Volume 5, Issue 12
December 2025
Establishing Patient Care Technician Services to the Delivery of Safe, Patient and Family Focused Quality Care
Cathariena Magrietha Uys, Zalikha Attar,Ragdah Fouad Nazlawy, Amani Bakr Tunusi, Rawan Tarik Bakalka, Sammah Jaha, Erwin Garcia Bolante, Abegail Corteza dela Cruz, Agnies Alviola, Majed Mohammed Alyasi, Essam Ali Alghamdi
DOI: http://dx.doi.org/10.52533/JOHS.2025.51205
Keywords: Patient care assistant, patient care technician, Saudi Commission for Health Specialty requirements, nursing resource availability
Background: Worldwide, healthcare systems are facing substantial deficits in the nursing profession, driven by increasing patient demands, an aging workforce, and higher turnover rates. Saudi Arabia is affected by this dilemma, as recent reports indicate a continuous disparity between the supply of registered nurses (RNs) and the increasing demand for healthcare services, especially in acute care environments. This shortage has contributed to increased workloads, staff burnout, and potential risks to patient safety and care quality.
Local problem: The implementation of new staffing approaches is essential due to the nationwide shortage of RNs. The introduction of the Patient Care Technician (PCT) recruitment initiative at King Fahd Armed Forces Hospital in November 2022 has had a positive impact on the delivery of high-quality, patient-centered care that prioritizes patient and family safety.
Methods: This quality improvement project was guided by the IHI model for enhancement. We obtained data regarding registered nurse overtime, turnover, and satisfaction from hospital databases and surveys. We employed descriptive analysis to examine the results and utilized charts to illustrate trends and effects.
Interventions: A needs analysis was conducted to identify departments with the greatest needs; subsequently, new PCT positions were established, accompanied by the development and implementation of an orientation program. Performance evaluations were utilized to evaluate PCT readiness following the probationary period.
Results: By July 2024, 93 PCTs (77 females and 16 males) had been integrated into inpatient, outpatient, and emergency departments, representing 7.5% of the total staff. The integration led to a 9.5% reduction in overtime hours for RNs, significantly exceeding the 5% target. This reduction translated into projected annual savings of approximately 1.5 million Saudi Riyals in overtime costs alongside enhancements in staff satisfaction and a decrease in turnover rates over time.
Conclusion: PCTs assist RNs by performing fundamental nursing tasks, enhancing patient outcomes, increasing job satisfaction among RNs, and reducing turnover and overtime rates through effective teamwork.
Introduction
Nurses are crucial to the healthcare system and play a central role in delivering care. They advocate for health promotion, educate patients, provide care, assist in healing, participate in rehabilitation, and provide support (1). Despite being the largest provider group, there is a severe shortage of qualified registered nurses (RNs). Since the 1980s, the Saudi Arabian Ministry of Health has struggled with a persistent shortage of nursing staff, a problem that persists in today's healthcare workforce. This was also the case for a large tertiary military hospital. Patients, providers, organizations, and policymakers all have a role to play in making sure patients are healthy and safe. Thus, it is important to set up Patient Care Technician (PCT) services and a healthcare system that is not only efficient and effective but also safe and focused on patients and their families. Furthermore, the deployment of PCTs to alleviate the increasing workload burden of RNs is a strategy that deserves attention in the increasing number of developing countries. Although many studies in different work settings and countries have demonstrated a positive impact of the PCT model on nursing services and workload burden on regulated nursing professionals, only a few reports mention investigations that target additional, basic nursing-focused studies on the workload burden of RNs (1).
Acute care settings are experiencing a notable rise in critical staffing shortages, with more registered nurse (RN) positions projected to be available through 2022 than in any other profession in the United States (2). The demand for nursing exceeds the supply, necessitating alternative staffing models that incorporate unlicensed personnel and non-RN licensed positions to assist with patient care. These positions encompass licensed practical/vocational nurses (LPN/LVN), paramedics, and unlicensed assistive personnel (UAP) (3). UAPs encompass certified nursing assistant (CNA), nursing assistant, PCT, and nurse aide. The implementation of a layered staffing model enhances the dynamism of the healthcare environment, facilitating the registered nurse's role and contributing to improved patient outcomes. The American Nurses Association (ANA) emphasized the importance of employing competent, supervised nursing assistive personnel to provide high-quality, affordable healthcare (ANA, 2013 & 2022). A strong collaboration between RNs and UAPs was found to enhance patient satisfaction and improve various quality indicators, including falls, pressure ulcers, infection control, glycemic management, personal hygiene, infusion therapy, and communication (4-7). Several studies conducted in Saudi Arabia have demonstrated the positive influence of workforce interventions on nursing outcomes. Evidence indicates that reorganizing the workforce can improve the balance of nursing responsibilities and enhance patient satisfaction (8). Additionally, leadership support during staff restructuring has been shown to significantly reduce overtime rates (9). The significance of programs that instructed unlicensed personnel was underscored by their association with enhanced patient safety metrics and a decrease in adverse occurrences.
