical methods and surgical methods.
Medical Treatment
Various medical treatment modalities have been investigated in the treatment of OME (Table 1). Otitis media with effusion and associated ETD can be resolved mechanically by various maneuvers, such as Toynbee and Valsalva maneuvers (16). These maneuvers do not need any equipment and are self-administered. Both maneuvers provide similar improvements in middle ear pressures, are of very low cost, and have no side effects (17). Therefore, they are recommended to be used either alone or as an adjunct to medication treatment. Another medical treatment method is the use of intranasal corticosteroids, which suppress the local inflammation in the Eustachian tube and the middle ear. Topical steroids can provide early and short-term symptomatic relief in OME (18). Oral steroids have no role in OME and are associated with various systemic side effects (19).
Mucolytic agents can provide short-term relief in OME symptoms by indirectly alleviating inflammation by decreasing mucus production and increasing excretion of secreted mucus (20). However, these agents are not recommended in the treatment of OME in international guidelines, since studies on mucolytics have failed to clearly establish their cost-effectiveness (7). Oral antibiotics are not typically prescribed in OME, given the nonsterile nature of OME (21, 22). They were not associated with any benefits on OME symptoms, hearing loss, or ventilation tube application rates in the long term (23). Therefore, the use of antibiotics is not recommended in the treatment of OME in international guidelines (7). Furthermore, oral or nasal antihistamines or decongestants have no role in OME treatment, and side effects related to these drugs can be seen at a substantial rate (24). Overall, there is no definitive medical therapy for OME, and both American and European guidelines advise surgical intervention for chronic cases that persist beyond a 3-month period of watchful waiting (16).
|
Table 1. Medical Treatment of Otitis media with effusion |
||
|
Treatment |
Role |
Evidence/Limitation |
|
Valsalva / Toynbee maneuvers |
Equalize middle-ear pressure |
Effective, low-cost, no side effects |
|
Topical intranasal steroids |
Reduce ET inflammation |
Short-term symptom relief |
|
Oral steroids |
Not recommended |
No long-term benefit, systemic side effects |
|
Mucolytics |
Reduce mucus viscosity |
No proven cost-effectiveness |
|
Oral antibiotics |
Not recommended |
No benefit in nonsterile OME |
|
Antihistamines & decongestants |
Not recommended |
No effect, significant side effects |
Surgical Treatment
Ventilation tube insertion (or also referred to as tympanostomy tube) is the key treatment for chronic OME according to guidelines (7). It is indicated in cases of atrophy or retraction of the tympanic membrane associated with an objective hearing loss between 25 and 40 dB on audiometry or with reduced quality of life due to milder hearing losses (25). Ventilation tube insertion is associated with significant improvements in hearing and quality of life during the first 9 months (26). Ventilation tubes inserted into the tympanic membrane enable air to flow from the external auditory canal into the middle ear cavity, bypassing the Eustachian tube, and thereby helping to equalize middle ear pressure with atmospheric pressure. Grommet tubes are preferred in the first line in primary OME surgery (16). The most common complication for the ventilation tube insertion procedure is otorrhea (27). Adenoidectomy can be combined with the ventilation tube insertion procedure for the treatment of OME. Compared to ventilation tube insertion alone, combined adenoidectomy and ventilation tube insertion decrease the risk of OME recurrence and the need for re-insertion of ventilation tube insertion in the 2-year follow-up period, especially over the age of 4 (28, 29).