In order to address the shortage of nursing staff and to develop a potential workforce, healthcare facilities commonly use unlicensed assistive personnel, such as PCTs (4). By establishing entry-level positions and focusing on hiring and retaining these workers, resources can be allocated to developing the nursing pipeline (3). An analysis of the nursing workforce revealed that there was a decrease of over 100,000 RNs between 2020 and 2021. Additionally, in March 2023, the International Council of Nurses called for a worldwide health crisis to address the global shortage of nurses. There are many challenges faced by nurses in Saudi Arabia that significantly affect patient care and outcomes. The lack of nurses, the quick burnout of staff, and the adverse effects of overwork all make patient care worse (8). There are not enough qualified nurses because of cultural differences, too much dependence on foreign nurses, and not enough local schools (10). A common way to deal with staff shortages is to make people work overtime. Nurses who work long hours get tired both physically and mentally (11). These conditions not only affect general health but also make it harder to think clearly (8, 11, 12). From a patient care perspective, the adverse effects of overtime are significant. Fatigued nurses are less likely to engage in thorough patient assessments. This situation can lead to adverse events, compromising patient safety and care quality (11). The high-stress work environment, along with not enough staff and too much overtime, makes it more likely that nurses in Saudi Arabia will burn out. Burnout is characterized by emotional exhaustion, depersonalization, and a diminished sense of personal accomplishment (8, 12). It negatively impacts nurses' job performance, leading to decreased productivity and efficiency. Literature presents various strategies to alleviate these adverse events. These include increasing nurse support teams and nurse-to-patient ratios and implementing robust training programs to enhance the preparation of nurses for the demands of the job. Additionally, fostering a supportive work environment that prioritizes nurses' well-being can help reduce the incidence of burnout and its associated risks (1).
PCTs are healthcare providers who deliver basic nursing care under the supervision of RNs. Their practice reduces the work burden on RNs by saving time and effort, enables them to spend more direct and voluntary nursing time, increases professional satisfaction, and provides added value to safe and efficient patient care with the right resources (1, 13). PCTs' roles and responsibilities include facilitating daily patient care tasks, such as bathing, dressing, and toileting, including emptying a patient’s bladder; transporting, feeding, and assisting with repositioning; and assisting the nursing staff to monitor and record patients’ vital signs, such as blood pressure, temperature, pulse rate, and weight (13-15). The integration of PCT services aligns with theoretical frameworks such as the Quality-Caring Model. This model emphasizes the importance of caring relationships in healthcare. PCTs, through their supportive role, foster these relationships. Moreover, PCT services align with the Institute of Medicine's recommendations for patient-centered care. These recommendations point out the importance of considering patients' needs, preferences, and values in care delivery. Moreover, PCT services contribute to patient and family satisfaction. They provide personalized care that meets the unique needs of each patient. They alleviate the workload of nurses, allowing them to focus on complex patient needs, and play a crucial role in realizing this vision and addressing quality improvement priorities
This improvement project aimed to establish a structured assessment that would determine the readiness of new PCT staff to function independently in providing patient care. The objectives were to provide PCT support to help the RN in providing efficient and competent patient care in both ambulatory and inpatient settings, as well as assisting the RN and team members in achieving the greatest healthcare outcomes for the individuals in need of care.
Methods
Context
The improvement project was founded on the principles of the Institute for Healthcare Improvement (IHI) model of improvement. Recently, nurses have expressed that a significant portion of their time is spent on low-value tasks related to basic patient care, rather than on leveraging their advanced nursing skills. The autonomy model of nursing care emphasizes enhancing group capacity by establishing clear objectives and fostering a trusting work environment. The nursing department decided to redefine basic nursing care and recruited PCTs to perform essential nursing care duties. The emphasis was on delivering safe, affordable, and efficient healthcare services.
Project Design and Approach
The project was executed in stages using the intervention improvement approach: preplanning, planning, action, evaluation, and analysis. By July 2023, the program was entirely operational, having been initiated in November 2022. The pre-planning phase of the model commences in November and December 2022. Team members are adequately equipped for project and program work during this phase. The development of pedagogical and training materials, as well as the pursuit of project mentors, marked the commencement of model planning in January 2023. The intervention phase progressed rapidly, which allowed for the timely evaluation of its early outcomes (Figure 1). The service content was incorporated into clinical nursing practice after analyzing implementation and incorporating healthcare team comments, which demonstrated an improved satisfaction rate. It is advantageous to commence with fundamental nursing care administration and ensure continuity of care delivery. Head Nurses, Assistant Head Nurses, Charge Nurses, and unit preceptors will be required to conduct extensive evaluations of performance outcomes, in addition to first-line Continuous Nurse Educators and Clinical Resource Nurses. These roles were chosen for their direct oversight of patient care delivery and experience in frontline training. To satisfy future training requirements, a flow diagram must demonstrate the program's advancement and designate the valued service level enhancement from the current condition.

Figure 1: PCT Timeline Chart
Intervention
The hospital policy was established following the committee meeting, during which the nursing leadership provided the necessary sanction. Additionally, the new certified PCT role was authorized for the pilot phase. As part of this phase, the Certified PCT was scheduled to participate in a PCT Orientation Program, a Hospital-Wide Staff Orientation, and a unit orientation. During these sessions, they received both theoretical and practical training. The introduction was conducted in accordance with the hospital's policies. The creation of a simulation area featuring high-fidelity, state-of-the-art mannequins has facilitated hands-on training, allowing students to practice their diverse nursing skills and evaluate their competency in a controlled and simulated environment with the assistance and guidance of their clinical preceptors and clinical resource nurse. PCTs are assigned complete responsibility for a variety of patient care responsibilities, including activities of daily living, vital sign measurement, blood pressure monitoring, sample collection (including urinary catheterization), oral hygiene, cardiology chair, lab runner, mobilization, and walking assistance, based on their passion and skills. They were prohibited from administering direct care to patients with central lines or nasogastric tubes, monitoring telemetry, or dispensing medications. Training encompassed infection control, hazardous material management, major disaster response, facility management safety, and various types of hospitals, as well as standard precautions. These skills were acquired through training and orientation, which equipped them with the necessary confidence and competence to ensure a successful hospital entry.
One of the numerous interventions to preserve the quality of work and alleviate the workload is the development of curricula and the establishment of a service for PCT. To facilitate the provision of high-quality care and the acquisition of new skills during their employment, PCT training programs must be established. The principles that skills must be job-related and learning must be continuous should be the primary focus of operating policies. A critical resource capable of performing clinically and economically significant practical nursing duties in the healthcare industry will be established by increasing the number of current certification and training programs for PCTs. Hospitals should provide support for the implementation of formal internal training, which should include evidence-based training that addresses critical factors that influence a secure work environment, and PCTs will collectively acquire all the necessary skills. Formal training culminating in certification facilitates comprehension of the significance of pathophysiological responses to alterations in the conditions of patients undergoing acute care.
Today, the role of PCT should be viewed as a platform to showcase one's capacity to manage various situations, alongside the conventional focus on personal care and support.
PCTs are responsible for the provision of fundamental care, including cleansing patients, changing linens, taking vital signs, assisting with exercise, and conducting all the tasks required for patients to achieve full recovery. The effective integration of PCTs within the nursing team alleviates the workload of RNs by ensuring the completion of patients' essential activities of daily living (ADLs). The entry-level nursing role of PCTs may facilitate opportunities for further qualifications, as PCTs acquire knowledge and experience in primary nursing tasks. The person-centered model of PCT enables participants to achieve their nursing goals and aspirations. Standards must be regularly reviewed and adjusted to align with the requirements of the clinical area through systematic benchmarking and data evaluations. Standard measurements are crucial as they facilitate enhancement through the provision of quantifiable metrics. The responsibilities and requirements of the clinical area are ensured to be effectively aligned with teaching, training, and development. Consequently, it was implemented in the performance quality department and the program dashboard to achieve significant outcomes.
The project team was formed after conducting a comprehensive stakeholder analysis. The stakeholder analysis assists the project in identifying the key individuals who can significantly impact its success or failure. Members of the human resources department were instrumental in the creation of the new position and the recruitment of the most appropriate candidates. The nursing education and nursing excellence members were instrumental in ensuring the project met international and national education standards and complied with the national laws.
Study of the intervention(s)
The project assessment commenced with a baseline data analysis of staff attrition and overtime for the year 2022. This analysis served as a reference point for comparison, enabling us to determine whether the observed outcomes were a result of the intervention. The interventions' progress was optimized by utilizing the insights obtained from the descriptive analyses. The project's impact was evaluated through a comparison of outcome data to the baseline and a pre- and post-intervention analysis.
Measures
Primary Outcome: To decrease the average monthly registered nursing overtime by 5% from the baseline by the end of June 2024.
Secondary Outcome: To lower the turnover rates of RNs, lessen burnout, and enhance staff satisfaction.
Quantitative data were collected through the nursing human resources and finance databases. Staff perceptions were measured through satisfaction surveys. Numeric variables were published in table, run chart, and control chart formats. Measures chosen for studying processes and outcomes of the intervention(s), including rationale for choosing them, their operational definitions, and their validity and reliability. Description of the approach to the ongoing assessment of contextual elements that contributed to the success, failure, efficiency, and cost. Methods employed for assessing completeness and accuracy of data (Table 1).