Balloon Dilation of the Eustachian Tube
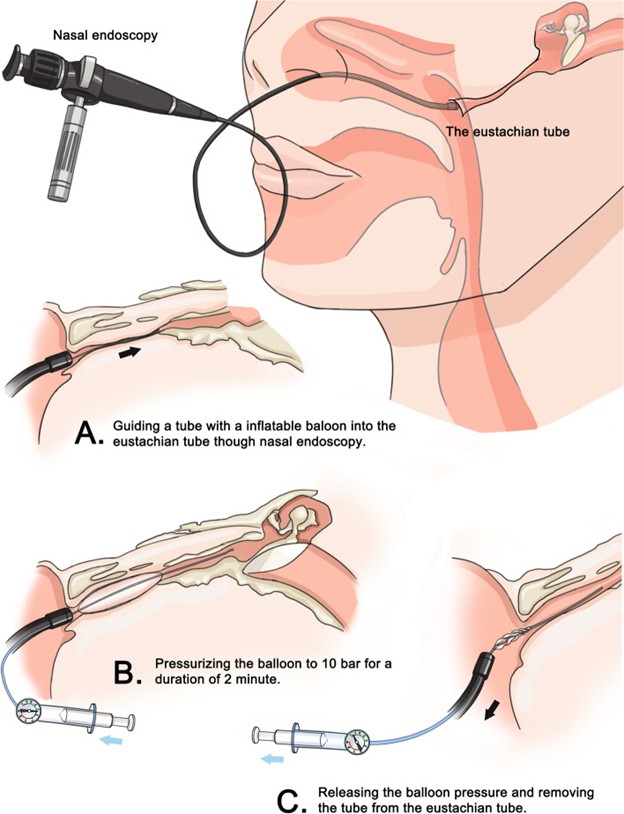
Balloon dilation of the Eustachian tube has shown promising results in the treatment of Eustachian tube dysfunction. This procedure starts with the positioning of an insertion instrument near the Eustachian tube opening; then a balloon catheter is advanced 2 cm into the ET and inflated with sterile water to a pressure of 10–12 bar for 2 min (8, 30) (Figure 1). Following dilation, the balloon is deflated, and the catheter is removed. In most studies, the BDET procedure was performed transnasally under general anesthesia (30-35), while in one instance, only local anesthesia was used (36). BDET procedure has been indicated as a generally safe procedure, with complication rates of about 2%. However, studies have reported potential complications for BDET, which can be classified into major and minor complications (37). Major complications include emphysema and pneumomediastinum, while minor complications include bleeding, hemotympanum, transient tinnitus, rhinitis, dizziness, acute otitis media, and altered tongue sensation due to chorda tympani compression. Various assessment methods for BDET outcomes were used by different authors. Some relied on otoscopic evaluation of the ears before and after the procedure (31, 32, 38, 39), while others compared the results of the Valsalva maneuver (30-33, 36), tympanometry (30-34, 38-40), pure tone audiometry (30, 31, 33, 36, 39), and tubomanometry (31). The impact of BDET on changes in subjective Eustachian tube dysfunction symptoms has also been examined by multiple authors (30, 31, 33-36, 38-40).
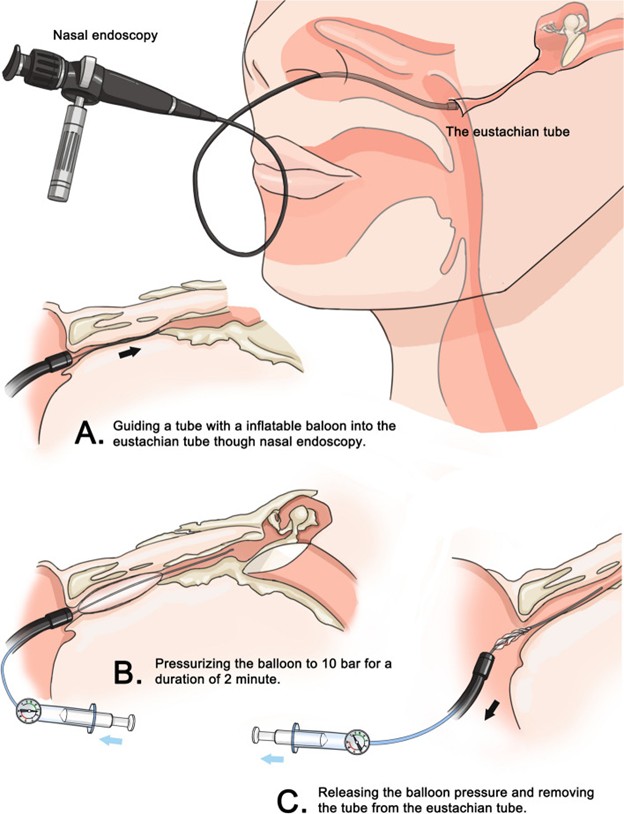
Figure 1: Balloon dilation eustachian tuboplasty procedure (40).
Treatment of Otitis Media with Effusion Using Balloon Dilation of the Eustachian Tube
Balloon Dilation of the Eustachian Tube in Children
Although balloon dilation of the Eustachian tube has been widely and successfully used in the adult population, there were concerns regarding its use in children. Physicians preferred not to use BET for the treatment of Eustachian tube dysfunction due to the presence of an aberrant or dehiscent bony internal carotid canal in children (14). This clarifies a misunderstanding that the balloon remains in the bony canal, whereas it is inflated in the cartilaginous portion of the Eustachian tube and is located at a sufficient distance from the carotid canal (41). However, these concerns have been reduced since Tisch et al. reported a successful balloon dilation of the Eustachian tube in an 18-month-old girl, proving that BET can be used in children (42). Since then, multiple studies have been conducted to emphasize the safety and efficacy of Eustachian tuboplasty in the treatment of Eustachian tube dysfunction in children (43-51). Another concern is the inadequacy of the 20 mm balloon for insertion in children, whose Eustachian tube measures 21.2 mm (52). However, infants have a proportionally longer cartilaginous portion, reducing the risk of the balloon extending into the osseous segment (14, 45). Therefore, correct placement remains generally safe despite shorter pediatric anatomy.