|
Table 1. Methods employed for assessing the completeness and accuracy of data, including project measures and data quality |
|||||
|
Measure type |
Measure |
Definition/unit |
Data source |
Collection method & frequency |
Data Quality Check |
|
Outcome |
Monthly overtime hours |
Total overtime hours worked by nursing staff per calendar month |
Electronic rostering/payroll system |
Monthly extract by Nursing Administration in collaboration with HR/payroll |
Cross-check that all nursing cost centres are included; missing months or units queried with HR; compare monthly total to previous month to identify outliers Reconciliation against HR/payroll summary reports; random spot-check of unit-level overtime against original duty rosters |
|
Outcome |
Nursing staff turnover rate |
Monthly turnover (%) = number of nursing staff separations in month ÷ average monthly nursing headcount × 100 |
HR information system |
Monthly report generated by HR and shared with Nursing Administration |
Verify that all separations (resignations, terminations, transfers out) are included; check that headcount is non-missing for all months Cross-check against HR master headcount reports; confirm any extreme changes with the HR business partner |
|
Outcome |
Nursing staff satisfaction rates |
Mean RN satisfaction scores (overall and by domain) from the annual RN survey |
Standardised RN satisfaction survey (external vendor) |
Annual online/ paper survey; hospital-level and domain-level scores obtained from the vendor |
Compare the number of RN respondents with the eligible RN population to estimate the response rate, and check for missing domains or scales Vendor automated range and consistency checks; internal review of outliers; where feasible, duplicate export compared with vendor summary reports |
|
Process |
Number of PCTs per unit |
Count of active PCT posts per clinical unit on the last day of each month |
HR payroll/staffing establishment list |
Monthly snapshot taken on the last day of each month |
Compare unit-level counts with the previous month; resolve discrepancies with unit managers Cross-check against approved establishments and active contracts; verify a random sample of names against unit rosters |
|
Process |
Number of PCTs hired per month and year |
Count of newly appointed PCTs whose employment commences in the given month/year |
HR recruitment records |
Monthly extraction of new PCT appointments |
Compare the monthly total with the recruitment log; confirm that start dates fall within the reporting period Spot-check appointment records against signed employment contracts/offer letters |
|
Process |
Number of PCTs who completed mandatory training during probation |
Count and % of newly hired PCTs who completed all mandatory modules within probationary period |
Learning management system / Education records |
Quarterly report from the Education Department |
Ensure all new PCT hires for the period are included, and cross-check the list against the HR hire list Verify completion dates and module list against training records; random audit of certificates in personnel files |
|
Balancing |
PCT competence survey results |
Mean scores for knowledge, skills, and attitude domains from the PCT self-assessment survey |
Locally designed PCT competence survey |
Administered to all PCTs after orientation / during follow-up; data entered onto spreadsheet |
Check the number of responses against PCT headcount; identify missing items and incomplete surveys; apply predefined rules for handling missing data Double data entry or verification of a sample of records; logical checks (e.g., valid response range 1–5); review of extreme values with unit educators |
Study Setting and Participants
This enhancement initiative was implemented at King Fahad Armed Forces Hospital, a significant tertiary military healthcare institution, in a variety of inpatient and ambulatory care facilities. The facility is affiliated with the Ministry of Defense Health Service division and accepts referrals from the Mecca region. The ratio of PCTs is contingent upon the number of technicians employed on the unit, with one to three technicians typically working a shift. In the inpatient department, a minimum of 10-15 RNs and 1-3 registered practical nurses are employed on a shift basis. From November 11, 2022, to the present, 93 PCTs are employed in the inpatient, outpatient, and emergency departments, comprising 7.5% of the hospital's total healthcare providers. Their distribution across units is illustrated in Table 2. Of these, 77 are female, and 16 are male. The SCFHS license is held by all PCT personnel. The professional qualifications and PCT tasks are diverse, encompassing a variety of activities, including the cleansing of patient facilities, as well as the maintenance of environmental and medical apparatus. They are responsible for a variety of tasks, such as assisting with activities of daily living, conducting hourly visits, preventing pressure ulcers and accidents, transporting patients, documenting vital signs, and conveying specimens and blood products.
Data Collection
Data was obtained in two phases: the initial phase compared the underlying distribution of core patient care responsibilities with the distribution of nursing technician skills and examined trends in RN turnover and overtime. In the second segment, a questionnaire was administered to gather assessments of PCT skills. The primary goal of the survey questionnaire was to evaluate the requirements of PCTs to effectively fulfill the necessary duties and responsibilities at their new workplace. The questionnaire was distributed online through Google Forms.
|
Table 2. Distribution Of PCTs per Units/ Departments |
||
|
Category |
# of PCT |
Units/ Departments |
|
Cardiac Services |
3 |
Cardiac Surgical Intensive Care Unit |
|
1 |
Pediatric Cardiac Intensive Care Unit |
|
|
1 |
Cardiac Ward |
|
|
0 |
Cardiac Operating Room (COR) |
|
|
0 |
Cardiac Catheterization Laboratory (CCL) |
|
|
Surgical Services |
9 |
Surgical Ward 1 & 2 |
|
2 |
Day Surgery Unit |
|
|
3 |
Radiology Department |
|
|
4 |
Endoscopy Unit |
|
|
0 |
Operating Room / Recovery Room (OR/RR) |
|
|
Medical Services |
8 |
Medical Ward 1 |
|
8 |
Medical Ward 2 |
|
|
4 |
Medical Ward 3 |
|
|
1 |
Medical Day Unit (Oncology) |
|
|
2 |
VIP / Royal Patient Suite |
|
|
Renal Services |
6 |
Renal Transplant Unit / Hemodialysis & Nephrology Clinic (RTU/HD) |
|
Maternal & Child Services |
0 |
Pediatrics Clinic |
|
6 |
Pediatric Ward & Pediatric Oncology |
|
|
0 |
Pediatric ICU |
|
|
5 |
Well Baby Nursery (WBN) |
|
|
0 |
Neonatal Intensive Care Unit (NICU) |
|
|
3 |
Obstetric Ward 1 |
|
|
3 |
Obstetric Ward 2 |
|
|
0 |
Labor and Delivery (L&D) |
|
|
3 |
Obstetrics Clinic (OB) |
|
|
Critical Services |
3 |
Emergency Department (ED) |
|
4 |
Intensive Care Unit (ICU) |
|
|
Ambulatory Services |
1 |
Home Health Care (HHC) |
|
4 |
Family Medicine Department (FMD) |
|
|
6 |
Hospital Specialty Clinic (HSC) |
|
|
0 |
Dermatology Clinic |
|
|
1 |
Endocrine Clinic |
|
|
Satellite Clinics |
0 |
Preventive Medicine (PM) |
|
1 |
Ground Forces Clinic |
|
|
0 |
Air Defense Institute Clinic |
|
|
1 |
Royal Saudi Air Force Clinic |
|
|
0 |
Naval Base Clinic |
|
|
0 |
Al Manar Clinic |
|
Analysis
The numeric variables were analyzed using a quantitative methodology. Microsoft Excel data analytics add-in packages were used to perform a descriptive quantitative data analysis. Qualitative and quantitative methods are used to draw inferences from the data. Data was plotted on tables and graphs in percentages and numbers to provide a visualization of the variables and to track the progress of the interventions.
Ethical considerations
The initiative was authorized by the hospital director. The Ministry of Defense, Health Service Division (MODHS) nursing executive branch endorses the employment of patient care assistants. All data collection and analysis procedures were conducted in accordance with ethical standards, thereby guaranteeing the integrity of the data and the confidential treatment of patients.
Results
Outcome Measures
Monthly RN overtime decreased progressively over the project period as PCTs were recruited, trained, and deployed. Monthly RN overtime hours showed a sustained reduction following PCT implementation. On the overtime X chart (Figure 2), several points in 2024 fell below the previous lower control limit, indicating a genuine process shift and associated cost savings. Expected seasonal variation, with temporary peaks in March–May coincided with Ramadan and preferred vacation periods, but no sustained increase in overtime. Overtime use was higher in the first and second quarters of 2023, when few PCTs had yet been hired, and then declined and stabilized as PCT recruitment accelerated from the third quarter of 2023 through the first quarter of 2024.
Using RN overtime as a proxy for cost, and assuming an hourly salary of 31.46 Saudi riyals, mean monthly overtime decreased from 41 951 hours during the recruitment and pilot phases (November 2022–June 2023) to 37 976 hours during the hospital-wide adoption phase (January–July 2024), an absolute reduction of 3 975 hours per month (approximately 9.5%). This corresponded to an avoided overtime cost of about 125,054 SAR per month and an estimated 875,375 SAR over the 7-month adoption period. If sustained for 12 months, the projected annual overtime cost avoidance would be approximately 1.5 million SAR.
Monthly RN turnover was monitored using individuals and moving-range (I–MR) control charts from November 2022 to June 2024. The X chart (Figure 3) showed turnover fluctuating around a centreline of 0.90% (UCL 1.64%, LCL 0.15%), with a single special-cause point in December 2022 (1.7%) above the upper control limit; all subsequent points lay within the control limits. From the period of formalizing PCT training onwards, monthly turnover ranged from 0.3% to 1.1%, with most values at or below the centreline, indicating no deterioration and a small improvement in average turnover as the PCT model was implemented and spread.
The MR chart (Figure 4) showed small month-to-month changes in turnover (moving range 0–0.9 percentage points), with all values within the moving-range limits (CLmr 0.28, UCLmr 0.91). This pattern is consistent with common-cause variation over time and suggests that PCT implementation did not introduce additional instability into the nursing workforce.
RN satisfaction (Table 3) improved over the same period that the PCT role was introduced, piloted, and adopted, with no evidence of any adverse effect. The overall mean satisfaction score rose from 3.95 in 2022 (pre-implementation/early recruitment) to 4.13 in 2024 (post-hospital-wide adoption), with most of the gain between 2022 and 2023. Domains likely to reflect PCT support showed clear improvement, including Tasks (4.22 to 4.52), Staffing and resource adequacy (2.41 to 2.70), and Nursing foundations for quality of care (2.95 to 3.06), alongside gains in decision making, professional status, and nursing administration. Although some domains, such as RN–RN interactions and opportunities for professional development, changed little and remained below external benchmarks, the overall pattern suggests that introducing PCTs was associated with maintained or modestly improved RN satisfaction, recognizing that other organizational initiatives occurred in parallel.