The efficacy and safety of balloon dilation of the Eustachian tube in the treatment of OME in children have also been evaluated. Ma et al. aimed to evaluate the additional benefits of BET when combined with tympanostomy tube insertion (TTI) and ablation of tonsils and adenoids (ATA) to treat chronic OME in children (49). While both treatment approaches showed favorable post-surgical outcomes, the experimental group (BET+TTI+AAI) showed better improvement in clinical symptoms six months after the surgery; better otoscopy results six months after the surgery; a higher proportion of type A tympanograms in the postoperative acoustic impedance; lower air conduction (AC), bone conduction (BC), and air-bone gap (ABG) values in the postoperative pure tone audiometry test; and a higher effective rate (49). These findings highlight the additional value and benefits of adding balloon dilation Eustachian tuboplasty to tympanostomy tube insertion and ablation of tonsils and adenoids in treating chronic OME in children.
Another study by Demir and Batman aimed to evaluate the efficacy of BET as a first-line treatment of chronic OME in children compared with ventilation tube insertion (41). Overall, the study reported higher success rates and better results of hearing tests in the BET group. They found a higher reduction in the ABG in the BET group after the surgery compared with the ventilation tube insertion group (41). Furthermore, cases of recurrent OME were higher in the ventilation tube insertion group. However, both procedures did not lead to the retraction of the tympanic membrane, which was attributed to the duration of the study (41).
The role and safety of BET in the treatment of OME in children were also evaluated by Chen and colleagues (50). The evaluation was done through comparing the outcomes of BET combined with myringotomy and tube insertion procedure with the outcomes of myringotomy and tube insertion only procedure. They found that BET combined with myringotomy and tube insertion is effective and safe for children with OME and that it can effectively extend the improvement period and increase the cure rate compared to conventional myringotomy and tube insertion, especially after the ventilation tube is removed (50). Nevertheless, while the ventilation tube was in place, the outcomes of the two groups were almost the same due to its direct effect.
Balloon Dilation of the Eustachian Tube in Adults
Numerous studies have assessed the efficacy and safety of balloon dilation of the Eustachian tube, either alone or combined with other treatment modalities, in the treatment of OME in adults (32, 33, 53-58). Li et al. aimed to evaluate the effect of BET combined with grommet insertion on the function and the opening structure of the Eustachian tube in adults with refractory OME (54). The study reported that BET and grommet insertion procedure was associated with favorable subjective and objective outcomes and also achieved good results in Eustachian tube function and structure (54). BET and grommet insertion led to a significant increase in the postoperative quantitative examination peak pressure deviation of Eustachian tube function. Additionally, this procedure was associated with a lower pure-tone auditory threshold and air-bone gap than those before surgery, with no significant difference in the pure-tone auditory threshold between 3 and 6 months postoperatively (54). However, long-term follow-up showed a degree of deterioration in the Eustachian tube function and hearing outcomes in a few cases, but overall BET combined with grommet insertion enlarged the Eustachian tube, improved active and passive opening, and is an effective treatment for refractory OME (54). These findings are consistent with the findings of other related studies with the same aim (56, 57).
The use of combined BET and tympanocentesis in the treatment of adults with OME has been evaluated by multiple studies. Formankova et al. compared the efficacy of BET with concurrent tympanocentesis to BET alone in adults with chronic OME (33). This study, along with other related studies, showed that BET alone can be sufficient in the treatment of OME and that BET is more effective than tympanostomy alone or no treatment (32, 59, 60). In addition, owing to their strong anti-inflammatory capacity, studies have examined the use of corticoids, especially methylprednisolone, to reduce the mucosal inflammation, thus improving balloon dilation of the Eustachian tube efficacy. Si et al. evaluated the effects of methylprednisolone irrigation on the outcomes of BET when used in the treatment of OME in adults (58). One-month post-dilation histopathology showed normal mucosa in BET and tympanic paracentesis with methylprednisolone irrigation group. The same group also showed the best improvement in the Eustachian tube function (58). Intratympanic irrigation with methylprednisolone can maximize the clearance of middle-ear fluid while allowing the steroid to exert potent anti-inflammatory and anti-edematous effects within the middle ear.
Clinical Implications
Surgical treatment is the definitive treatment for chronic otitis media with effusion. Ventilation tube insertion is effective in the treatment of OME; however, it has been linked to recurrence of OME. Balloon dilation of the Eustachian tube is associated with a higher effective rate and leads to improvement in clinical symptoms, postoperative otoscopy results, postoperative acoustic impedance, and postoperative pure tone audiometry in both children and adults, especially when combined with ventilation tube insertion. BDET alone can achieve similar improvements; however, it needs more validation by future studies. Reports indicated that it can be used as first-line therapy for chronic OME. Multiple medical treatment modalities can help alleviate symptoms and improve outcomes, including maneuvers, such as the Valsalva maneuver, topical steroids, and mucolytic agents.
Conclusion
Otitis media with effusion is one of the most common causes of hearing loss in children and has a considerable risk of chronicity in adults. Balloon dilation of the Eustachian tube has shown safety and effectiveness, either alone or combined with other procedures, in the treatment of chronic OME. Future studies should investigate the use of BDET as first-line therapy for chronic OME in children and adults.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical consideration
Non applicable.
Data availability
All data is available within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.