|
Table 3. National Database of Nursing Quality Indicators Job Satisfaction Scales |
||||||
|
2022 |
2023 |
2024 |
||||
|
Individual Measure or Domains for RN satisfaction survey |
Hospital Rate |
Non-Magnet Hospital Mean |
Hospital Rate |
Non-Magnet Hospital Mean |
Hospital Rate |
Non-Magnet Hospital Mean |
|
Measure 1: Tasks |
4.22 |
4.41 |
4.45 |
4.40 |
4.52 |
4.58 |
|
Measure 2: RN-RN Interactions |
4.84 |
5.18 |
4.80 |
5.25 |
4.81 |
5.21 |
|
Measure 3: RN-MD Interaction |
4.30 |
4.67 |
4.37 |
4.63 |
4.48 |
4.67 |
|
Measure 4: Decision Making |
3.92 |
3.67 |
4.18 |
3.58 |
4.18 |
3.78 |
|
Measure 5: Autonomy |
4.40 |
4.47 |
4.57 |
4.59 |
4.61 |
4.65 |
|
Measure 6: Professional Status |
4.23 |
4.39 |
4.45 |
4.40 |
4.49 |
4.56 |
|
Measure 7: Pay |
3.38 |
3.09 |
3.81 |
2.90 |
3.72 |
3.33 |
|
Measure 8: Professional Development Opportunity |
4.11 |
4.49 |
4.25 |
4.62 |
4.30 |
4.64 |
|
Measure 9: Professional Development Access |
4.34 |
4.44 |
4.38 |
4.53 |
4.53 |
4.57 |
|
Measure 10: Nursing Management |
4.61 |
4.87 |
4.64 |
4.83 |
4.64 |
4.83 |
|
Measure 11: Nursing Administration |
4.28 |
3.75 |
4.33 |
3.63 |
4.34 |
3.86 |
|
Measure 12: Staffing and Resource Adequacy |
2.41 |
2.65 |
2.66 |
2.82 |
2.70 |
2.91 |
|
Measure 13: Nursing Foundations for Quality of Care |
2.95 |
3.08 |
3.00 |
3.13 |
3.06 |
3.17 |
|
Measure 14: Interprofessional Scale-Rollup |
3.37 |
4.01 |
3.45 |
4.07 |
3.48 |
4.05 |
|
Mean |
3.95 |
4.08 |
4.10 |
4.10 |
4.13 |
4.20 |

Figure 2: X chart of monthly RN overtime utilisation post-PCT implementation

Figure 3: Turnover rate – X chart (individuals)
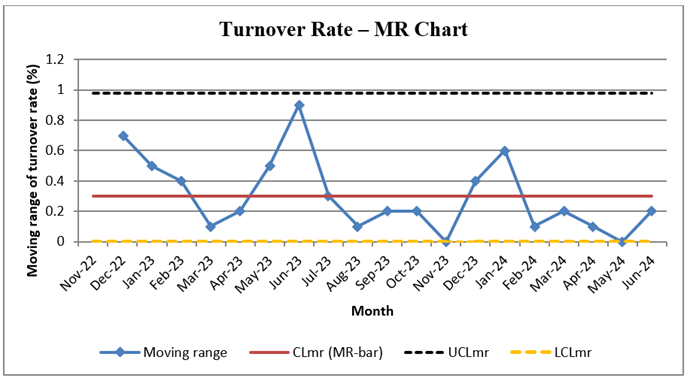
Figure 4: Turnover rate – MR chart (moving range)
Process measures
Monthly PCT hiring trends from 2022 to 2024. (Table 4) showed a progressive increase in recruitment, with a marked ramp-up from the third quarter of 2023 onwards. Expansion of the PCT workforce was associated with a modest reduction in RN overtime. Across the 20 months, overtime ranged from 33 774 to 47 159 hours (mean approximately 39 800 hours per month) and decreased stepwise across project phases: from 43 455 hours per month during the recruitment phase, to 41 450 hours during the pilot PCT orientation programme, 39 125 hours during formalization of PCT training and orientation, and 37 976 hours after hospital-wide adoption of PCT training, despite concurrent growth in overall nursing headcount. Correlation analysis demonstrated a weak negative association between the number of PCTs employed and overtime use (Pearson r ≈ –0.23), and simple linear regression suggested an average reduction of about 180 overtime hours for each additional PCT.
|
Table 4. Monthly recruitment of patient care technicians, November 2022–July 2024 |
|
|
Month/year |
# of PCT Staff recruited |
|
Nov-22 |
15 |
|
Dec-22 |
1 |
|
Jan-23 |
1 |
|
Feb-23 |
2 |
|
Mar-23 |
0 |
|
Apr-23 |
0 |
|
May-23 |
0 |
|
Jun-23 |
0 |
|
Jul-23 |
0 |
|
Aug-23 |
0 |
|
Sep-23 |
1 |
|
Oct-23 |
12 |
|
Nov-23 |
8 |
|
Dec-23 |
10 |
|
Jan-24 |
7 |
|
Feb-24 |
14 |
|
Mar-24 |
6 |
|
Apr-24 |
2 |
|
May-24 |
7 |
|
Jun-24 |
3 |
|
Jul-24 |
4 |
Balancing measures
Most PCTs reported high readiness and confidence to function independently in providing patient care (Table 5). Overall, 89.4% of respondents agreed or strongly agreed with the readiness statements (10.9% agree, 78.5% strongly agree), while only 5.6% disagreed or strongly disagreed, and 4.2% were neutral. Strongly agree responses were highest for Attitude (80.0%), followed by Knowledge (78.1%) and Skills (77.3%). Disagreement was low in all domains (Knowledge 5.0%, Skills 5.4%, Attitude 4.9%), indicating that only a small minority of PCT staff felt unsure or unprepared in relation to their roles, skills or professional attitude.
|
Table 5. Patient care technicians’ self-reported readiness to function independently in patient care (%) |
||||||
|
Domain |
Item |
Strongly disagree |
Disagree |
Neutral |
Agree |
Strongly agree |
|
Knowledge |
I know my roles and responsibilities as per my job description. |
4.6 |
0 |
3.1 |
12.3 |
80 |
|
I understand my scope of practice. |
4.6 |
0 |
3.1 |
16.9 |
75.4 |
|
|
I am aware of the basic skills needed to provide high-quality care in clinical areas. |
6.2 |
0 |
3.1 |
7.7 |
83.1 |
|
|
I am aware of hospital policies, procedures and guidelines, including infection control and safety standards. |
4.6 |
0 |
7.7 |
12.3 |
73.8 |
|
|
Skills |
I take responsibility for orienting my patient. |
4.6 |
1.5 |
4.6 |
7.7 |
81.5 |
|
I am confident in performing my duties and responsibilities. |
6.2 |
0 |
4.6 |
1.5 |
87.7 |
|
|
I am able to complete assigned hours, including overtime, weekends, nights, holidays and any shift. |
4.6 |
1.5 |
12.3 |
10.9 |
64.6 |
|
|
I assist in the daily functioning of the unit/department in support of patient care. |
4.6 |
0 |
0 |
10.8 |
83.1 |
|
|
I provide direct assistance to patients in meeting their personal hygiene needs (e.g. bathing/showering, dressing, toileting, oral hygiene). |
6.2 |
0 |
3.1 |
16.9 |
73.8 |
|
|
Attitude |
I report to work on time. |
4.6 |
1.5 |
12.3 |
16.9 |
64.6 |
|
I am cooperative and willing to perform delegated tasks within my ability. |
6.2 |
0 |
0 |
10.8 |
83.1 |
|
|
I am approachable and respect patients’ rights. |
6.2 |
0 |
3.1 |
16.9 |
73.8 |
|
|
I support and apply organisational values in providing quality patient care. |
4.6 |
1.5 |
0 |
6.2 |
87.7 |
|
|
I contribute to the delivery of safe, patient- and family-focused quality care. |
3.1 |
3.1 |
1.5 |
1.5 |
90.8 |
|
|
Mean |
5.1 |
0.5 |
4.2 |
10.9 |
78.5 |
|
Discussion
Summary of findings
The project exceeded its primary objective of reducing the monthly extra hours performed by RNs. Mean monthly overtime fell by 9.5%, representing a 4.5-percentage-point improvement over the initial 5% target. This outcome demonstrates the efficacy of PCTs in inpatient, outpatient, and emergency department environments. PCTs assisted RNs in delivering superior patient care more efficiently and with reduced stress by assuming fundamental care responsibilities. The principal concepts of health services administration were employed, particularly those emphasizing the enhancement of safety, quality, and equity in care delivery. Establishing a workforce structure that facilitates collaboration between RNs and unlicensed auxiliaries to enhance patient outcomes was facilitated by the administrative framework of a PCT service. Nurse leaders must be equipped with the necessary skills and frameworks to implement these employment models in order to enhance performance and reduce operational inefficiencies. Studies in both clinical and social disciplines have demonstrated that the transition to PCTs is a direct response to the persistent shortage of nurses in the United States (16). Initiatives that unite companies and educational institutions to emphasize organized PCT recruitment and training have been effective, highlighting the significance of a workforce equipped with diverse skills. This initiative represents a significant shift in healthcare delivery, transitioning from hospital-centered models to patient-centered approaches. PCTs are indispensable in this transformation, as they guarantee that patients' fundamental requirements are consistently met, thereby improving their overall satisfaction, trust, and comfort. They assess vital signs, maintain hygiene standards, and facilitate mobility. This initiative enhances the significance of RNs and increases total patient engagement (17). Historically, hospitals with inadequate staffing levels have adversely impacted the quality of primary care and patient experiences. The project addressed this issue by monitoring not only the improvement in RNs' workloads but also the assistance provided by other staff members in delivering care (18). The findings underscore the need to align staffing strategies with patient requirements and provider capabilities. Formally implementing these approaches may enhance care outcomes and maintain workforce stability in healthcare facilities facing similar challenges.
Interpretation
The results of this research are consistent with data from around the world, which suggests that the addition of unlicensed assistive staff, such as PCTs, may alleviate the shortage of nurses, reduce the burden on RNs, and enhance the quality of treatment. The monthly overtime of RNs decreased by 9.5% when the Hospital began providing PCT services, resulting in substantial cost savings. This demonstrates that the model is beneficial for resolving personnel issues and optimizing operations. This demonstrates that the model is beneficial for resolving personnel issues and optimizing operations. The transition time for clinical professionals and the limited task authorization of PCTs resulted in delays in addressing patient needs during the early implementation phase. Nonetheless, team members saw these problems as opportunities for collective development. Feedback highlighted the need for clearly defined roles and targeted training to promote integration and guarantee the safe transfer of responsibilities. Scott et al. (2018) and Macy (2022) have previously demonstrated that the appropriate utilization of supportive workers can improve patient satisfaction and increase safety in care settings (19, 20). This aligns with prior findings. Nevertheless, the findings also demonstrate the critical nature of robust orientation programs, systematic monitoring, and open communication among various teams in order to maintain a high level of service quality. The results of this project are aligned with those of previous studies conducted in Saudi Arabia. In 2020, Alluhidan et al. demonstrated that the strategic utilization of support staff, as well as targeted modifications to the workforce, resulted in enhanced care quality and a reduction in nursing fatigue (8). Alsadaan et al. (2021) discovered that the provision of support roles, such as nursing auxiliaries, to RNs to alleviate their burden resulted in increased job satisfaction and decreased turnover intentions (10). Our project findings support this conclusion. The establishment of structured induction programs and executive involvement in role redesign led to a quantifiable decrease in overtime costs, as emphasized by Alruwaili et al. (2023) (9). This finding is similar to the 9.5% reduction in RN overtime that was observed. Alreshidi et al. (2024) conducted research that demonstrated the incorporation of unlicensed assistance personnel in emergency departments to improve treatment efficacy while ensuring patient safety (21). This study illustrates the safety and efficacy of our PCT methodology. Alghamdi et al. (2024) found that when RNs were given basic tasks to handle, they could focus more on important clinical duties (22). This study is consistent with our discovery that PCTs improve the quality of care delivered by RNs. The local results support the applicability of our intervention model within Saudi Arabia's healthcare system. The integration of PCTs effectively addresses chronic nursing shortages, improves patient care outcomes, and contributes to a more sustainable workforce. Institutions must commit to treating all individuals fairly and collaborating in order to effectively implement the PCT model over time. Examining the costs and experiences of PCTs, RNs, and Primary Nurses may assist in the development of more effective workforce plans and the enhancement of team-based care. This initiative gathers task-specific labor data and examines cost reductions to establish a framework for making personnel decisions based on evidence. This information is also crucial for the development of strategies for the recruitment and retention of personnel in Saudi hospitals.
Implications for Practice and Policy
A highly effective approach to address the shortage of personnel and prevent RNs from experiencing burnout is the integration of PCTs into nursing teams. Patients are assigned straightforward duties by PCTs, which allows qualified nurses to concentrate on more complex clinical responsibilities. It enhances the efficacy of care and contributes to improved nurse satisfaction in their responsibilities. Organized training and competency-based orientation programs must be prioritized by institutions to ensure that all employees comprehend their responsibilities and that tasks are securely transferred. Healthcare sector policymakers should promote long-term employment models that incorporate support personnel. This process involves the development of precise job descriptions, the sponsorship of standardized training, and the collaboration between RNs and PCTs. Future research must investigate the scalability of the PCT approach by analyzing patient-reported outcomes and treatment quality in various healthcare settings. Healthcare systems may enhance the delivery of care and mitigate the effects of nurse shortages by promoting team-based care and ensuring that employment plans are consistent with recognized best practices.
Limitations
This investigation employed a pre-test–post-test design that was implemented in a single hospital, thereby limiting the generalizability of the results to other healthcare environments. The results should be interpreted with caution due to the utilization of a convenience sample and a sample size that is not particularly substantial. Additionally, determining whether the intervention was responsible for the changes is more challenging due to the absence of a control group. The results may have been affected by confounding variables, such as differences within departments, changes in the availability of staff, and outside factors that impact overtime patterns. To improve the validity of results and get a thorough understanding of the efficacy of PCT integration, further research should use more rigorous study designs, including randomized or multicenter trials.
Conclusions
This project demonstrated that the integration of trained, non-licensed professionals, such as PCTs, into nursing teams can effectively address personnel shortages while ensuring high-quality care and lowering costs. The collaboration between PCTs and RNs significantly improved the workplace environment and increased overall employee satisfaction. The findings support the adoption of the PCT model as a strategic method to tackle both global and localized nursing shortages. Comprehensive educational programs and competency-based exams will standardize PCT training and clarify tasks, relieving the RN and increasing patient care. This secures task distribution and clarifies PCT obligations. Hospital managers should use shared decision-making and team-based care to improve nurse-technologist communication and trust. Encourage cross-disciplinary collaboration.
Disclosure
Conflict of interest
There is no conflict of interest.
Funding
No funding.
Ethical consideration
All data collection and analysis procedures were conducted in accordance with ethical standards, thereby guaranteeing the integrity of the data and the confidential treatment of patients.
Data availability
Data that support the findings of this study are embedded within the manuscript.
Author contribution
All authors contributed to conceptualizing, data drafting, collection and final writing of the manuscript.
Acknowledgement
We want to express our deep appreciation to the Head Nurses, Assistant Head Nurses, Charge Nurses, Clinical Resource Nurses, and Unit preceptors. Special appreciation to Ms. Samah Jaha, Acting Director, Nursing Education, Mr Erwin, Bolante, and Ms. Amani Tunusi, Nursing Excellence representatives. The project's achievements would not have been possible without their commitment.
